A New Era in Corneal Transplantation: Paradigm Shift and Evolution Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ethical, Legal and Psychosocial Aspects of Transplantation Global Challenges
E. K. Massey, F. Ambagtsheer, W. Weimar (Eds.) Ethical, Legal and Psychosocial Aspects of Transplantation Global Challenges PABST E. K. Massey, F. Ambagtsheer, W. Weimar (Eds.) Ethical, Legal and Psychosocial Aspects of Transplantation Global Challenges PABST SCIENCE PUBLISHERS Lengerich Bibliographic information published by Die Deutsche Nationalbibliothek Die Deutsche Nationalbibliothek lists this publication in the Deutsche Nationalbibliografie; detailed bibliographic data is available in the Internet at <http://dnb.ddb.de>. This work is subject to copyright. All rights are reserved, whether the whole or part of the mate- rial is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in other ways, and storage in data banks. The use of registered names, trademarks, etc. in this publication does not imply, even in the absence of a spe- cific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The authors and the publisher of this volume have taken care that the information and recommen- dations contained herein are accurate and compatible with the standards generally accepted at the time of publication. Nevertheless, it is difficult to ensure that all the information given is entirely accurate for all circumstances. The publisher disclaims any liability, loss, or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents of this volume. © 2017 Pabst Science Publishers · D-49525 Lengerich Internet: www.pabst-publishers.de, www.pabst-science-publishers.com E-mail: [email protected] Print: ISBN 978-3-95853-292-2 eBook: ISBN 978-3-95853-293-9 (www.ciando.com) Formatting: µ Printed in Germany by KM-Druck, D-64823 Gross-Umstadt Contents Preface Introduction Emma K. -

Medical Policy
Medical Policy Joint Medical Policies are a source for BCBSM and BCN medical policy information only. These documents are not to be used to determine benefits or reimbursement. Please reference the appropriate certificate or contract for benefit information. This policy may be updated and is therefore subject to change. *Current Policy Effective Date: 5/1/21 (See policy history boxes for previous effective dates) Title: Composite Tissue Allotransplantation Description/Background Composite tissue allotransplantation refers to the transplantation of histologically different tissue that may include skin, connective tissue, blood vessels, muscle, bone, and nerve tissue. The procedure is also known as reconstructive transplantation. To date, primary applications of this type of transplantation have been of the hand and face (partial and full), although there are also reported cases of several other composite tissue allotransplantations, including that of the larynx, knee, and abdominal wall. The first successful partial face transplant was performed in France in 2005, and the first complete facial transplant was performed in Spain in 2010. In the United States, the first facial transplant was done in 2008 at the Cleveland Clinic; this was a near-total face transplant and included the midface, nose, and bone. The first hand transplant with short-term success occurred in 1998 in France. However, the patient failed to follow the immunosuppressive regimen, which led to graft failure and removal of the hand 29 months after transplantation. The -

Four Cases of Corneal Perforation in Patients with Chronic Graft- Versus-Host Disease
Molecular Vision 2011; 17:598-606 <http://www.molvis.org/molvis/v17/a68> © 2011 Molecular Vision Received 21 October 2010 | Accepted 15 February 2011 | Published 25 February 2011 Four cases of corneal perforation in patients with chronic graft- versus-host disease Emi Inagaki, Yoko Ogawa, Yukihiro Matsumoto, Tetsuya Kawakita, Shigeto Shimmura, Kazuo Tsubota Department of Ophthalmology, Keio University School of Medicine, Tokyo, Japan Purpose: To report the clinical features and investigate the underlying pathological processes of spontaneous corneal perforation in patients with ocular chronic graft-versus-host disease (cGVHD). Methods: A full ophthalmological evaluation of corneal perforation in four patients with cGVHD was performed. Three of them underwent deep anterior lamellar keratoplasty and samples from two of three patients were used for histopathological analyses. Results: Three patients were successfully treated by corneal transplantation. One patient was treated with a therapeutic soft contact lens, and the wound healed within 2 days. The common clinical features of these patients were (1) the presence of definite dry eye related to cGVHD in 3 of 4 patients and probable dry eye in one patient, (2) a central or paracentral site of corneal ulceration and perforation, with no sign of infection, and (3) prior use of a topical or systemic corticosteroid, and/or topical non-steroidal anti-inflammatory drugs. Immunohistochemical findings revealed an increased number of cluster of differentiation 68+ (CD68+) macrophages and matrix metalloproteinase 9 (MMP-9) expression in the tissue surrounding the perforation. Conclusions: Our report extends current information on the clinical features and pathological processes of corneal perforation in cGVHD by showing increased MMP-9 expression and the accumulation of CD68+ positive macrophages in the affected areas. -

Costal Cartilage Graft in Asian Rhinoplasty: Surgical Techniques Sarina Rajbhandari and Chuan-Hsiang Kao
Chapter Costal Cartilage Graft in Asian Rhinoplasty: Surgical Techniques Sarina Rajbhandari and Chuan-Hsiang Kao Abstract Asian rhinoplasty is one of the most difficult and challenging surgeries in facial plastic surgery. As many Asians desire a higher nasal bridge and a refined nasal tip, they undergo various augmentation procedures such as artificial implant grafting and filler injections. Autologous rib graft is a very versatile graft material that can be used to augment the nose, with lesser complications, if done precisely. In this chapter, we have discussed the steps of rib graft harvesting, carving and setting into the nose to form a new dorsal height. Keywords: rhinoplasty, costal cartilage, Asians, warping 1. Introduction Asian rhinoplasty is one of the most difficult and challenging surgeries in facial plastic surgery. In Asians, the most common complaints regarding appearance of the nose are a low dorsum and an unrefined tip. Thus, most Asian rhinoplasties include augmentation of the nasal dorsum using either autologous or artificial implant, and/or nasal tip surgery. Clients who have had augmentation rhinoplasty previously frequently opt for revision. Hence, when a client comes for augmenta- tion or Asian rhinoplasty, the surgeon has to confirm whether the client has had any rhinoplasty (or several rhinoplasties) earlier. Artificial nasal implants for augmentation are still in vogue, owing to their simplicity and efficiency, but they are accompanied by several major and minor complications. Revision surgeries for these complications include correcting nasal contour deformities and fix functional problems, and require a considerable amount of cartilage. Revision surgeries are more complex than primary Asian rhinoplasty as they require intricate reconstruc- tion and the framework might be deficient. -
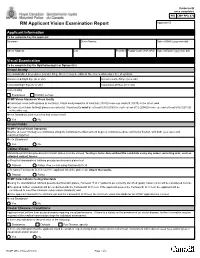
RCMP GRC 2180E (2017-10) Page 1 of 2 Protected B RM Applicant Vision Examination Report Once Completed Applicant ID
Protected B once completed PIB CMP PPU 070 RM Applicant Vision Examination Report Applicant ID Applicant Information To be completed by the applicant Surname Given Names Date of Birth (yyyy-mm-dd) Street Address City Province Postal Code (A9A 9A9) Date of Exam (yyyy-mm-dd) Visual Examination To be completed by the Ophthalmologist or Optometrist Visual Acuity Any standardized procedures (Landoit Ring, Snellen) may be utilized. No error is allowed per line of symbols. Uncorrected Right Eye (6/ or 20/) Uncorrected Left Eye (6/ or 20/) Corrected Right Eye (6/ or 20/) Corrected Left Eye (6/ or 20/) Corrected by Eyeglasses Contact Lenses RCMP Vision Standards Visual Acuity Corrected vision (with glasses or contacts): Visual acuity must be at least 6/6 (20/20) in one eye and 6/9 (20/30) in the other; and Uncorrected vision (without glasses or contacts): Visual acuity must be at least 6/18 (20/60) in each eye or 6/12 (20/40) in one eye and at least 6/30 (20/100) in the other eye. Meets Standards, both corrected and uncorrected? Yes No Visual Fields RCMP Field of Vision Standards Must be at least 150 degrees continuous along the horizontal meridian and 20 degrees continuous above and below fixation, with both eyes open and examined together. Meets Standards? Yes No Colour-Vision Standardized Ishihara pseudo-isochromatic plates must be utilized. Testing is to be done without the candidate using any colour correcting aids, such as coloured contact lenses. a) Result of standardized Ishihara pseudo-isochromatic plates test Passed Failed. If so, re-test using Farnsworth D-15. -

Modern Laser in Situ Keratomileusis Outcomes
REVIEW/UPDATE Modern laser in situ keratomileusis outcomes Helga P. Sandoval, MD, MSCR, Eric D. Donnenfeld, MD, Thomas Kohnen, MD, PhD, FEBO, Richard L. Lindstrom, MD, Richard Potvin, OD, David M. Tremblay, MD, Kerry D. Solomon, MD Laser in situ keratomileusis (LASIK) articles published between 2008 and 2015 that contain clin- ical outcomes data were reviewed and graded for quality, impression, and potential bias. All 97 relevant articles (representing 67 893 eyes) provided a positive or neutral impression of LASIK. Industry bias was not evident. The aggregate loss of 2 or more lines of corrected distance visual acuity was 0.61% (359/58 653). The overall percentage of eyes with uncorrected distance visual acuity better than 20/40 was 99.5% (59 503/59 825). The spherical equivalent refraction was within G1.0 diopter (D) of the target refraction in 98.6% (59 476/60 329) of eyes, with 90.9% (59 954/65 974) within G0.5 D. In studies reporting patient satisfaction, 1.2% (129/9726) of pa- tients were dissatisfied with LASIK. Aggregate outcomes appear better than those reported in summaries of the safety and effectiveness of earlier laser refractive surgery systems approved by the U.S. Food and Drug Administration. Modern results support the safety, efficacy, and patient satisfaction of the procedure. Financial Disclosure: Proprietary or commercial disclosures are listed after the references. J Cataract Refract Surg 2016; 42:1224–1234 Q 2016 ASCRS and ESCRS Laser in situ keratomileusis (LASIK) is one of the most have been performed globally.1 Laser in situ keratomil- commonly performed elective procedures in the United eusis was introduced by Pallikaris et al.2 in 1990. -

Fast Facts & Stats
FAST FACTS & STATS “Of all the senses, sight must be the most delightful.” ~ Helen Keller More sensory neurons are dedicated to vision than the other four senses combined, and giving the gift of sight – through cornea donation – can be life-giving and life-changing. But what does it really mean? “Eye donation” doesn’t mean the entire eye is transplanted; instead, only the cornea (the clear, dome-shaped surface that covers the front of the eye) is replaced, restoring sight for those with cornea-related blindness. The entire eye can be used for research and education, potentially helping untold thousands of people regain their sight as researchers gain new understanding of the cause and effects of eye conditions that lead to blindness. Historical facts: · The first human corneal transplant was performed in 1905 by Dr. Eduard Zirm in Olomouc, Czechoslovakia. · The first U.S. transplant was performed in New York City by Dr. R. Townley Paton in 1937. · The first eye bank – a non-profit organization that recovers, evaluates, prepares and distributes eyes donated for use in corneal transplantation, research and education – opened in 1944 in New York City. · The Eye Bank Association of America, established in 1961, is the oldest transplant association and was formed by a group of ophthalmologists and eye bankers. Statistics: · 50,930: Number of corneas provided for transplant in the U.S. in 2017, meeting 100% of U.S. demand. · 33,367: Number of corneas exported, helping restore sight worldwide. · 12 million: Corneal disease cases worldwide that result in blindness or visual impairment— and that could be reversed with cornea transplants. -

Early Postoperative Rotational Stability and Its Related Factors of a Single-Piece Acrylic Toric Intraocular Lens
Eye (2020) 34:474–479 https://doi.org/10.1038/s41433-019-0521-0 ARTICLE Early Postoperative Rotational stability and its related factors of a single-piece acrylic toric intraocular lens 1,2 3 4 5 1 1 1 Shuyi Li ● Xi Li ● Suhong He ● Qianyin Zheng ● Xiang Chen ● Xingdi Wu ● Wen Xu Received: 30 November 2018 / Accepted: 18 June 2019 / Published online: 12 July 2019 © The Author(s) 2019. This article is published with open access Abstract Purpose In the present study, we aimed to evaluate the early postoperative rotational stability of TECNIS toric intraocular lens (IOL) and analyse its correlation with preoperative and intraoperative parameters. Methods A total of 102 eyes from 87 cataract patients who underwent implantation of TECNIS toric IOL during July 2016 to November 2017 were enrolled in this retrospective study. Preoperative parameters including corneal astigmatism, axial length (AL), lens thickness (LT), anterior chamber depth (ACD) and sulcus-to-sulcus (STS), were determined. The area of capsulorhexis was measured with Rhinoceros 5.0 software. The follow-up examinations including the residual astigmatism (RAS) and postoperative toric IOL axis, were performed at 1 month and 3 months after surgery. − − 1234567890();,: 1234567890();,: Results RAS was 0.84 ± 0.88 D at 1 month and 0.81 ± 0.89 D at 3 months after surgery. The rotation of toric IOL at 3 months was 4.83 ± 3.65°. The Pearson’s r of ACD, horizontal and vertical STS, and toric IOL target axis was 0.011, 0.039, 0.045 and 0.082. The toric IOL rotation was positively correlated with the area of capsulorhexis (r = 0.522, P = 0.0003), LT (r = 0.288, P = 0.003) and AL (r = 0.259, P = 0.009). -
Exploring Vigilance Notification for Organs
NOTIFY - E xploring V igilanc E n otification for o rgans , t issu E s and c E lls NOTIFY Exploring VigilancE notification for organs, tissuEs and cElls A Global Consultation e 10,00 Organised by CNT with the co-sponsorship of WHO and the participation of the EU-funded SOHO V&S Project February 7-9, 2011 NOTIFY Exploring VigilancE notification for organs, tissuEs and cElls A Global Consultation Organised by CNT with the co-sponsorship of WHO and the participation of the EU-funded SOHO V&S Project February 7-9, 2011 Cover Bologna, piazza del Nettuno (photo © giulianax – Fotolia.com) © Testi Centro Nazionale Trapianti © 2011 EDITRICE COMPOSITORI Via Stalingrado 97/2 - 40128 Bologna Tel. 051/3540111 - Fax 051/327877 [email protected] www.editricecompositori.it ISBN 978-88-7794-758-1 Index Part A Bologna Consultation Report ............................................................................................................................................7 Part B Working Group Didactic Papers ......................................................................................................................................57 (i) The Transmission of Infections ..........................................................................................................................59 (ii) The Transmission of Malignancies ....................................................................................................................79 (iii) Adverse Outcomes Associated with Characteristics, Handling and Clinical Errors -

Xenotransplantation: Past, Present, and Future
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Curr Opin Manuscript Author Organ Transplant Manuscript Author . Author manuscript; available in PMC 2018 December 01. Published in final edited form as: Curr Opin Organ Transplant. 2017 December ; 22(6): 513–521. doi:10.1097/MOT.0000000000000463. XENOTRANSPLANTATION: PAST, PRESENT, AND FUTURE Burcin Ekser, MD, PhD1, Ping Li, PhD1, and David K.C. Cooper, MD, PhD2 1Division of Transplant Surgery, Department of Surgery, Indiana University School of Medicine, Indianapolis, IN, USA 2Xenotransplantation Program, Department of Surgery, The University of Alabama at Birmingham, Birmingham, AL, USA Abstract Purpose of review—To review the progress in the field of xenotransplantation with special attention to most recent encouraging findings which will eventually bring xenotransplantation to the clinic in the near future. Recent findings—Starting from early 2000, with the introduction of Gal-knockout pigs, prolonged survival especially in heart and kidney xenotransplantation was recorded. However, remaining antibody barriers to nonGal antigens continue to be the hurdle to overcome. The production of genetically-engineered pigs was difficult requiring prolonged time. However, advances in gene editing, such as zinc finger nucleases, transcription activator-like effector nucleases, and most recently CRISPR technology made the production of genetically-engineered pigs easier and available to more researchers. Today, the survival of pig-to-nonhuman primate heterotopic heart, kidney, and islet xenotransplantation reached >900 days, >400 days, and >600 day, respectively. The availability of multiple-gene pigs (5 or 6 genetic modifications) and/or newer costimulation blockade agents significantly contributed to this success. Now, the field is getting ready for clinical trials with an international consensus. -

History of Corneal Transplantation, Eye Banking and the EBAA The
History of Corneal Transplantation, Eye Banking and the EBAA The Success of Early Corneal Transplants In 1905, when Eduard Konrad Zirm, MD, performed the first successful corneal transplant, a long line of corneal transplantation, research and techniques began. During its existence, Zirm’s eye bank, located in a rural area of Austria, treated over 47,000 patients. Not many years later in 1914, Anton Elschnig, MD, also of Austria, performed the second successful corneal transplant and over the next two decades, he would make various contributions to the study of peri-operative infection and pre-operative preparation. The 1920s and 1930s would find Russian ophthalmologist Vladimir Filatov refining lamellar keratoplasty and developing a new method for full thickness keratoplasty. He also used a donor cornea from a cadaver for a penetrating keratoplasty in the 1930s. Ramon Castroviejo, a Spanish ophthalmologist, was an influential figure in both European and American developments in corneal transplantation, particularly from the 1920s through the 1940s. During his research fellowship at the Mayo Clinic, he developed a double-bladed knife for square grafts and conducted research that culminated in the development of new keratoplasty techniques. The Beginnings of Eye Banking and the EBAA The 1940s not only brought improvements to corneal transplantation, but also an incentive to mainstream those procedures into eye banking. R. Townley Paton, a renowned American ophthalmologist who was trained at Johns Hopkins in Baltimore, had established his own practice and had become affiliated with Manhattan Eye, Ear & Throat Hospital, where he began performing corneal transplants with privately-acquired tissue. After performing many corneal transplants, Paton came to the conclusion that a formal system of eye collection needed to be developed – thus, the eye bank was born. -

Ophthalmology Abbreviations Alphabetical
COMMON OPHTHALMOLOGY ABBREVIATIONS Listed as one of America’s Illinois Eye and Ear Infi rmary Best Hospitals for Ophthalmology UIC Department of Ophthalmology & Visual Sciences by U.S.News & World Report Commonly Used Ophthalmology Abbreviations Alphabetical A POCKET GUIDE FOR RESIDENTS Compiled by: Bryan Kim, MD COMMON OPHTHALMOLOGY ABBREVIATIONS A/C or AC anterior chamber Anterior chamber Dilators (red top); A1% atropine 1% education The Department of Ophthalmology accepts six residents Drops/Meds to its program each year, making it one of nation’s largest programs. We are anterior cortical changes/ ACC Lens: Diagnoses/findings also one of the most competitive with well over 600 applicants annually, of cataract whom 84 are granted interviews. Our selection standards are among the Glaucoma: Diagnoses/ highest. Our incoming residents graduated from prestigious medical schools ACG angle closure glaucoma including Brown, Northwestern, MIT, Cornell, University of Michigan, and findings University of Southern California. GPA’s are typically 4.0 and board scores anterior chamber intraocular ACIOL Lens are rarely lower than the 95th percentile. Most applicants have research lens experience. In recent years our residents have gone on to prestigious fellowships at UC Davis, University of Chicago, Northwestern, University amount of plus reading of Iowa, Oregon Health Sciences University, Bascom Palmer, Duke, UCSF, Add power (for bifocal/progres- Refraction Emory, Wilmer Eye Institute, and UCLA. Our tradition of excellence in sives) ophthalmologic education is reflected in the leadership positions held by anterior ischemic optic Nerve/Neuro: Diagno- AION our alumni, who serve as chairs of ophthalmology departments, the dean neuropathy ses/findings of a leading medical school, and the director of the National Eye Institute.