Refractive Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

History of Refractive Surgery
History of Refractive Surgery Refractive surgery corrects common vision problems by reshaping the cornea, the eye’s outermost layer, to bend light rays to focus on the retina, reducing an individual’s dependence on eye glasses or contact lenses.1 LASIK, or laser-assisted in situ keratomileusis, is the most commonly performed refractive surgery to treat myopia, hyperopia and astigmatism.1 The first refractive surgeries were said to be the removal of cataracts – the clouding of the lens in the eye – in ancient Greece.2 1850s The first lensectomy is performed to remove the lens 1996 Clinical trials for LASIK begin and are approved by the of the eye to correct myopia.2 Food & Drug Administration (FDA).3 Late 19th 2 Abott Medical Optics receives FDA approval for the first Century The first surgery to correct astigmatism takes place. 2001 femtosecond laser, the IntraLase® FS Laser.3 The laser is used to create a circular, hinged flap in the cornea, which allows the surgeon access to the tissue affecting the eye’s 1978 Radial Keratotomy is introduced by Svyatoslov Fyodorov shape.1 in the U.S. The procedure involves making a number of incisions in the cornea to change its shape and 2002 The STAR S4 IR® Laser is introduced. The X generation is correct refractive errors, such as myopia, hyperopia used in LASIK procedures today.4 and astigmatism.2,3 1970s Samuel Blum, Rangaswamy Srinivasan and James J. Wynne 2003 The FDA approves the use of wavefront technology,3 invent the excimer laser at the IBM Thomas J. Watson which creates a 3-D map of the eye to measure 1980s Research Center in Yorktown, New York. -

Perioperative Assessment for Refractive Cataract Surgery
642 REVIEW/UPDATE Perioperative assessment for refractive cataract surgery Kendall Donaldson, MD, MS, Luis Fernandez-Vega-Cueto, MD, PhD, Richard Davidson, MD, Deepinder Dhaliwal, MD, Rex Hamilton, MD, Mitchell Jackson, MD, Larry Patterson, MD, Karl Stonecipher, MD, for the ASCRS Refractive–Cataract Surgery Subcommittee As cataract surgery has evolved into lens-based refractive surgery, decisions regarding the power of the IOL to be implanted during cata- expectations for refractive outcomes continue to increase. During ract surgery. However, with all the available technology, it can be diffi- the past decade, advancements in technology have provided new cult to decipher which of the many technologies is necessary or best ways to measure the cornea in preparation for cataract surgery. for patients and for practices. This article reviews currently available The increasing ability to accurately estimate corneal power allows options for topography, tomography, keratometry, and biometry in determination of the most precise intraocular lens (IOL) for each pa- preparation for cataract surgery. In addition, intraoperative aberrom- tient. New equipment measures the anterior and posterior corneal etry and integrated cataract suites are reviewed. surfaces to most accurately estimate corneal power and corneal ab- errations. These measurements help surgeons make the best J Cataract Refract Surg 2018; 44:642–653 Q 2018 ASCRS and ESCRS ver the past 2 decades, we have experienced an only the anterior corneal surface with the use of topo- evolution in cataract surgery from simply the graphic devices; however with discovery of the impact of O removal of the cloudy lens to a refractive proced- posterior corneal astigmatism, we can now achieve higher ure that provides patients with increasingly higher levels degrees of accuracy by taking into account the effect of the of spectacle independence. -
Safety Considerations for Phakic Iols Avoid Potential Problems by Paying Attention to These Points
REFRACTIVE SURGERY FEATURE STORY Safety Considerations for Phakic IOLs Avoid potential problems by paying attention to these points. BY GWyn SAMUEL WILLIAMS, MRCS; AND MOHAMMED MUHTASEB, FRCOPHTH n the decades since their introduction in the 1950s, phakic IOLs have become a compelling option for the correction of refractive error. There are, however, potential problems that can result from electing a Iphakic IOL as part of a refractive solution. Consequently, various safety parameters have been devised to mini- mize risks. But before complications can be properly addressed, it is important to distinguish among the avail- able phakic IOLs and differentiate those problems associ- ated with each lens design. TYPES OF PHAKIC IOL Initial phakic IOL designs were angle-fixated lenses Figure 1. The Artisan lens is the longest-serving example of intended for implantation in the anterior chamber.1 an iris-supported lens. Unfortunately, the first 5-year follow-up study demon- strated a high rate of angle recession, glaucoma, hyphe- Posterior chamber phakic IOLs. The move to the pos- ma, endothelial cell loss, and decentration, leading to terior chamber began in the 1980s, when surgeons began removal in up to 60% of cases.2 Subsequent lens designs fixating iris-supported lenses on the posterior rather than improved, and today, in addition to anterior chamber the anterior face of the iris but continued to place the phakic IOLs, posterior chamber phakic IOLs are also optic in the anterior chamber.6 These so-called anterior- available. posterior lenses were associated with pupil block and Anterior chamber phakic IOLs. Phakic IOLs designed daytime photophobia in bright light, as the pupil could for the anterior chamber are either angle-supported or not constrict beyond a certain size due to the protrud- iris-supported. -

Ocular Surface Changes Associated with Ophthalmic Surgery
Journal of Clinical Medicine Review Ocular Surface Changes Associated with Ophthalmic Surgery Lina Mikalauskiene 1, Andrzej Grzybowski 2,3 and Reda Zemaitiene 1,* 1 Department of Ophthalmology, Medical Academy, Lithuanian University of Health Sciences, 44037 Kaunas, Lithuania; [email protected] 2 Department of Ophthalmology, University of Warmia and Mazury, 10719 Olsztyn, Poland; [email protected] 3 Institute for Research in Ophthalmology, Foundation for Ophthalmology Development, 61553 Poznan, Poland * Correspondence: [email protected] Abstract: Dry eye disease causes ocular discomfort and visual disturbances. Older adults are at a higher risk of developing dry eye disease as well as needing for ophthalmic surgery. Anterior segment surgery may induce or worsen existing dry eye symptoms usually for a short-term period. Despite good visual outcomes, ocular surface dysfunction can significantly affect quality of life and, therefore, lower a patient’s satisfaction with ophthalmic surgery. Preoperative dry eye disease, factors during surgery and postoperative treatment may all contribute to ocular surface dysfunction and its severity. We reviewed relevant articles from 2010 through to 2021 using keywords “cataract surgery”, ”phacoemulsification”, ”refractive surgery”, ”trabeculectomy”, ”vitrectomy” in combina- tion with ”ocular surface dysfunction”, “dry eye disease”, and analyzed studies on dry eye disease pathophysiology and the impact of anterior segment surgery on the ocular surface. Keywords: dry eye disease; ocular surface dysfunction; cataract surgery; phacoemulsification; refractive surgery; trabeculectomy; vitrectomy Citation: Mikalauskiene, L.; Grzybowski, A.; Zemaitiene, R. Ocular Surface Changes Associated with Ophthalmic Surgery. J. Clin. 1. Introduction Med. 2021, 10, 1642. https://doi.org/ 10.3390/jcm10081642 Dry eye disease (DED) is a common condition, which usually causes discomfort, but it can also be an origin of ocular pain and visual disturbances. -

Effects of Depth of Incision on Final Outcome in Radial Keratotomy N
Effects of Depth of Incision on final outcome in Radial Keratotomy N. Raja, M. K. Niazi B-35, PAF Complex, Sector E-9, Islamabad. Abstract Objective: To assess the effect of depth of incision on the final outcome of radial keratotomy for correction of myopia. Methods: Sixty-five eyes with preoperative uncorrected myopia between 2.5-6.0D in subjects with a mean age of 29.2 (+7) years underwent radial keratotomy between Sept 1999--July 2002 in department of Ophthalmology, Military Hospital, Rawalpindi. Based on their preoperative depth of incision the eyes were divided into group-A (twenty-five eyes), with an incision depth of 500-530 µm, and Group-B (forty eyes), with an incision depth of 531- 560 µm. The comparison between the postoperative visual acuity of two groups was made at the end of study after one years` follow up. Results: A total of Sixteen eyes in Group-A (64%) that were within one diopter of emmetropia at first follow-up reverted back to their preoperative myopic state after one year of surgery as compared to only two eyes (5%) in Group-B (p<0.05). Hyperopic shift occurred in two eyes (8%) in Group-A, as compared to four eyes (10%) of Group-B (p >0.05). After one year, refraction showed that only 24% cases of Group-A were within 1 diopter of emmetropia as compared to 85% cases in Group-B. Similarly, 40% cases of Group-A were within 2 diopters of emmetropia as compared to 90% cases of Group-B. Glare and variation of vision in the initial four weeks were the most frequently reported complications in both groups. -

Refractive Surgery Faqs. Refractive Surgery the OD's Role in Refractive
9/18/2013 Refractive Surgery Refractive Surgery FAQs. Help your doctor with refractive surgery patient education Corneal Intraocular Bill Tullo, OD, FAAO, LASIK Phakic IOL Verisys Diplomate Surface Ablation Vice-President of Visian PRK Clinical Services LASEK CLE – Clear Lens Extraction TLC Laser Eye Centers Epi-LASIK Cataract Surgery AK - Femto Toric IOL Multifocal IOL ICRS - Intacs Accommodative IOL Femtosecond Assisted Inlays Kamra The OD’s role in Refractive Surgery Refractive Error Determine the patient’s interest Myopia Make the patient aware of your ability to co-manage surgery Astigmatism Discuss advancements in the field Hyperopia Outline expectations Presbyopia/monovision Presbyopia Enhancements Risks Make a recommendation Manage post-op care and expectations Myopia Myopic Astigmatism FDA Approval Common Use FDA Approval Common Use LASIK: 1D – 14D LASIK: 1D – 8D LASIK: -0.25D – -6D LASIK: -0.25D – -3.50D PRK: 1D – 13D PRK: 1D – 6D PRK: -0.25D – -6D PRK: -0.25D – -3.50D Intacs: 1D- 3D Intacs: 1D- 3D Intacs NONE Intacs: NONE P-IOL: 3D- 20D P-IOL: 8D- 20D P-IOL: NONE P-IOL: NONE CLE/CAT: any CLE/CAT: any CLE/CAT: -0.75D - -3D CLE/CAT: -0.75D - -3D 1 9/18/2013 Hyperopia Hyperopic Astigmatism FDA Approval Common Use FDA Approval Common Use LASIK: 0.25D – 6D LASIK: 0.25D – 4D LASIK: 0.25D – 6D LASIK: 0.25D – 4D PRK: 0.25D – 6D PRK: 0.25D – 4D PRK: 0.25D – 6D PRK: 0.25D – 4D Intacs: NONE Intacs: NONE Intacs: NONE Intacs: NONE P-IOL: NONE P-IOL: NONE P-IOL: NONE P-IOL: -

Improved Preservation of Human Corneal Basement Membrane
BritishJournal ofOphthalmology 1994; 78: 863-870 863 Improved preservation ofhuman corneal basement membrane following freezing of donor tissue for Br J Ophthalmol: first published as 10.1136/bjo.78.11.863 on 1 November 1994. Downloaded from epikeratophakia Robert D Young, W John Armitage, Paul Bowerman, Stuart D Cook, David L Easty Abstract States, good results continue to be achieved by Current methods for the production of the small number ofBritish surgeons performing lenticules for epikeratophakia involve rapid the technique.4 However, no comprehensive freezing, cryolathing, and slow warming of the account of its long term outcome has yet been donor cornea. We have found that this pro- published. cedure causes structural damage to the Several complications resulting in the failure epithelial basement membrane in the donor of epikeratophakia have been reported, includ- cornea which may subsequently contribute to ing infection, graft dehiscence, persistent inter- poor postoperative re-epithelialisation of the face haze or opacity, ulceration, and imperfect implant, leading to graft failure. Endeavouring re-epithelialisation. Among these, the failure of to overcome these problems, the effects of host epithelial cells to migrate over and re- cryoprotection of donor cornea were investi- surface the anterior face of the grafted tissue gated, using dimethyl sulphoxide, in conjunc- continues to be the major reason for the removal tion with different cooling and warming rates ofepikeratophakia lenticules.'-'0 as part of the protocol for cryolathing. The Epithelial healing is itselfa complex phenome- structural integrity of the epithelial basement non involving mitosis of host cells at the graft membrane zone (BMZ) was then assessed by periphery, centripetal migration, and attach- electron microscopy and by immunofluores- ment. -

Anesthesia for Eye Surgery
Anesthesia for Eye Surgery Having a surgery can be stressful. We would like to provide you the following information to help you prepare for your eye surgery. Eye surgeries are typically done under topical or local anesthesia with or without mild sedation. Topical Anesthesia This is administered via special eye drops by a preoperative nurse. Local Anesthesia This is administered via injection by an ophthalmologist. Your ophthalmologist will inject local anesthesia to the eye that is to undergo the operation. During the injection, you will be lightly sedated. In the operating room During the procedure it is very important that you remain still. This is a very delicate surgery; any abrupt movement can hinder a surgeon’s performance. If you have any concerns during the surgery, such as pain, urge to cough or itching, please let us know immediately. Typically, patients are not heavily sedated for this type of procedure. Therefore, it is normal for patients to feel pressure around their eyes, but not pain. In order to maintain surgical sterility, your face and body will be covered with a sterile drape. You will be given supplemental oxygen to breathe. An anesthesia clinician will continue to monitor your vital signs for the duration of the procedure. The length of the procedure usually ranges from 10 minutes to 30 minutes. In the recovery room After surgery, you will be brought to the recovery room. A recovery room nurse will continue to monitor your vital signs for the next 20 to 30 minutes. It is important that you do not drive or operate any machinery for the next 24 hours. -

Table of Contents
Leadership Development Program Project Abstracts Table of Contents LDP XXII, CLASS OF 2020 GRADUATES Name/Society/Project Page John J. Chen, MD, PhD 1 North American Neuro-Ophthalmology Society Project: The Neuro-Ophthalmology career path: misconceptions and barriers to recruitment Jeremy D. Clark, MD 2 Kentucky Academy of Eye Physicians and Surgeons Project: The Web of Innovation: Silent Auction Benefitting Political Action funds in Kentucky Gennifer J. Greebel, MD 3 New York State Ophthalmological Society Project: Inspiring Professional Aspirations in Adolescents with Low Vision Mark A. Greiner, MD 4 Eye Bank Association of America Project: Revisiting Eye Banking Medical Standards To Accommodate Emerging Technologies Jennifer F. Jordan, MD 5 North Carolina Society of Eye Physicians and Surgeons Project: Advocacy Exposure for North Carolina Ophthalmologists in Training Kapil G. Kapoor, MD 6 Virginia Society of Eye Physicians and Surgeons Project: Unwrapping Virginia Bill 506B Erin Lichtenstein, MD 7 Maine Society of Eye Physicians and Surgeons Project: Bringing Ophthalmology Residents to Maine Jennifer L. Lindsey, MD 8 Association of Veterans Affairs Ophthalmologists Project: Illuminating the Path to Advocacy for Veterans Affairs Ophthalmologists Donald A. Morris, DO 9 American Osteopathic College of Ophthalmology Project: Single Accreditation of Ophthalmology residencies is here. What is the next step? Lisa Nijm, MD, JD 10 Women in Ophthalmology Project: Implementing a Clinical Trials Training Program to Increase Diversity of Primary Investigators Involved in Ophthalmic Research LDP XXII, CLASS OF 2020 GRADUATES (cont’d) Name/Society/Project Page Roma P. Patel, MD, MBA 11 California Academy of Eye Physicians and Surgeons Project: Increasing Membership Value to our CAEPS Members Jelena Potic, MD, PhD 12 European Society of Ophthalmology Project: Harmonization of Surgical Skills Standards for Young Ophthalmologists across Europe Pradeep Y. -
RCMP GRC 2180E (2017-10) Page 1 of 2 Protected B RM Applicant Vision Examination Report Once Completed Applicant ID
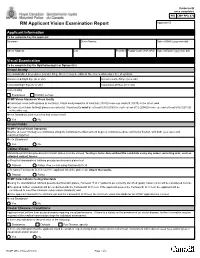
Protected B once completed PIB CMP PPU 070 RM Applicant Vision Examination Report Applicant ID Applicant Information To be completed by the applicant Surname Given Names Date of Birth (yyyy-mm-dd) Street Address City Province Postal Code (A9A 9A9) Date of Exam (yyyy-mm-dd) Visual Examination To be completed by the Ophthalmologist or Optometrist Visual Acuity Any standardized procedures (Landoit Ring, Snellen) may be utilized. No error is allowed per line of symbols. Uncorrected Right Eye (6/ or 20/) Uncorrected Left Eye (6/ or 20/) Corrected Right Eye (6/ or 20/) Corrected Left Eye (6/ or 20/) Corrected by Eyeglasses Contact Lenses RCMP Vision Standards Visual Acuity Corrected vision (with glasses or contacts): Visual acuity must be at least 6/6 (20/20) in one eye and 6/9 (20/30) in the other; and Uncorrected vision (without glasses or contacts): Visual acuity must be at least 6/18 (20/60) in each eye or 6/12 (20/40) in one eye and at least 6/30 (20/100) in the other eye. Meets Standards, both corrected and uncorrected? Yes No Visual Fields RCMP Field of Vision Standards Must be at least 150 degrees continuous along the horizontal meridian and 20 degrees continuous above and below fixation, with both eyes open and examined together. Meets Standards? Yes No Colour-Vision Standardized Ishihara pseudo-isochromatic plates must be utilized. Testing is to be done without the candidate using any colour correcting aids, such as coloured contact lenses. a) Result of standardized Ishihara pseudo-isochromatic plates test Passed Failed. If so, re-test using Farnsworth D-15. -

Modern Laser in Situ Keratomileusis Outcomes
REVIEW/UPDATE Modern laser in situ keratomileusis outcomes Helga P. Sandoval, MD, MSCR, Eric D. Donnenfeld, MD, Thomas Kohnen, MD, PhD, FEBO, Richard L. Lindstrom, MD, Richard Potvin, OD, David M. Tremblay, MD, Kerry D. Solomon, MD Laser in situ keratomileusis (LASIK) articles published between 2008 and 2015 that contain clin- ical outcomes data were reviewed and graded for quality, impression, and potential bias. All 97 relevant articles (representing 67 893 eyes) provided a positive or neutral impression of LASIK. Industry bias was not evident. The aggregate loss of 2 or more lines of corrected distance visual acuity was 0.61% (359/58 653). The overall percentage of eyes with uncorrected distance visual acuity better than 20/40 was 99.5% (59 503/59 825). The spherical equivalent refraction was within G1.0 diopter (D) of the target refraction in 98.6% (59 476/60 329) of eyes, with 90.9% (59 954/65 974) within G0.5 D. In studies reporting patient satisfaction, 1.2% (129/9726) of pa- tients were dissatisfied with LASIK. Aggregate outcomes appear better than those reported in summaries of the safety and effectiveness of earlier laser refractive surgery systems approved by the U.S. Food and Drug Administration. Modern results support the safety, efficacy, and patient satisfaction of the procedure. Financial Disclosure: Proprietary or commercial disclosures are listed after the references. J Cataract Refract Surg 2016; 42:1224–1234 Q 2016 ASCRS and ESCRS Laser in situ keratomileusis (LASIK) is one of the most have been performed globally.1 Laser in situ keratomil- commonly performed elective procedures in the United eusis was introduced by Pallikaris et al.2 in 1990. -

Laser Vision Correction Surgery
Patient Information Laser Vision Correction 1 Contents What is Laser Vision Correction? 3 What are the benefits? 3 Who is suitable for laser vision correction? 4 What are the alternatives? 5 Vision correction surgery alternatives 5 Alternative laser procedures 5 Continuing in glasses or contact lenses 5 How is Laser Vision Correction performed? 6 LASIK 6 Surface laser treatments 6 SMILE 6 What are the risks? 7 Loss of vision 7 Additional surgery 7 Risks of contact lens wear 7 What are the side effects? 8 Vision 8 Eye comfort 8 Eye Appearance 8 Will laser vision correction affect my future eye health care? 8 How can I reduce the risk of problems? 9 How much does laser vision correction cost? 9 2 What is Laser Vision Correction? Modern surgical lasers are able to alter the curvature and focusing power of the front surface of the eye (the cornea) very accurately to correct short sight (myopia), long sight (hyperopia), and astigmatism. Three types of procedure are commonly used in If you are suitable for laser vision correction, your the UK: LASIK, surface laser treatments (PRK, surgeon will discuss which type of procedure is the LASEK, TransPRK) and SMILE. Risks and benefits are best option for you. similar, and all these procedures normally produce very good results in the right patients. Differences between these laser vision correction procedures are explained below. What are the benefits? For most patients, vision after laser correction is similar to vision in contact lenses before surgery, without the potential discomfort and limitations on activity. Glasses may still be required for some activities after Short sight and astigmatism normally stabilize in treatment, particularly for reading in older patients.