Higher Lung Deposition with Respimat® Soft Mist™ Inhaler Than HFA-MDI in COPD Patients with Poor Technique
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

California Essential Drug List
California Essential Drug List The Essential Drug List (formulary) includes a list of drugs covered by Health Net. The drug list is updated at least monthly and is subject to change. All previous versions are no longer in effect. You can view the most current drug list by going to our website at www.healthnet.com. Refer to Evidence of Coverage or Certificate of Insurance for specific cost share information. For California Individual & Family Plans: Drug Lists Select Health Net Large Group – Formulary (pdf). For Small Business Group: Drug Lists Select Health Net Small Business Group – Formulary (pdf). NOTE: To search the drug list online, open the (pdf) document. Hold down the “Control” (Ctrl) and “F” keys. When the search box appears, type the name of your drug and press the “Enter” key. If you have questions or need more information call us toll free. California Individual & Family Plans (off-Exchange) If you have questions about your pharmacy coverage call Customer Service at 1-800-839-2172 California Individual & Family Plans (on-Exchange) If you have questions about your pharmacy coverage call Customer Service at 1-888-926-4988 Hours of Operation 8:00am – 7:00pm Monday through Friday 8:00am – 5:00pm Saturday Small Business Group If you have questions about your pharmacy coverage call Customer Service at 1-800-361-3366 Hours of Operation 8:00am – 6:00pm Monday through Friday Updated September 1, 2021 Health Net of California, Inc. and Health Net Life Insurance Company are subsidiaries of Health Net, LLC and Centene Corporation. Health Net is a registered service mark of Health Net, LLC Table of Contents What If I Have Questions Regarding My Pharmacy Benefit? ................................... -
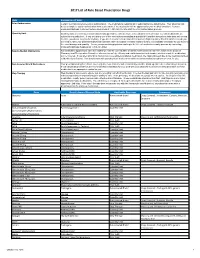
2017 List of Rule Based Prescription Drugs
2017 List of Rule Based Prescription Drugs Rule Explanation of Rule Prior Authorization Certain medications require a prior authorization. The medications requiring prior authorization are listed below. Your physician will need to complete a prior authorization form to determine if the medication will be approved for your medical condition. Contact EnvisionRXOptions Customer Service Help Desk at 1-800-361-4542 to start the Prior Authorization process. Quantity Limit Quantity limits are clinically recommended limits put in place to help ensure safe utilization of medication. Certain medications are subject to a quantity limit. If you are taking one of the medications mandating a quantity limit and the amount you take does not exceed the limit, you do not need to do anything. If you are in need of a medication that requires a higher quantity than that which is listed, you will need to have your prescribing physician submit a letter of medical necessity explaining why it is medically necessary for you to be on the exact dosage and quantity. You or your prescribing physician can begin the letter of medical necessity process by contacting EnvisionRXOptions Helpdesk at 1-800-361-4542. New-to-Market Medications Any medication approved to enter the market will only be covered after a clinical review decision has been made by the Envision Pharmacy and Therapeutics Committee who reviews safety, efficacy and cost information to determine whether or not the medication will be covered. If you attempt to fill or claim a non-covered New-to-Market medication, the claim will reject due to the medications New- to-Market classification. -
Medi-Cal Formulary May 2020
Formulary Medi-Cal MAY 2020 The IEHP Medi-Cal Formulary is subject to change throughout the year. All previous versions of the formulary are no longer in effect once a new formulary is available. The IEHP Medi-Cal Formulary can be found at: www.iehp.org/en/members/medical Last Updated: 04/17/2020 Inland Empire Health Plan (IEHP) Medi-Cal Formulary Table of Contents A . Foreword ..................................................................................................................... 2 B. IEHP Member Services .............................................................................................. 2 C. How to Use the Formulary .......................................................................................... 2 D. Prescription Coverage ................................................................................................. 3 D1. Quantity Limits .................................................................................................... 3 D2. Step Therapy ........................................................................................................ 3 E. Filling a Prescription and IEHP’s Pharmacy Network ............................................... 4 F. Definitions ................................................................................................................... 4 G. List of Covered Drugs .............................................................................................. 10 H. Index ....................................................................................................................... -

Inhalation Drug Delivery Devices: Technology Update
Medical Devices: Evidence and Research Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Inhalation drug delivery devices: technology update Mariam Ibrahim Abstract: The pulmonary route of administration has proven to be effective in local and Rahul Verma systemic delivery of miscellaneous drugs and biopharmaceuticals to treat pulmonary and non- Lucila Garcia-Contreras pulmonary diseases. A successful pulmonary administration requires a harmonic interaction between the drug formulation, the inhaler device, and the patient. However, the biggest single Department of Pharmaceutical Sciences, College of Pharmacy, problem that accounts for the lack of desired effect or adverse outcomes is the incorrect use The University of Oklahoma Health of the device due to lack of training in how to use the device or how to coordinate actuation Sciences Center, Oklahoma City, and aerosol inhalation. This review summarizes the structural and mechanical features of OK, USA aerosol delivery devices with respect to mechanisms of aerosol generation, their use with different formulations, and their advantages and limitations. A technological update of the current state-of-the-art designs proposed to overcome current challenges of existing devices is also provided. Keywords: pulmonary delivery, asthma, nebulizers, metered dose inhaler, dry powder inhaler Introduction Inhalation therapy has been used for thousands of years, albeit in a different form and use. Inhalation therapy was practiced by ancient civilizations in Egypt, Greece, India, and People’s Republic of China as evidenced by different artifacts displayed in museums, that may be considered the first used inhalation devices.1,2 Currently, inhalation therapy is the best option for lung diseases like asthma, cystic fibrosis, and chronic obstructive pulmonary disease (COPD). -

Olodaterol Monograph
Olodaterol Monograph Olodaterol (Striverdi Respimat) National Drug Monograph VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a comprehensive drug review for making formulary decisions. Updates will be made when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. FDA Approval Information Description/Mechan Olodaterol is a long-acting beta2-adrenergic agonist (LABA). Binding to and activating ism of Action beta2-adrenoceptors in the airways results in stimulation of intracellular adenyl cyclase, an enzyme that mediates the synthesis of cyclic-3’, 5’ adenosine monophosphate (cAMP). Elevated levels of cAMP induce bronchodilation by relaxation of airway smooth muscle cells. Indication(s) Under Long-term once daily maintenance bronchodilator treatment of airflow obstruction in Review patients with COPD including chronic bronchitis and/or emphysema Dosage Form(s) Inhalation spray for oral inhalation via Respimat (a soft-mist inhaler) Under Review The soft-mist inhalers (SMI) provide multi-dose medication using liquid formulations similar to that used in nebulizers and are propellant-free. Presently, Respimat is the only SMI commercially available for clinical use. The soft mist is released at a slower velocity and has more prolonged spray duration than the mist produced from pressurized metered dose inhalers (pMDIs). Pressurized MDIs require coordination of actuation with inhalation which may be difficult for some patients partly due to the rapid speed at which the drug is delivered and the short duration of the mist. -

Preventive Drug List
navitus.com Share a Clear View Preventive Drug List Updated July 2021 Your health plan is making an effort to reduce your health care costs by giving you tools to help you stay healthy and productive. Below are the medications included on your Preventive Drug List. These medications help protect against or manage some high risk medical conditions. Taking these medications as directed by your prescriber can help avoid serious health problems. That may mean fewer doctor visits and hospitalizations, reducing your total health care costs. In the drug list below, generic drugs are shown in lowercase type. Brand name drugs are shown in uppercase type. Antiasthmatic/Bronchodilators theophylline soln ADVAIR DISKUS INHALER *generic Wixela only for wixela inhaler *brand Advair Diskus only for non-HDHP plans* HDHPs* ADVAIR HFA INHALER Anticoagulant albuterol/ipratropium neb soln ELIQUIS TAB aminophylline tab PRADAXA CAP ARNUITY ELLIPTA INHALER warfarin tab ASMANEX HFA INHALER XARELTO TAB ASMANEX INHALER Antidiabetics budesonide inh susp acarbose tab FLOVENT DISKUS INHALER chlorpropamide tab FLOVENT HFA INHALER glimepiride tab fluticasone/salmeterol inhaler glipizide ER tab ipratropium neb soln glipizide tab METAPROTERENOL SYRUP glipizide/metformin tab montelukast chew tab glyburide micronized tab montelukast tab glyburide tab THEOCHRON glyburide/metformin tab theophylline CR tab metformin ER tab theophylline ER tab metformin tab • Note: The list is subject to change and not all drugs listed may be covered on your formulary. Please refer to your Navitus -

Connecticut Medicaid
ACNE AGENTS, TOPICAL ‡ ANGIOTENSIN MODULATOR COMBINATIONS ANTICONVULSANTS, CONT. CONNECTICUT MEDICAID (STEP THERAPY CATEGORY) AMLODIPINE / BENAZEPRIL (ORAL) LAMOTRIGINE CHEW DISPERS TAB (not ODT) (ORAL) (DX CODE REQUIRED - DIFFERIN, EPIDUO and RETIN-A) AMLODIPINE / OLMESARTAN (ORAL) LAMOTRIGINE TABLET (IR) (not ER) (ORAL) Preferred Drug List (PDL) ACNE MEDICATION LOTION (BENZOYL PEROXIDE) (TOPICAL)AMLODIPINE / VALSARTAN (ORAL) LEVETIRACETAM SOLUTION, IR TABLET (not ER) (ORAL) • The Connecticut Medicaid Preferred Drug List (PDL) is a BENZOYL PEROXIDE CREAM, WASH (not FOAM) (TOPICAL) OXCARBAZEPINE TABLET (ORAL) listing of prescription products selected by the BENZOYL PEROXIDE 5% and 10% GEL (OTC) (TOPICAL) ANTHELMINTICS PHENOBARBITAL ELIXIR, TABLET (ORAL) Pharmaceutical and Therapeutics Committee as efficacious, BENZOYL PEROXIDE 6% CLEANSER (OTC) (TOPICAL) ALBENDAZOLE TABLET (ORAL) PHENYTOIN CHEW TABLET, SUSPENSION (ORAL) safe and cost effective choices when prescribing for HUSKY CLINDAMYCIN PH 1% PLEGET (TOPICAL) BILTRICIDE TABLET (ORAL) PHENYTOIN SOD EXT CAPSULE (ORAL) A, HUSKY C, HUSKY D, Tuberculosis (TB) and Family CLINDAMYCIN PH 1% SOLUTION (not GEL or LOTION) (TOPICAL)IVERMECTIN TABLET (ORAL) PRIMIDONE (ORAL) Planning (FAMPL) clients. CLINDAMYCIN / BENZOYL PEROXIDE 1.2%-5% (DUAC) (TOPICAL) SABRIL 500 MG POWDER PACK (ORAL) • Preferred or Non-preferred status only applies to DIFFERIN 0.1% CREAM (TOPICAL) (not OTC GEL) (DX CODE REQ.) ANTI-ALLERGENS, ORAL SABRIL TABLET (ORAL) those medications that fall within the drug classes DIFFERIN -
A Guide to Aerosol Delivery Devices for Respiratory Therapists 4Th Edition
A Guide To Aerosol Delivery Devices for Respiratory Therapists 4th Edition Douglas S. Gardenhire, EdD, RRT-NPS, FAARC Dave Burnett, PhD, RRT, AE-C Shawna Strickland, PhD, RRT-NPS, RRT-ACCS, AE-C, FAARC Timothy R. Myers, MBA, RRT-NPS, FAARC Platinum Sponsor Copyright ©2017 by the American Association for Respiratory Care A Guide to Aerosol Delivery Devices for Respiratory Therapists, 4th Edition Douglas S. Gardenhire, EdD, RRT-NPS, FAARC Dave Burnett, PhD, RRT, AE-C Shawna Strickland, PhD, RRT-NPS, RRT-ACCS, AE-C, FAARC Timothy R. Myers, MBA, RRT-NPS, FAARC With a Foreword by Timothy R. Myers, MBA, RRT-NPS, FAARC Chief Business Officer American Association for Respiratory Care DISCLOSURE Douglas S. Gardenhire, EdD, RRT-NPS, FAARC has served as a consultant for the following companies: Westmed, Inc. and Boehringer Ingelheim. Produced by the American Association for Respiratory Care 2 A Guide to Aerosol Delivery Devices for Respiratory Therapists, 4th Edition American Association for Respiratory Care, © 2017 Foreward Aerosol therapy is considered to be one of the corner- any) benefit from their prescribed metered-dose inhalers, stones of respiratory therapy that exemplifies the nuances dry-powder inhalers, and nebulizers simply because they are of both the art and science of 21st century medicine. As not adequately trained or evaluated on their proper use. respiratory therapists are the only health care providers The combination of the right medication and the most who receive extensive formal education and who are tested optimal delivery device with the patient’s cognitive and for competency in aerosol therapy, the ability to manage physical abilities is the critical juncture where science inter- patients with both acute and chronic respiratory disease as sects with art. -

SPIOLTO® RESPIMAT® 2.5 Micrograms
AUSTRALIAN PRODUCT INFORMATION - SPIOLTO RESPIMAT 2.5 micrograms/ 2.5 micrograms tiotropium (as bromide monohydrate)/olodaterol (as hydrochloride) solution for inhalation 1 NAME OF THE MEDICINE tiotropium (as bromide monohydrate) and olodaterol (as hydrochloride) 2 QUALITATIVE AND QUANTITATIVE COMPOSITION SPIOLTO® RESPIMAT® is a soft mist inhaler delivering tiotropium + olodaterol solution for inhalation. The SPIOLTO RESPIMAT cartridge containing the solution for inhalation is only for use with the SPIOLTO RESPIMAT inhaler. The delivered dose is 2.5 microgram tiotropium and 2.5 microgram olodaterol per puff (2 puffs comprise one medicinal dose) and is equivalent to 3.124 micrograms tiotropium bromide monohydrate and 2.7 micrograms olodaterol hydrochloride. Two puffs equal one dose of 5 micrograms/5 micrograms. The delivered dose is the dose which is available for the patient after passing the mouthpiece. Excipients with known effect: SPIOLTO RESPIMAT contains 0.0011 mg benzalkonium chloride in each actuation. For the full list of excipients, see Section 6.1 List of excipients. 3 PHARMACEUTICAL FORM SPIOLTO RESPIMAT solution for inhalation is a clear, colourless solution contained in a plastic container crimped into an aluminium cylinder (cartridge) for use with the SPIOLTO RESPIMAT inhaler. The SPIOLTO RESPIMAT inhaler has a light-green coloured cap. The SPIOLTO RESPIMAT cartridge is only intended for use with the SPIOLTO RESPIMAT inhaler. 4 CLINICAL PARTICULARS 4.1 THERAPEUTIC INDICATIONS SPIOLTO RESPIMAT is indicated as a once-daily maintenance bronchodilator treatment to relieve symptoms in adult patients with chronic obstructive pulmonary disease (COPD). 4.2 DOSE AND METHOD OF ADMINISTRATION SPIOLTO RESPIMAT is for oral inhalation only. -

Spiriva Respimat-RMS-Combined-En-Clean
Version 4, 02/2016 SUMMARY OF PRODUCT CHARACTERISTICS, LABELLING AND PACKAGE LEAFLET Version: 24 May 2019 1 SUMMARY OF PRODUCT CHARACTERISTICS Version: 24 May 2019 2 1. NAME OF THE MEDICINAL PRODUCT Spiriva Respimat 2.5 microgram, inhalation solution 2. QUALITATIVE AND QUANTITATIVE COMPOSITION The delivered dose is 2.5 microgram tiotropium per puff (2 puffs comprise one medicinal dose) and is equivalent to 3.124 microgram tiotropium bromide monohydrate. The delivered dose is the dose which is available for the patient after passing the mouthpiece. Excipient with known effect: This medicine contains 0.0011 mg benzalkonium chloride in each actuation. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Inhalation solution Clear, colourless, inhalation solution 4. CLINICAL PARTICULARS 4.1 Therapeutic indications COPD Tiotropium is indicated as a maintenance bronchodilator treatment to relieve symptoms of patients with chronic obstructive pulmonary disease (COPD). Asthma Spiriva Respimat is indicated as add-on maintenance bronchodilator treatment in patients aged 6 years and older with severe asthma who experienced one or more severe asthma exacerbations in the preceding year (see sections 4.2 and 5.1). 4.2 Posology and method of administration Posology The medicinal product is intended for inhalation use only. The cartridge can only be inserted and used in the Respimat inhaler (see 4.2). Two puffs from the Respimat inhaler comprise one medicinal dose. The recommended dose for adults is 5 microgram tiotropium given as two puffs from the Respimat inhaler once daily, at the same time of the day. The recommended dose should not be exceeded. -

Allergies & Cold & Flu Antibiotics
Contact The Society of St. Vincent de Paul Charitable Pharmacy is a fully licensed pharmacy operating on a (608)‐442‐7200 stand-alone basis and providing prescribed Address medications at no charge to those low-income P.O. Box 259686 individuals who qualify for the pharmacy’s 2033 Fish Hatchery Rd services. The pharmacy stocks low-cost drugs for common conditions such as heart disease, diabetes, Madison, WI 53725‐9686 infections, and other types of illnesses. The Hours of Operation Prescription Program is designed to provide up to a 30- Mon. & Wed.: 1‐4PM day supply per prescription. Thurs.: 3‐6PM Note: This list is not an all-inclusive list. If the medication you are taking is not on the list, we still may be able to assist. [UPDATED OCTOBER 2017] ALLERGIES & COLD & FLU BRAND NAME GENERIC NAME ATARAX HYDROXYZINE HCL 25MG TABLETS CLARITIN LORATADINE 10MG TABLETS FLONASE FLUTICASONE PROPIONATE 50MCG NASAL SPRAY MUCINEX FAST‐MAX COLD ACETAMINOPHEN 650MG + DEXTROMETHORPHAN HBR 20MG + GUAIFENESIN 400MG + PHENYLEPHRINE HCL 10MG SYRUP NASONEX MOMETASONE FUROATE MONOHYDRATE 50MCG NASAL SPRAY NYQUIL LIQUID GELS ACETAMINOPHEN 325MG + DOXYLAMINE SUCCINATE 6.25MG + DEXTROMETHORPHAN HBR 15MG LIQUICAPS NYQUIL SYRUP ACETAMINOPHEN 650MG + DOXYLAMINE SUCCINATE 12.5MG + DEXTROMETHORPHAN HBR 30MG SYRUP OPTICROM CROMOLYN SODIUM 4% OPHTHALMIC SOLUTION ROBITUSSIN/ROBITUSSIN SUGAR‐FREE DEXTROMETHORPHAN HBR 20MG/10ML + GUAIFENESIN 200MG/10 ML SYRUP SINUS RINSE SALINE NASAL RINSE XYZAL 24 HR LEVOCETIRIZINE DIHYDROCHLORIDE 5MG TABLETS ZYRTEC CETIRIZINE HCL 10MG -

A Patient's Guide To
A Patient’s Guide to Aerosol Medication Delivery 3rd Edition Prepared by: Tim Op’t Holt, EdD, RRT, AE-C, FAARC Kimberly Wiles, RRT, CPFT Ellen Becker, PhD, RRT-NPS, RPFT, AE-C, FAARC Edited by: Timothy Myers, MBA, RRT-NPS, FAARC Copyright ©2017 by the American Association for Respiratory Care A Patient’s Guide to Aerosol Medication Delivery, 3rd Edition Tim Op’t Holt, EdD, RRT, AE-C, FAARC Kimberly Wiles, RRT, CPFT Ellen Becker, PhD, RRT-NPS, RPFT, AE-C, FAARC Edited by: Timothy Myers, MBA, RRT-NPS, FAARC With a Foreword by Thomas Kallstrom, MBA, RRT, FAARC Executive Director/Chief Executive Officer American Association for Respiratory Care Produced by the American Association for Respiratory Care 1 A Patient’s Guide to Aerosol Medication Delivery, 3rd Edition American Association for Respiratory Care © 2017 Foreward Gaining as much information as possible about We hope that you find this Patient Guide your aerosol delivery devices is essential. You useful. The American Association for Respiratory have taken a positive first step by obtaining this Care invites you to learn more about better third edition of “A Patient’s Guide to Aerosol self-management of lung disease through other Medication Delivery.” The American Association online resources that, again, have been created for Respiratory Care (AARC) asked respiratory to help you and to allow you to practice a higher therapists who were noted aerosol delivery level of self-management. Simply go to www. experts to write this guide. This guide was written aarc.org or www.yourlunghealth.org. There you with you in mind.