Inhaled Therapy Case: Selecting the Best Device & Mixing Nebs January 2018
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Appendix a Common Abbreviations Used in Medication
UNIVERSITY OF AMSTERDAM MASTERS THESIS Impact of Medication Grouping on Fall Risk Prediction in Elders: A Retrospective Analysis of MIMIC-III Critical Care Database Student: SRP Mentor: Noman Dormosh Dr. Martijn C. Schut Student No. 11412682 – SRP Tutor: Prof. dr. Ameen Abu-Hanna SRP Address: Amsterdam University Medical Center - Location AMC Department Medical Informatics Meibergdreef 9, 1105 AZ Amsterdam Practice teaching period: November 2018 - June 2019 A thesis submitted in fulfillment of the requirements for the degree of Master of Medical Informatics iii Abstract Background: Falls are the leading cause of injury in elderly patients. Risk factors for falls in- cluding among others history of falls, old age, and female gender. Research studies have also linked certain medications with an increased risk of fall in what is called fall-risk-increasing drugs (FRIDs), such as psychotropics and cardiovascular drugs. However, there is a lack of consistency in the definitions of FRIDs between the studies and many studies did not use any systematic classification for medications. Objective: The aim of this study was to investigate the effect of grouping medications at different levels of granularity of a medication classification system on the performance of fall risk prediction models. Methods: This is a retrospective analysis of the MIMIC-III cohort database. We created seven prediction models including demographic, comorbidity and medication variables. Medica- tions were grouped using the anatomical therapeutic chemical classification system (ATC) starting from the most specific scope of medications and moving up to the more generic groups: one model used individual medications (ATC level 5), four models used medication grouping at levels one, two, three and four of the ATC and one model did not include med- ications. -

California Essential Drug List
California Essential Drug List The Essential Drug List (formulary) includes a list of drugs covered by Health Net. The drug list is updated at least monthly and is subject to change. All previous versions are no longer in effect. You can view the most current drug list by going to our website at www.healthnet.com. Refer to Evidence of Coverage or Certificate of Insurance for specific cost share information. For California Individual & Family Plans: Drug Lists Select Health Net Large Group – Formulary (pdf). For Small Business Group: Drug Lists Select Health Net Small Business Group – Formulary (pdf). NOTE: To search the drug list online, open the (pdf) document. Hold down the “Control” (Ctrl) and “F” keys. When the search box appears, type the name of your drug and press the “Enter” key. If you have questions or need more information call us toll free. California Individual & Family Plans (off-Exchange) If you have questions about your pharmacy coverage call Customer Service at 1-800-839-2172 California Individual & Family Plans (on-Exchange) If you have questions about your pharmacy coverage call Customer Service at 1-888-926-4988 Hours of Operation 8:00am – 7:00pm Monday through Friday 8:00am – 5:00pm Saturday Small Business Group If you have questions about your pharmacy coverage call Customer Service at 1-800-361-3366 Hours of Operation 8:00am – 6:00pm Monday through Friday Updated September 1, 2021 Health Net of California, Inc. and Health Net Life Insurance Company are subsidiaries of Health Net, LLC and Centene Corporation. Health Net is a registered service mark of Health Net, LLC Table of Contents What If I Have Questions Regarding My Pharmacy Benefit? ................................... -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -
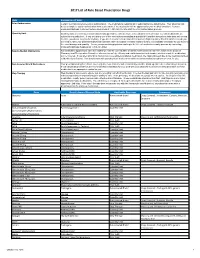
2017 List of Rule Based Prescription Drugs
2017 List of Rule Based Prescription Drugs Rule Explanation of Rule Prior Authorization Certain medications require a prior authorization. The medications requiring prior authorization are listed below. Your physician will need to complete a prior authorization form to determine if the medication will be approved for your medical condition. Contact EnvisionRXOptions Customer Service Help Desk at 1-800-361-4542 to start the Prior Authorization process. Quantity Limit Quantity limits are clinically recommended limits put in place to help ensure safe utilization of medication. Certain medications are subject to a quantity limit. If you are taking one of the medications mandating a quantity limit and the amount you take does not exceed the limit, you do not need to do anything. If you are in need of a medication that requires a higher quantity than that which is listed, you will need to have your prescribing physician submit a letter of medical necessity explaining why it is medically necessary for you to be on the exact dosage and quantity. You or your prescribing physician can begin the letter of medical necessity process by contacting EnvisionRXOptions Helpdesk at 1-800-361-4542. New-to-Market Medications Any medication approved to enter the market will only be covered after a clinical review decision has been made by the Envision Pharmacy and Therapeutics Committee who reviews safety, efficacy and cost information to determine whether or not the medication will be covered. If you attempt to fill or claim a non-covered New-to-Market medication, the claim will reject due to the medications New- to-Market classification. -

Injectable Anesthesia in South American Camelids
INJECTABLE ANESTHESIA IN SOUTH AMERICAN CAMELIDS Thomas Riebold DVM, Diplomate ACVAA Veterinary Teaching Hospital College of Veterinary Medicine Oregon State University Corvallis, Oregon 97331 INTRODUCTION Interest in llamas, and more recently in alpacas, as pets and as breeding and pack animals has led to increased demand for veterinary services for them. While they have some unique species characteristics regarding anesthesia, many of the principles and techniques used in food animal and equine anesthesia also apply to South American camelids. Except for differences in size, anesthetic management of alpacas and llamas is similar. Much like there are species differences between cattle, sheep, and goats in their response to xylazine, it does appear that alpacas require higher doses of sedatives, approximately 10-20%, to obtain the same response that lower doses of sedatives would obtain in llamas. PREANESTHETIC CONSIDERATIONS Consideration for preanesthetic preparation includes fasting, assessment of hematologic and blood chemistry values, venous catheterization, and estimation of bodyweight. The camelid has a stomach divided into three compartments. Therefore, potential complications similar to those of domestic ruminants, regurgitation and aspiration pneumonia, exist during anesthesia. Abdominal tympany as it occurs in anesthetized domestic ruminants does not appear to occur in anesthetized camelids. It is recommended that the animals be fasted 12-18 hours and deprived of water for 8-12 hours. In nonelective cases, this is often not possible and precautions should be taken to avoid aspiration of gastric fluid and ingesta. Fasting neonatal camelids is not advisable because hypoglycemia may result. As in other species, hematologic and blood chemistry values are determined before anesthesia. -
Medi-Cal Formulary May 2020
Formulary Medi-Cal MAY 2020 The IEHP Medi-Cal Formulary is subject to change throughout the year. All previous versions of the formulary are no longer in effect once a new formulary is available. The IEHP Medi-Cal Formulary can be found at: www.iehp.org/en/members/medical Last Updated: 04/17/2020 Inland Empire Health Plan (IEHP) Medi-Cal Formulary Table of Contents A . Foreword ..................................................................................................................... 2 B. IEHP Member Services .............................................................................................. 2 C. How to Use the Formulary .......................................................................................... 2 D. Prescription Coverage ................................................................................................. 3 D1. Quantity Limits .................................................................................................... 3 D2. Step Therapy ........................................................................................................ 3 E. Filling a Prescription and IEHP’s Pharmacy Network ............................................... 4 F. Definitions ................................................................................................................... 4 G. List of Covered Drugs .............................................................................................. 10 H. Index ....................................................................................................................... -

Inhalation Drug Delivery Devices: Technology Update
Medical Devices: Evidence and Research Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Inhalation drug delivery devices: technology update Mariam Ibrahim Abstract: The pulmonary route of administration has proven to be effective in local and Rahul Verma systemic delivery of miscellaneous drugs and biopharmaceuticals to treat pulmonary and non- Lucila Garcia-Contreras pulmonary diseases. A successful pulmonary administration requires a harmonic interaction between the drug formulation, the inhaler device, and the patient. However, the biggest single Department of Pharmaceutical Sciences, College of Pharmacy, problem that accounts for the lack of desired effect or adverse outcomes is the incorrect use The University of Oklahoma Health of the device due to lack of training in how to use the device or how to coordinate actuation Sciences Center, Oklahoma City, and aerosol inhalation. This review summarizes the structural and mechanical features of OK, USA aerosol delivery devices with respect to mechanisms of aerosol generation, their use with different formulations, and their advantages and limitations. A technological update of the current state-of-the-art designs proposed to overcome current challenges of existing devices is also provided. Keywords: pulmonary delivery, asthma, nebulizers, metered dose inhaler, dry powder inhaler Introduction Inhalation therapy has been used for thousands of years, albeit in a different form and use. Inhalation therapy was practiced by ancient civilizations in Egypt, Greece, India, and People’s Republic of China as evidenced by different artifacts displayed in museums, that may be considered the first used inhalation devices.1,2 Currently, inhalation therapy is the best option for lung diseases like asthma, cystic fibrosis, and chronic obstructive pulmonary disease (COPD). -

Olodaterol Monograph
Olodaterol Monograph Olodaterol (Striverdi Respimat) National Drug Monograph VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a comprehensive drug review for making formulary decisions. Updates will be made when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. FDA Approval Information Description/Mechan Olodaterol is a long-acting beta2-adrenergic agonist (LABA). Binding to and activating ism of Action beta2-adrenoceptors in the airways results in stimulation of intracellular adenyl cyclase, an enzyme that mediates the synthesis of cyclic-3’, 5’ adenosine monophosphate (cAMP). Elevated levels of cAMP induce bronchodilation by relaxation of airway smooth muscle cells. Indication(s) Under Long-term once daily maintenance bronchodilator treatment of airflow obstruction in Review patients with COPD including chronic bronchitis and/or emphysema Dosage Form(s) Inhalation spray for oral inhalation via Respimat (a soft-mist inhaler) Under Review The soft-mist inhalers (SMI) provide multi-dose medication using liquid formulations similar to that used in nebulizers and are propellant-free. Presently, Respimat is the only SMI commercially available for clinical use. The soft mist is released at a slower velocity and has more prolonged spray duration than the mist produced from pressurized metered dose inhalers (pMDIs). Pressurized MDIs require coordination of actuation with inhalation which may be difficult for some patients partly due to the rapid speed at which the drug is delivered and the short duration of the mist. -

Preventive Drug List
navitus.com Share a Clear View Preventive Drug List Updated July 2021 Your health plan is making an effort to reduce your health care costs by giving you tools to help you stay healthy and productive. Below are the medications included on your Preventive Drug List. These medications help protect against or manage some high risk medical conditions. Taking these medications as directed by your prescriber can help avoid serious health problems. That may mean fewer doctor visits and hospitalizations, reducing your total health care costs. In the drug list below, generic drugs are shown in lowercase type. Brand name drugs are shown in uppercase type. Antiasthmatic/Bronchodilators theophylline soln ADVAIR DISKUS INHALER *generic Wixela only for wixela inhaler *brand Advair Diskus only for non-HDHP plans* HDHPs* ADVAIR HFA INHALER Anticoagulant albuterol/ipratropium neb soln ELIQUIS TAB aminophylline tab PRADAXA CAP ARNUITY ELLIPTA INHALER warfarin tab ASMANEX HFA INHALER XARELTO TAB ASMANEX INHALER Antidiabetics budesonide inh susp acarbose tab FLOVENT DISKUS INHALER chlorpropamide tab FLOVENT HFA INHALER glimepiride tab fluticasone/salmeterol inhaler glipizide ER tab ipratropium neb soln glipizide tab METAPROTERENOL SYRUP glipizide/metformin tab montelukast chew tab glyburide micronized tab montelukast tab glyburide tab THEOCHRON glyburide/metformin tab theophylline CR tab metformin ER tab theophylline ER tab metformin tab • Note: The list is subject to change and not all drugs listed may be covered on your formulary. Please refer to your Navitus -

Connecticut Medicaid
ACNE AGENTS, TOPICAL ‡ ANGIOTENSIN MODULATOR COMBINATIONS ANTICONVULSANTS, CONT. CONNECTICUT MEDICAID (STEP THERAPY CATEGORY) AMLODIPINE / BENAZEPRIL (ORAL) LAMOTRIGINE CHEW DISPERS TAB (not ODT) (ORAL) (DX CODE REQUIRED - DIFFERIN, EPIDUO and RETIN-A) AMLODIPINE / OLMESARTAN (ORAL) LAMOTRIGINE TABLET (IR) (not ER) (ORAL) Preferred Drug List (PDL) ACNE MEDICATION LOTION (BENZOYL PEROXIDE) (TOPICAL)AMLODIPINE / VALSARTAN (ORAL) LEVETIRACETAM SOLUTION, IR TABLET (not ER) (ORAL) • The Connecticut Medicaid Preferred Drug List (PDL) is a BENZOYL PEROXIDE CREAM, WASH (not FOAM) (TOPICAL) OXCARBAZEPINE TABLET (ORAL) listing of prescription products selected by the BENZOYL PEROXIDE 5% and 10% GEL (OTC) (TOPICAL) ANTHELMINTICS PHENOBARBITAL ELIXIR, TABLET (ORAL) Pharmaceutical and Therapeutics Committee as efficacious, BENZOYL PEROXIDE 6% CLEANSER (OTC) (TOPICAL) ALBENDAZOLE TABLET (ORAL) PHENYTOIN CHEW TABLET, SUSPENSION (ORAL) safe and cost effective choices when prescribing for HUSKY CLINDAMYCIN PH 1% PLEGET (TOPICAL) BILTRICIDE TABLET (ORAL) PHENYTOIN SOD EXT CAPSULE (ORAL) A, HUSKY C, HUSKY D, Tuberculosis (TB) and Family CLINDAMYCIN PH 1% SOLUTION (not GEL or LOTION) (TOPICAL)IVERMECTIN TABLET (ORAL) PRIMIDONE (ORAL) Planning (FAMPL) clients. CLINDAMYCIN / BENZOYL PEROXIDE 1.2%-5% (DUAC) (TOPICAL) SABRIL 500 MG POWDER PACK (ORAL) • Preferred or Non-preferred status only applies to DIFFERIN 0.1% CREAM (TOPICAL) (not OTC GEL) (DX CODE REQ.) ANTI-ALLERGENS, ORAL SABRIL TABLET (ORAL) those medications that fall within the drug classes DIFFERIN -

“Opioid” Definition Drug Inclusion and Exclusion List
WSHA WSMA Opioid Prescribing Report Medication Inclusion/Exclusion list For purposes of developing WSHA WSMA Opioid Prescribing Report metrics, the following medications tracked in the Prescription Monitoring Program database were included and counted as “opioid prescriptions”: Drug Name ACETAMINOPHEN-CODEINE ASCOMP WITH CODEINE BELLADONNA-OPIUM BUTALB-ACETAMINOPH-CAFF-CODEIN BUTALB-CAFF-ACETAMINOPH-CODEIN BUTALBITAL COMPOUND-CODEINE BUTORPHANOL TARTRATE CARISOPRODOL-ASPIRIN-CODEINE CHERATUSSIN AC CHERATUSSIN DAC CODEINE SULFATE CODEINE-GUAIFENESIN DEMEROL DILAUDID DOLOPHINE HCL DURAMORPH ENDOCET FENTANYL CITRATE FENTORA FIORICET WITH CODEINE FIORINAL WITH CODEINE #3 GUAIATUSSIN AC GUAIFENESIN AC GUAIFENESIN DAC GUAIFENESIN W/CODEINE GUAIFENESIN-CODEINE HYDROCODONE BITARTRATE HYDROCODONE BT-HOMATROPINE MBR HYDROCODONE-ACETAMINOPHEN HYDROCODONE-CHLORPHENIRAMNE ER HYDROCODONE-HOMATROPINE MBR HYDROCODONE-IBUPROFEN HYDROMET HYDROMORPHONE HCL INFUMORPH IOPHEN-C NR LAZANDA LEVORPHANOL TARTRATE LORTAB MEPERIDINE HCL MORPHINE SULFATE NORCO NUCYNTA OPANA OPIUM TINCTURE OXAYDO OXYCODONE HCL OXYCODONE HCL-ASPIRIN OXYCODONE HCL-IBUPROFEN OXYCODONE HYDROCHLORIDE OXYCODONE-ACETAMINOPHEN OXYMORPHONE HCL PENTAZOCINE-NALOXONE HCL PERCOCET PRIMLEV PROMETHAZINE VC-CODEINE PROMETHAZINE-CODEINE PROMETHAZINE-PHENYLEPH-CODEINE ROXICODONE SUBSYS SUFENTANIL CITRATE TRAMADOL HCL TRAMADOL HCL-ACETAMINOPHEN TUSSIGON TUSSIONEX TYLENOL-CODEINE NO.3 TYLENOL-CODEINE NO.4 ULTRACET ULTRAM VICODIN VICODIN ES VICODIN HP VIRTUSSIN AC Other medications, used primarily to -

Use of Antitussives After the Initiation of Angiotensin-Converting Enzyme Inhibitors
저작자표시-비영리-변경금지 2.0 대한민국 이용자는 아래의 조건을 따르는 경우에 한하여 자유롭게 l 이 저작물을 복제, 배포, 전송, 전시, 공연 및 방송할 수 있습니다. 다음과 같은 조건을 따라야 합니다: 저작자표시. 귀하는 원저작자를 표시하여야 합니다. 비영리. 귀하는 이 저작물을 영리 목적으로 이용할 수 없습니다. 변경금지. 귀하는 이 저작물을 개작, 변형 또는 가공할 수 없습니다. l 귀하는, 이 저작물의 재이용이나 배포의 경우, 이 저작물에 적용된 이용허락조건 을 명확하게 나타내어야 합니다. l 저작권자로부터 별도의 허가를 받으면 이러한 조건들은 적용되지 않습니다. 저작권법에 따른 이용자의 권리는 위의 내용에 의하여 영향을 받지 않습니다. 이것은 이용허락규약(Legal Code)을 이해하기 쉽게 요약한 것입니다. Disclaimer 약학 석사학위 논문 안지오텐신 전환 효소 억제제 개시 이후 진해제의 사용 분석 Use of Antitussives After the Initiation of Angiotensin-Converting Enzyme Inhibitors 2017년 8월 서울대학교 대학원 약학과 사회약학전공 권 익 태 안지오텐신 전환 효소 억제제 개시 이후 진해제의 사용 분석 Use of Antitussives After the Initiation of Angiotensin-Converting Enzyme Inhibitors 지도교수 홍 송 희 이 논문을 권익태 석사학위논문으로 제출함 2017년 4월 서울대학교 대학원 약학과 사회약학전공 권 익 태 권익태의 석사학위논문을 인준함 2017년 6월 위 원 장 (인) 부 위 원 장 (인) 위 원 (인) Abstract Use of Antitussives After the Initiation of Angiotensin-Converting Enzyme Inhibitors Ik Tae Kwon Department of Social Pharmacy College of Pharmacy, Seoul National University Background Angiotensin-converting enzyme inhibitors (ACEI) can induce a dry cough, more frequently among Asians. If healthcare professionals fail to detect coughs induced by an ACEI, patients are at risk of getting antitussives inappropriately instead of discontinuing ACEI. The purpose of this study was to examine how the initiation of ACEI affects the likelihood of antitussive uses compared with the initiation of Angiotensin Receptor Blocker (ARB) and to determine the effect of the antitussive use on the duration and adherence of therapy in a Korean population.