Positive Blood Culture with Negative BCID Result Guideline
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gene Number Genera
Table 4. Location of the various genes Modified April 28, 2021 Originally modified from AAC 1999 43:2823-30 with permission from ASM Journals Gene Number Genera METHYLASES e erm(A) 11 AggregatibacterL,1, Bacteroides, Enterococcus , Haemophilusr, Helcococcus, Klebsiella, a a Listeria, Peptostreptococcus , Prevotella , Staphylococcus, Streptococcus erm(B) 39 Aggregatibacter1, Aerococcus, Bacillus, Bacteroidesa, Campylobacteraf, a Citrobacter, Corynebacterium, Clostridium , Clostridioides, Enterobacter, Escherichia, a a Eubacterium , Enterococcus, Fusobacterium , Gallibacteriumcp, Gemella, Haemophilus, Klebsiella, a Lactobacillus, Listeriacc, Micrococcus, Neisseria, Pantoea, Pediococcus, Peptostreptococcus , a a Porphyromonas , Proteus, Pseudomonas, Rothia, Ruminococcus , Salmonellacn, Serratia, Shigella ag, Staphylococcus, Streptococcus, UreaplasmaO, Wollinellaa, Treponemab, Trueperella1 a erm(C) 38 Aeromonasy, AggregatibacterL, Actinomyces, Bacillus, Bacteroides , Brevundimonas y, Burkholderia y, Campylobacter, Capnocytophagaa,ca ,Chryseomonasy, ,Corynebacterium, n a Clostridiuma,n Escherichia , Eubacterium , Enterococcus, Fusobacteriuma,br, Haemophilusr, y y Lactobacillus, Listeria, Macrococcus, Micrococcus, Neisseria, Paenibacillus , Pasteurella , a a Prevotella , Peptostreptococcus , Pseudomonasy, Pseudoramibactera,br, Rhizobiumy, Salmonella, y y y Serratia, Sinorhizobium , Sphingomonas , Stenotrophomans , Staphylococcus, Streptococcus, a Trueperella n, Wolinella erm(D) 2 Bacillus, Salmonella a a a a n erm(E) 7 Bacteroides , Eubacterium -

The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio In
microorganisms Review The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio in the Treatment of Obesity and Inflammatory Bowel disease Spase Stojanov 1,2, Aleš Berlec 1,2 and Borut Štrukelj 1,2,* 1 Faculty of Pharmacy, University of Ljubljana, SI-1000 Ljubljana, Slovenia; [email protected] (S.S.); [email protected] (A.B.) 2 Department of Biotechnology, Jožef Stefan Institute, SI-1000 Ljubljana, Slovenia * Correspondence: borut.strukelj@ffa.uni-lj.si Received: 16 September 2020; Accepted: 31 October 2020; Published: 1 November 2020 Abstract: The two most important bacterial phyla in the gastrointestinal tract, Firmicutes and Bacteroidetes, have gained much attention in recent years. The Firmicutes/Bacteroidetes (F/B) ratio is widely accepted to have an important influence in maintaining normal intestinal homeostasis. Increased or decreased F/B ratio is regarded as dysbiosis, whereby the former is usually observed with obesity, and the latter with inflammatory bowel disease (IBD). Probiotics as live microorganisms can confer health benefits to the host when administered in adequate amounts. There is considerable evidence of their nutritional and immunosuppressive properties including reports that elucidate the association of probiotics with the F/B ratio, obesity, and IBD. Orally administered probiotics can contribute to the restoration of dysbiotic microbiota and to the prevention of obesity or IBD. However, as the effects of different probiotics on the F/B ratio differ, selecting the appropriate species or mixture is crucial. The most commonly tested probiotics for modifying the F/B ratio and treating obesity and IBD are from the genus Lactobacillus. In this paper, we review the effects of probiotics on the F/B ratio that lead to weight loss or immunosuppression. -

Current Trends of Enterococci in Dairy Products: a Comprehensive Review of Their Multiple Roles
foods Review Current Trends of Enterococci in Dairy Products: A Comprehensive Review of Their Multiple Roles Maria de Lurdes Enes Dapkevicius 1,2,* , Bruna Sgardioli 1,2 , Sandra P. A. Câmara 1,2, Patrícia Poeta 3,4 and Francisco Xavier Malcata 5,6,* 1 Faculty of Agricultural and Environmental Sciences, University of the Azores, 9700-042 Angra do Heroísmo, Portugal; [email protected] (B.S.); [email protected] (S.P.A.C.) 2 Institute of Agricultural and Environmental Research and Technology (IITAA), University of the Azores, 9700-042 Angra do Heroísmo, Portugal 3 Microbiology and Antibiotic Resistance Team (MicroART), Department of Veterinary Sciences, University of Trás-os-Montes and Alto Douro (UTAD), 5001-801 Vila Real, Portugal; [email protected] 4 Associated Laboratory for Green Chemistry (LAQV-REQUIMTE), University NOVA of Lisboa, 2829-516 Lisboa, Portugal 5 LEPABE—Laboratory for Process Engineering, Environment, Biotechnology and Energy, Faculty of Engineering, University of Porto, 420-465 Porto, Portugal 6 FEUP—Faculty of Engineering, University of Porto, 4200-465 Porto, Portugal * Correspondence: [email protected] (M.d.L.E.D.); [email protected] (F.X.M.) Abstract: As a genus that has evolved for resistance against adverse environmental factors and that readily exchanges genetic elements, enterococci are well adapted to the cheese environment and may reach high numbers in artisanal cheeses. Their metabolites impact cheese flavor, texture, Citation: Dapkevicius, M.d.L.E.; and rheological properties, thus contributing to the development of its typical sensorial properties. Sgardioli, B.; Câmara, S.P.A.; Poeta, P.; Due to their antimicrobial activity, enterococci modulate the cheese microbiota, stimulate autoly- Malcata, F.X. -
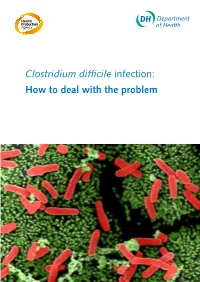
Clostridium Difficile Infection: How to Deal with the Problem DH INFORMATION RE ADER B OX
Clostridium difficile infection: How to deal with the problem DH INFORMATION RE ADER B OX Policy Estates HR / Workforce Commissioning Management IM & T Planning / Finance Clinical Social Care / Partnership Working Document Purpose Best Practice Guidance Gateway Reference 9833 Title Clostridium difficile infection: How to deal with the problem Author DH and HPA Publication Date December 2008 Target Audience PCT CEs, NHS Trust CEs, SHA CEs, Care Trust CEs, Medical Directors, Directors of PH, Directors of Nursing, PCT PEC Chairs, NHS Trust Board Chairs, Special HA CEs, Directors of Infection Prevention and Control, Infection Control Teams, Health Protection Units, Chief Pharmacists Circulation List Description This guidance outlines newer evidence and approaches to delivering good infection control and environmental hygiene. It updates the 1994 guidance and takes into account a national framework for clinical governance which did not exist in 1994. Cross Ref N/A Superseded Docs Clostridium difficile Infection Prevention and Management (1994) Action Required CEs to consider with DIPCs and other colleagues Timing N/A Contact Details Healthcare Associated Infection and Antimicrobial Resistance Department of Health Room 528, Wellington House 133-155 Waterloo Road London SE1 8UG For Recipient's Use Front cover image: Clostridium difficile attached to intestinal cells. Reproduced courtesy of Dr Jan Hobot, Cardiff University School of Medicine. Clostridium difficile infection: How to deal with the problem Contents Foreword 1 Scope and purpose 2 Introduction 3 Why did CDI increase? 4 Approach to compiling the guidance 6 What is new in this guidance? 7 Core Guidance Key recommendations 9 Grading of recommendations 11 Summary of healthcare recommendations 12 1. -

Infective Endocarditis Caused by C. Sordellii: the First Case Report from India
Published online: 2021-05-19 THIEME 74 C.Case sordellii Report in Endocarditis Chaudhry et al. Infective Endocarditis Caused by C. sordellii: The First Case Report from India Rama Chaudhry1 Tej Bahadur1 Tanu Sagar1 Sonu Kumari Agrawal1 Nazneen Arif1 Shiv K. Choudhary2 Nishant Verma1 1Department of Microbiology, All India Institute of Medical Address for correspondence Dr. Rama Chaudhry, MD, Department Sciences, New Delhi, India of Microbiology, All India Institute of Medical Sciences, Ansari Nagar, 2Department of Cardiothoracic and Vascular Surgery, All India New Delhi 110029, India (e-mail: [email protected]). Institute of Medical Sciences, New Delhi, India J Lab Physicians 2021;13:74–76. Abstract Clostridium sordellii is a gram-positive anaerobic bacteria most commonly isolated Keywords from skin and soft tissue infection, penetrating injurious and intravenous drug abus- ► infective endocarditis ers. The exotoxins produced by the bacteria are associated with toxic shock syndrome. ► Clostridium sordellii We report here a first case of infective endocarditis due to C. sordellii from a female ► diagnosis patient with ventricular septal defect from India. Introduction admitted to the cardiothoracic vascular surgery ward of All India Institute of Medical Sciences (AIIMS), New Delhi, India Anaerobes are major components of the normal micro- with complaints of worsening shortness of breath and pal- bial flora present on human skin and mucosa. Infections pitations. Patient reported having an episode of IE 3 months due to anaerobic bacteria are common, but they are dif- back for which she had been admitted to AIIMS and was ficult to isolate from infected sites and are often over- discharged after treatment. -

Methicillin-Resistant Staphylococcus Aureus (MRSA)
Methicillin-Resistant Staphylococcus Aureus (MRSA) Over the past several decades, the incidence of resistant gram-positive organisms has risen in the United States. MRSA strains, first identified in the 1960s in England, were first observed in the U.S. in the mid 1980s.1 Resistance quickly developed, increasing from 2.4% in 1979 to 29% in 1991.2 The current prevalence for MRSA in hospitals and other facilities ranges from <10% to 65%. In 1999, MRSA accounted for more than 50% of all Staphylococcus aureus isolates within U.S. intensive care units.3, 4 The past years, however, outbreaks of MRSA have also been seen in the community setting, particularly among preschool-age children, some of whom have attended day-care centers.5, 6, 7 MRSA does not appear to be more virulent than methicillin-sensitive Staphylococcus aureus, but certainly poses a greater treatment challenge. MRSA also has been associated with higher hospital costs and mortality.8 Within a decade of its development, methicillin resistance to Staphylococcus aureus emerged.9 MRSA strains generally are now resistant to other antimicrobial classes including aminoglycosides, beta-lactams, carbapenems, cephalosporins, fluoroquinolones and macrolides.10,11 Most of the resistance was secondary to production of beta-lactamase enzymes or intrinsic resistance with alterations in penicillin-binding proteins. Staphylococcus aureus is the most frequent cause of nosocomial pneumonia and surgical- wound infections and the second most common cause of nosocomial bloodstream infections.12 Long-term care facilities (LTCFs) have developed rates of MRSA ranging from 25%-35%. MRSA rates may be higher in LTCFs if they are associated with hospitals that have higher rates.13 Transmission of MRSA generally occurs through direct or indirect contact with a reservoir. -

Use of the Diagnostic Bacteriology Laboratory: a Practical Review for the Clinician
148 Postgrad Med J 2001;77:148–156 REVIEWS Postgrad Med J: first published as 10.1136/pmj.77.905.148 on 1 March 2001. Downloaded from Use of the diagnostic bacteriology laboratory: a practical review for the clinician W J Steinbach, A K Shetty Lucile Salter Packard Children’s Hospital at EVective utilisation and understanding of the Stanford, Stanford Box 1: Gram stain technique University School of clinical bacteriology laboratory can greatly aid Medicine, 725 Welch in the diagnosis of infectious diseases. Al- (1) Air dry specimen and fix with Road, Palo Alto, though described more than a century ago, the methanol or heat. California, USA 94304, Gram stain remains the most frequently used (2) Add crystal violet stain. USA rapid diagnostic test, and in conjunction with W J Steinbach various biochemical tests is the cornerstone of (3) Rinse with water to wash unbound A K Shetty the clinical laboratory. First described by Dan- dye, add mordant (for example, iodine: 12 potassium iodide). Correspondence to: ish pathologist Christian Gram in 1884 and Dr Steinbach later slightly modified, the Gram stain easily (4) After waiting 30–60 seconds, rinse with [email protected] divides bacteria into two groups, Gram positive water. Submitted 27 March 2000 and Gram negative, on the basis of their cell (5) Add decolorising solvent (ethanol or Accepted 5 June 2000 wall and cell membrane permeability to acetone) to remove unbound dye. Growth on artificial medium Obligate intracellular (6) Counterstain with safranin. Chlamydia Legionella Gram positive bacteria stain blue Coxiella Ehrlichia Rickettsia (retained crystal violet). -

Complete Genome Sequences of Two Enterococcus Faecium Strains and Comparative Genomic Analysis
EXPERIMENTAL AND THERAPEUTIC MEDICINE 19: 2019-2028, 2020 Complete genome sequences of two Enterococcus faecium strains and comparative genomic analysis YONG‑QI GAN, TAO ZHANG, YONG‑QIANG GAN, ZHUANG ZHAO and BIN ZHU Guangxi Institute for Food and Drug Control, Nanning, Guangxi Zhuang Autonomous Region 530021, P.R. China Received December 1, 2018; Accepted August 12, 2019 DOI: 10.3892/etm.2020.8447 Abstract. Enterococci are used for improvement of the intes- environment when treating bacterial diarrhea (3). There are tinal environment and have clinical benefits. Enterococcus two main advantages to Enterococcus that make it the most faecalis and Enterococcus faecium have similar morpholo- popular edible probiotic in animals and humans: i) In the gies, leading to confusion between the two species. In order gastrointestinal (GI) tract, Enterococcus competes with patho- to identify the National Institute for Food and Drug Control gens and thus decreases their virulence (2); ii) Enterococcus (strain 140623) and Shin Biofermin S (strain SBS-1, one of resists acid stress and cannot be digested by GI‑secreted diges- the cocci), which are widely used clinically, the present study tive juice (4). E. faecalis and E. faecium are used as digestive sequenced and analyzed these two strains. The biochemical agents for the treatment of diarrhea caused by flatulence characteristics, gas chromatography and mass spectrometry and indigestion (2). However, these two bacteria are difficult results of 140623 and SBS-1 revealed that the two strains were to distinguish morphologically. Species identification and more similar to E. faecium than E. faecalis. The genomes of genome characterization of these strains may elucidate thera- 140623 and SBS-1 contained 2,812,926 bp and 2,797,745 bp, peutic strategies for bacterial infection and probiotic treatment respectively, based on Illumina HiSeq 2000 sequencing. -

Transfer of Streptococcus Faecalis and Streptococcus Faecium to the Genus Enterococcus Norn
INTERNATIONALJOURNAL OF SYSTEMATICBACTERIOLOGY, Jan. 1984, p. 31-34 Vol. 34, No. 1 OO20-7713/84/010031-04$02.00/0 Copyright 0 1984, International Union of Microbiological Societies Transfer of Streptococcus faecalis and Streptococcus faecium to the Genus Enterococcus norn. rev. as Enterococcus faecalis comb. nov. and Enterococcus faecium comb. nov. KARL H. SCHLEIFER* AND RENATE KILPPER-BALZ Lehrstuhl fur Mikrobiologie, Technische Universitat Miinchen, D-8000 Miinchen 2, Federal Republic of Germany The results of deoxyribonucleic acid-deoxyribonucleic acid and deoxyribonucleic acid-ribosomal ribonu- cleic acid hybridization studies demonstrated that Streptococcus faecalis and Streptococcus faecium are distantly related to the non-enterococcal streptococci (Streptococcus hovis and Streptococcus equinus) of serological group D and to other streptococci. On the basis of our results and those of previous studies, we propose that S. faecalis and S. faecium be transferred to the genus Enterococcus (ex Thiercelin and Jouhaud) nom. rev. as Enterococcus faecalis (Andrewes and Horder) comb. nov. and Enterococcus faecium (Orla-Jensen) comb. nov., respectively. A description of the genus Enterococcus nom. rev. and emended descriptions of E. faecalis and E. faecium are given. The streptococci belonging to serological group D can be De Ley (4) and were corrected to the value for the reference divided into two physiologically different groups. Strepto- Escherichia coli K-12 DNA. coccus faecalis and Streptococcus faecium were placed in the enterococcus division of the streptococci, whereas RESULTS AND DISCUSSION Streptococcus bovis and Streptococcus equinus were placed in the viridans division by Sherman (21). Kalina proposed (9) The DNA base compositions, serological groups, and that Streptococcus faecalis and Streptococcus faecium peptidoglycan types of the test strains are shown in Table 1. -

Identification, Properties, and Application of Enterocins Produced by Enterococcal Isolates from Foods
IDENTIFICATION, PROPERTIES, AND APPLICATION OF ENTEROCINS PRODUCED BY ENTEROCOCCAL ISOLATES FROM FOODS THESIS Presented in Partial Fulfillment of the Requirement for the Degree Master of Science in the Graduate School of The Ohio State University By Xueying Zhang, B.S. ***** The Ohio State University 2008 Master Committee: Approved by Professor Ahmed E. Yousef, Advisor Professor Hua Wang __________________________ Professor Luis Rodriguez-Saona Advisor Food Science and Nutrition ABSTRACT Bacteriocins produced by lactic acid bacteria have gained great attention because they have potentials for use as natural preservatives to improve food safety and stability. The objectives of the present study were to (1) screen foods and food products for lactic acid bacteria with antimicrobial activity against Gram-positive bacteria, (2) investigate virulence factors and antibiotic resistance among bacteriocin-producing enterooccal isolates, (3) characterize the antimicrobial agents and their structural gene, and (4) explore the feasibility of using these bacteriocins as food preservatives. In search for food-grade bacteriocin-producing bacteria that are active against spoilage and pathogenic microorganisms, various commercial food products were screened and fifty-one promising Gram-positive isolates were studied. Among them, fourteen food isolates with antimicrobial activity against food-borne pathogenic bacteria, Listeria monocytogenes and Bacillus cereus, were chosen for further study. Based on 16S ribosomal RNA gene sequence analysis, fourteen food isolates were identified as Enterococcus faecalis, and these enterococcal isolates were investigated for the presence of virulence factors and antibiotic resistance through genotypic and phenotypic screening. Results indicated that isolates encoded some combination of virulence factors. The esp gene, encoding extracellular surface protein, was not detected in any of the isolates. -

Identification and Antimicrobial Susceptibility Testing of Anaerobic
antibiotics Review Identification and Antimicrobial Susceptibility Testing of Anaerobic Bacteria: Rubik’s Cube of Clinical Microbiology? Márió Gajdács 1,*, Gabriella Spengler 1 and Edit Urbán 2 1 Department of Medical Microbiology and Immunobiology, Faculty of Medicine, University of Szeged, 6720 Szeged, Hungary; [email protected] 2 Institute of Clinical Microbiology, Faculty of Medicine, University of Szeged, 6725 Szeged, Hungary; [email protected] * Correspondence: [email protected]; Tel.: +36-62-342-843 Academic Editor: Leonard Amaral Received: 28 September 2017; Accepted: 3 November 2017; Published: 7 November 2017 Abstract: Anaerobic bacteria have pivotal roles in the microbiota of humans and they are significant infectious agents involved in many pathological processes, both in immunocompetent and immunocompromised individuals. Their isolation, cultivation and correct identification differs significantly from the workup of aerobic species, although the use of new technologies (e.g., matrix-assisted laser desorption/ionization time-of-flight mass spectrometry, whole genome sequencing) changed anaerobic diagnostics dramatically. In the past, antimicrobial susceptibility of these microorganisms showed predictable patterns and empirical therapy could be safely administered but recently a steady and clear increase in the resistance for several important drugs (β-lactams, clindamycin) has been observed worldwide. For this reason, antimicrobial susceptibility testing of anaerobic isolates for surveillance -
Testing, Surveillance and Management of Clostridium Difficile
Annex C: Testing, Surveillance and Management of Clostridium difficile In All Health Care Settings Provincial Infectious Diseases Advisory Committee (PIDAC) Revised: January 2013 The Ontario Agency for Health Protection and Promotion (Public Health Ontario) is a Crown corporation dedicated to protecting and promoting the health of all Ontarians and reducing inequities in health. As a hub organization, Public Health Ontario links public health practitioners, front-line health workers and researchers to the best scientific intelligence and knowledge from around the world. Public Health Ontario provides expert scientific and technical support relating to communicable and infectious diseases; surveillance and epidemiology; health promotion, chronic disease and injury prevention; environmental and occupational health; health emergency preparedness; and public health laboratory services to support health providers, the public health system and partner ministries in making informed decisions and taking informed action to improve the health and security of Ontarians. The Provincial Infectious Diseases Advisory Committee on Infection Prevention and Control (PIDAC-IPC) is a multidisciplinary committee of health care professionals with expertise and experience in Infection Prevention and Control. The committee advises Public Health Ontario on the prevention and control of health care associated infections, considering the entire health care system for protection of both clients/patients/residents and health care providers. PIDAC-IPC produces “best practice” knowledge products that are evidence-based, to the largest extent possible, to assist health care organizations in improving quality of care and client/patient/resident safety. Disclaimer for Best Practice Documents This document was developed by the Provincial Infectious Diseases Advisory Committee on Infection Prevention and Control (PIDAC-IPC).