Association of Environmental Factors and High HFMD Occurrence In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chiang Rai Tea in 2019, the Production Area of Tea in Chiang
Chiang Rai Tea In 2019, the production area of tea in Chiang Rai Province is 84,118 rais, harvesting area of 80,043 rai and average yield (fresh tea leaves) that farmers can harvest are 1,063 kilograms per rai. The total yield is 85,104 tons. The major tea production areas in Chiang Rai Provice are Wiang Pa Pao District, Mae Fah Luang District, Mae Suai District, Mueang Chiang Rai District, Thoeng District, Phan District and Mae Lao District. Map showing the major tea plantation areas in Chiang Rai Province MaeSaiDiMae Sai strictDistrict Mae Fa Luang District Chiang Saen District Mae Chan District Chiang Doi Luang Khong District District Wiang Chiang Wiang Rung District Kaen District Phaya Muang Chiang Rai District Wiang Chai Mengrai District District Mae Lao District Mae Suai District Thoeng District Phan District Pa Daet District Wiang Pa Pao District Tea production of Chiang Rai Province in 2019 (Source : Chiang Rai Provincial Agricultural Extension Office) Plantation Harvesting Average Yield of Yield of Fresh No. District Area Area Fresh Tea Leaves Tea Leaves (rai) (rai) (kilogram/rai) (ton) 1 Mueang Chiang Rai 3,706 3,146 1,050 3,303 2 Mae Suai 21,883 21,720 1,050 22,806 3 Wiang Pa Pao 30,959 30,929 970 30,001 4 Mae Fa Luang 26,354 23,032 1,200 27,638 5 Thoeng 121 121 900 109 6 Phan 265 265 1,100 292 7 Mae Lao 830 830 1,150 955 Total 84,118 80,043 1,063 85,104 Tea that are grown in Chiang Rai Province are divided into 2 varieties: 1. -

The Study on the Development of the Participatory Management Of
The Study on the Development of the Participatory Management of Occupational Group that Affects the Sustainable Development of Mae Chan Tai Community, Mae Suai District, Chiang Rai Province กำรศึกษำแนวทำงพัฒนำกำรบริหำรจัดกำรกลุ่มอำชีพอย่ำงมีส่วนร่วมที่ส่งผลต่อกำรพัฒนำ อย่ำงยั่งยืนของชุมชนแม่จันใต้ อ�ำเภอแม่สรวย จังหวัดเชียงรำย Sutheemon Chongesiriroj1 and Chanchai Bunchapatanasakda2 สุธีมนต์ ทรงศิริโรจน์1 และ ชาญชัย บัญชาพัฒนาศักดา2 1Doctor of Business Administration Program, Shinawatra University 1หลักสูตรบริหารธุรกิจดุษฎีบัณฑิต มหาวิทยาลัยชินวัตร 2School of Management, Shinawatra University 2คณะการจัดการ มหาวิทยาลัยชินวัตร Received: February 7, 2019 Revised: March 13, 2019 Accepted: March 13, 2019 Abstract This research is a mixed methods research on both qualitative and quantitative research which aims to study the participatory management of the occupational group and the potential development guidelines, which can bring the knowledge to develop the management pattern and the strategies for promoting the community sustainable development. Sample consisted of 36 households. The research found out that the management of the occupational group (POSDCoRB) in overall is in high level. Anyway, in each aspect, it was found that the opinions with the highest level towards the budgeting and the other aspects were rated as high level such as staffing, reporting, directing, planning, organizing, and coordinating respectively. The guidelines for the participatory development of the occupational group that affecting the potential sustainable development -

Thanapiriya Public Company Limited (TNP)
- Information Memorandum – Thanapiriya Public Company Limited (TNP) Head Office 661 Moo. 24 Rop Wiang, Muang, Chiang Rai 57000 Tel. +66 53 756 484 Fax: +66 53 756 484 Website: www.thanapiriya.co.th Listing Date As of 18 November 2015 (Trading commencement on 18 November 2015) Listing Securities 800 million common shares with par value of 0.25 Baht per share, total value of 200 million Baht Capital As of 18 November 2015 (Trading commencement) Registered Capital; Common Shares 200 million Baht (800 million shares) Paid-up Capital; Common Shares 200 million Baht (800 million shares) Secondary Market Market Alternative of Investment (mai) Offering Price 1.75 Baht Offering Date 11 - 13 November 2015 (The Company issues common shares to the public 200 million shares) Objectives and plans for utilizing the capital increase Amount Use of proceeds Estimated timing (million Baht) 1. Financing business expansion 245.00 Within 2016 2. Retiring bank loan 70.00 Within 2015 3. Using as working capital 19.41 Within 2015 - 2016 Total 334.41 Note: The capital increase in the amount of 350.00 million Baht, deduct an expenses in the amount of 15.59 million Baht, net proceeds in the amount of 334.41 million Baht. Green Shoe Option -None- Page 1 Type of Business and Nature of Operation Thanapiriya Public Company Limited (“The Company”) is a retailer and a wholesaler of consumer goods excluding fresh food under the name “Thanapiriya”. The major revenue is from store sales and the head office sales accounted for 75 percent and 25 percent of total sales revenue respectively. -

Using Multiple Criteria Decision Makingv (Mcdm) to Location Selection for Grass Flower Warehouse in Chiang Rai Province, Thailand
USING MULTIPLE CRITERIA DECISION MAKINGV (MCDM) TO LOCATION SELECTION FOR GRASS FLOWER WAREHOUSE IN CHIANG RAI PROVINCE, THAILAND Martusorn Khaengkhan College of Logistics and Supply Chain ,Suansunandha Rajabhat University 111/3-5 Phuttamonthon District, Nakhon Paththom,Thailand 73170 Email:[email protected], [email protected] ABSTRACT The purpose of this paper is to select warehouse location of grass flowers in Chiang Rai province Using Multiple Criteria Decision Making (MCDM) the three method for Simple Additive Weighting (SAW) Method, Order Preference by Similarity to Ideal Solution (TOPSIS) and The Analytic Hierarchy Process (AHP). For selected of grass flowers location warehouse in Chiang Rai Province.The entrepreneurs of grass flowers trading need to increase warehouse building to meet customer satisfaction. Thus, this paper is to surveyed 7 criteria of the entrepreneurs consist of size of property, property cost, labor cost, public utility, mode of transportation, ability to access of location and distance from supplier and investigated locating in 4 districts area using conjunctive constrain method to screen the alternative consist of Mae Jan district, Mae Sai district, Chiang Saen district and Chiang Khong district were used to selection. The decisions making of location selection used by SAW, TOPSIS and AHP, the result of this paper found that Tambon Pa Sang, Mae Chan district is appropriate located for building grass flowers warehouse in Chiang Rai province. Keywords: AHP, TOPSIS, SAW, Location Selection INTRODUCTION Regarding the necessity of the inventory, entrepreneurs may not want the much inventory in the stock because of the economic liquidity and the cost of the organization. But, in terms of inefficient logistic management and range and duration of transportation management, there will have the space of time condition. -

Regional Development of the Golden and Emerald Triangle Areas: Thai Perspective
CHAPTER 6 Regional Development of the Golden and Emerald Triangle Areas: Thai Perspective Nucharee Supatn This chapter should be cited as: Supatn, Nucharee, 2012. “Regional Development of the Golden and Emerald Triangle Areas: Thai Perspective.” In Five Triangle Areas in The Greater Mekong Subregion, edited by Masami Ishida, BRC Research Report No.11, Bangkok Research Center, IDE- JETRO, Bangkok, Thailand. CHAPTER 6 REGIONAL DEVELOPMENT OF THE GOLDEN AND EMERALD TRIANGLE AREAS: THAI PERSPECTIVES Nucharee Supatn INTRODUCTION Regarding international cooperation in the Greater Mekong Sub-region, two triangle areas of the three bordering countries also exist in Thailand. The first is known as the “Golden Triangle” of Myanmar, Lao PDR, and Thailand. It was known as the land of opium and the drug trade in a previous era. The second, the “Emerald Triangle,” includes areas of Cambodia, Lao PDR, and Thailand. In addition, there is also the “Quadrangle Area” of China, Lao PDR, Myanmar, and Thailand which is an extension of the Golden Triangle. Though there is no border between China and Thailand, there is cooperation in trading, drug and criminal control, and also the development of regional infrastructure, especially in the North-South Economic Corridor (NSEC) and the 4th Thai-Laos Friendship Bridge which is currently under construction. Figure 1 shows the location of the two triangles. The circled area indicates the Golden Triangle, which is located in the upper-north of Thailand, whereas the Emerald Triangle is in the northeastern region of the country. However, as these two triangles are located in different regions of Thailand with different characteristics and contexts, the discussions of each region are presented separately. -
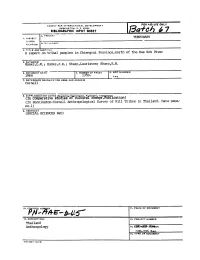
R International Development for Aid Use Onl Washington, D
AGENCY FOR INTERNATIONAL DEVELOPMENT FOR AID USE ONL WASHINGTON, D. C. 20523 BIBLIOGRAPHIC INPUT SHEET r________ lo_7 A..'.,J"J., TEMPORARY FI(.ATION h 2. TITLE AND SUBTITLE A report on tribal peoples in Chiengrai Province,north of the Mae Kok River 3. AUTHOR(S) Hanks,L.M.; Hanks,J.R.; Sharp,Lauriston; Sharp,R.B. 4. DOCUMENT DATE I S.NUMBER OF PAGES 6. ARC NUMBER 1964 135p. ARC 7. REFERENCE ORGANIZATION NAME AND ADDRESS Cornell 8. SUPPLEMENTARY 14OTES Spo1fo1n Or.anlzgj £fbft 0?8. AVflIib ict ion) (Incomparative s u -es o culturaT cnange. (In Bennington-Cornell Anthropological Survey of Hill Tribes in Thailand. Data pape" no.1) 9. ABSTRACT (SOCIAL SCIENCES R&D) 10. CITLNUER II. PRICE OF DOCUMENT 12. DESCRIPTORS 13. PROJECT NUMBER Thailand Anthropology 14. 10& a6RIIR r MMrn9o94 RAA_ 15. TYPE OF DOCUMENT AID 590-1 (4-74) Bennington - Cornell Anthropological Survey of Hill Tribes in Thailand A REPORT ON TRIBAL PEOPLES IN ,CHIENGRAI PROVINCE NORTH OF THE MAE KOK RIVER by Lucien M. Hanks Jane R. Hanks Lauriston Sharp Ruth B. Sharp Comparative Studies of Cultural Change Department of Anthropology Cornell University Ithaca, New York 1964 Orr .L.L40 INTRODUCTION In 1963, the Department of Anthropology at Cornell University contracted with the Agency for International Development to conduct applied social science research. A principal goal of this research is to aid foreign government officials and Agency for International Develop ment project administrators, technicians, policy and program planners to arrive at sound policy decisions through a better understanding of the total socio-economic context of the problems to be solved. -

TONAL VARIATION in the LUE DIALECTS of THAILAND Kanita
TONAL VARIATION IN THE (1) A1-2-3-4 (A1=A3, A2=A4), LUE DIALECTS OF comprising patterns 1 and 6; (2) A1-23-4, comprising patterns 2 and 7, THAILAND (3) A1-234, comprising patterns 3 and 8, (4) A12-34, comprising pattern 4; and 1 Kanita Chaimano (5) A123-4, comprising patterns 5 and 9. The tonal system and tone features of Abstract pattern 3/2 were found to be distributed widely in many provinces (Chiang Mai, This study analyzes the tonal variation of Lamphun, Lampang, and Nan). The tonal Lue dialects spoken in Thailand. These system and tone features of patterns 5/1 dialects are classified into groups based and 8/2 are found in Chiang Rai province; on structural differences in their tonal and those of patterns 4 and 7/1, in Chiang systems, and this classification then forms Mai province. the basis for a linguistic map of Thailand’s Lue dialects. The data were collected from Introduction 45 villages in 7 provinces in the northern part of Thailand. Three informants were According to Ruengdet Pankhuenkhat’s selected to represent each village, for a (1988) classification of the Tai language total of 135 informants participating in family, Lue has two main dialects: Lue this research. William J.Gedney’s (1972) and Yong. Some linguists identify the Lue wordlist was used to elicit tonal data. The and the Yong as belonging to a single tonal features of the dialects were ethnic group. Indeed linguistically, the analyzed using auditory information and Yong living in Thailand are of the same the personal computer programs “PRAAT, group as the Lue, but both of them call ver.4.5.12” and Microsoft Excel. -
Chiangrai.Compressed.Pdf
Cover Chiang Rai Eng nt.indd 1 12/28/10 4:25:11 PM Useful Calls Public Relations Office Tel: 0 5371 1870 Provincial Office Tel: 0 5371 1123 Chiang Rai District Office Tel: 0 5375 2177, 0 5371 1288 Chiang Rai Hospital Tel: 0 5371 1300 Mueang Chiang Rai District Police Station Tel: 0 5371 1444 Highway Police Tel: 1193 Tourist Police Tel: 0 5371 7779, 1155 Immigration Tel: 0 2287 3101-10 Mae Sai Immigration Tel: 0 5373 1008-9 Chiang Saen Immigration Tel: 0 5379 1330 Meteorological Department Tel: 1182 Tourism and Sports Office Tel: 0 5371 6519 Chiang Rai Tourism Association Tel: 0 5360 1299 TAT Tourist Information Centers Tourism Authority of Thailand Head Office 1600 Phetchaburi Road, Makkasan, Ratchathewi, Bangkok 10400 Tel: 0 2250 5500 (automatic 120 lines) Fax: 0 2250 5511 E-mail: [email protected] www.tourismthailand.org Ministry of Tourism and Sports 4 Ratchadamnoen Nok Avenue, Bangkok 10100 8.30 a.m.-4.30 p.m. everyday TAT Chiang Rai 448/16 Singhakhlai Road, Amphoe Mueang Chiang Rai, Chiang Rai 57000 Tel: 0 5371 7433, 0 5374 4674-5 Fax: 0 5371 7434 E-mail: [email protected] Areas of Responsibility: Chiang Rai, Phayao King Mengrai the Great Memorial Cover Chiang Rai Eng nt.indd 2 12/28/10 3:49:27 PM 003-066 Chiang Rai nt.indd 2 12/25/10003-066 2:46:22 Chiang PM Rai nt.indd 67 12/25/10 9:58:54 AM CONTENTS HOW TO GET THERE 5 ATTRACTIONS 7 Amphoe Mueang Chiang Rai 7 Amphoe Mae Lao 12 Amphoe Mae Chan 13 Amphoe Mae Sai 15 Amphoe Mae Fa Luang 16 Amphoe Chiang Saen 19 Amphoe Chiang Khong 22 Amphoe Wiang Kaen 23 Amphoe Thoeng 23 Amphoe Phan 24 -

Epidemiology of the Hill Tribe HIV/AIDS Populations, Thailand
Epidemiology of the Hill Tribe HIV/AIDS Populations, Thailand Tawatchai Apidechkul DrPH (Epidemiology)*,** * School of Health Science, Mae Fah Luang University, Chiang Rai, Thailand ** Center of Excellence for the Hill tribe Research, Mae Fah Luang University, Chiang Rai, Thailand Objective: A retrospective cohort study was conducted to determine the situation and factors related to the death among the HIV/AIDS Hill tribe in Northern Thailand. Material and Method: A systematic data-reviewing approach was used to identify the information from the rosters of ARV clinics, OPD cards, and laboratory reports from 16 hospitals in Chiang Rai Province, Thailand. The data were collected from the first reported HIV/AIDS case of the Hill tribe to the end of 2010. A logistic regression models were used to identify associations. A p-value <0.05 was considered as a statistical significance in multiple logistic regression models. Results: Three thousand one hundred thirty cases were included in the present study. The majority of patients were Akha (46.0%) followed by Lahu (19.7%), 54.6% were males, 44.6% were 26 to 35 years old. The major risk factor of HIV infection was sexual intercourse (91.7%); 33.3% were still alive at the date of data collection, 30.7% were diagnosed with pulmonary TB. Regarding survival status, females had a better surviving rate than males with adjusted OR = 1.41, 95% CI = 1.19-1.66. Those that had the route of transmission as “mother-to-child” and “IDU” had greater chance of survival compared to those who contracted HIV from “sexual intercourse”, with adjusted OR = 2.05, 95% CI = 1.56-2.18, and adjusted OR = 8.45, 95% CI = 1.55-46.13, respectively. -

Factor Associated with Alcohol Use Among Lahu and Akha Hill Tribe
Singkorn et al. Substance Abuse Treatment, Prevention, and Policy (2019) 14:5 https://doi.org/10.1186/s13011-019-0193-6 RESEARCH Open Access Factor associated with alcohol use among Lahu and Akha hill tribe youths, northern Thailand Onnalin Singkorn2,3, Tawatchai Apidechkul1,3*, Bukhari Putsa1, Sudkhed Detpetukyon1, Rachanee Sunsern1, Phitnaree Thutsanti3, Ratipark Tamornpark3, Panupong Upala3 and Chadaporn Inta3 Abstract Background: Alcohol use impacts several dimensions, including physical health, mental health, families, and social interactions. This study aimed to estimate the prevalence and to determine the factors associated with alcohol use among Akha and Lahu hill tribe youths in Chiang Rai, Thailand. Methods: An analytic cross-sectional design was applied to obtain key data on these associations. The study sample was Akha and Lahu hill tribe youths aged 15-24 years who lived in 30 selected hill tribe villages. A questionnaire was developed from an in-depth interview and group discussion and tested for validation and reliability before use. Descriptive statistics were used to demonstrate the general characteristics, and Chi-square test and logistic regression were used to detect associations between variables at α=0.05. Results: A total of 737 subjects were recruited into the study, of whom 50.0% were Lahu. The average age was 17.9 years, 80.7% were single, 71.1% were Christian, 65.9% graduated secondary school, and 65.7% had their major source of income from their parents. Overall, 17.3% smoked and 45.0% drank alcohol. Among the drinkers, 79.8% drank beer, 61. 5% started drinking at an age of 15-19 years, 86.8% had drank for < 5 years, 42.5% were persuaded to drink by their peers, 20.2% suffered an accident after alcohol use, and 17.2% had experienced unsafe sex after drinking alcohol. -

N. Sirimongkonlertkul / GMSARN International Journal 11 (2017) 45 - 50
N. Sirimongkonlertkul / GMSARN International Journal 11 (2017) 45 - 50 Nion Sirimongkonlertkul, Witoon Prommee, Sarawut Pongleerat and Vivarad Phonekeo Abstract— This paper studies the outcomes of new application on smart phones to solve smoke haze problem in Chiang Rai. In this application, there are three main parts including web server,android application, and users. For the web server, the automatic filter program downloads the hotspot data of only Chiang Rai every five minutes from the Earth Science Data and Information System (ESDIS) of NASA. After that, the web server updates the new hotspot data in the application installed on smart phones. This proposed application is tested between 1 January 2016 and 30 April 2016 by Protected areas regional office 15 of National Park, Wildlife and Plant Conservation Department. If the users receive warning voice from the hotspot monitoring application on their smart phone, they will plan to control fire area in this application for surveying. In surveyed results, this application can show the number of hotspots, geographic location of hotspots, land use map of burned area and 99 percent of detected hotspots are true fire. The top number of 3 hotspots is 322 in Mae Suai district. The average PM10 of Muean Chiang Rai and Mae Sai stations are to 128 µg/m and 186.74 µg/m3 which are higher than the normal AQI (Air Quantity Index of the United States Environment 3 3 Protection Agency (EPA), 120 µg/m ) in April 2016. Moreover, the maximun PM10 is to 317 µg/m at Mae Sai station. The moderate-resolution imaging spectroradiometer (MODIS) is used to study hotspots in Chiang Rai. -
Education Opportunities for Hill Tribes in Northern Thailand
RAP publication 2002/05 Case study on EDUCATION OPPORTUNITIES FOR HILL TRIBES IN NORTHERN THAILAND Implications for sustainable rural development Food and Agriculture Organization of the United Nations Regional Office for Asia and the Pacific Bangkok, Thailand 2002 The designations employed and the presentation of material in this information product do not imply the expression of any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. All rights reserved. Reproduction and dissemination of material in this information product for educational or other non-commercial purposes are authorized without any prior written permission from the copyright holders provided the source is fully acknowledged. Reproduction of material in this information product for resale or other commercial purposes is prohibited without written permission of the copyright holders. Applications for such permission should be addressed to the Senior Extension, Education and Communications Officer, FAO Regional Office for Asia and the Pacific, Maliwan Mansion, 39 Phra Athit Road, Bangkok 10200 Thailand. Photo Credits: R. Fujioka © FAO, 2002 For additional copies of this publication, please write to: Senior Extension, Education and Communications Officer FAO Regional Office for Asia and the Pacific Maliwan Mansion, 39 Phra Athit Road, Bangkok 10200 Thailand RAP publication 2002/05 Case study on EDUCATION OPPORTUNITIES FOR HILL TRIBES IN NORTHERN THAILAND Implications for sustainable rural development By Rika Fujioka Food and Agriculture Organization of the United Nations Regional Office for Asia and the Pacific Bangkok, Thailand 2002 TABLE OF CONTENTS Foreword .……………………………………………………………………………………….