1 Trends in Peptide Therapeutics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Review of Current Real-World Experience with Teriparatide As Treatment of Osteoporosis in Different Patient Groups
Journal of Clinical Medicine Review Review of Current Real-World Experience with Teriparatide as Treatment of Osteoporosis in Different Patient Groups Barbara Hauser 1,2,* , Nerea Alonso 2 and Philip L Riches 1,2 1 Rheumatic Disease Unit, Western General Hospital, NHS Lothian, Edinburgh EH4 2XU, UK; [email protected] 2 Rheumatology and Bone Disease Unit, Centre for Genomic and Experimental Medicine, MRC Institute of Genetics and Molecular Medicine, University of Edinburgh, Edinburgh EH4 2XU, UK; [email protected] * Correspondence: [email protected] Abstract: Teriparatide has proven effective in reducing both vertebral and non-vertebral fractures in clinical trials of post-menopausal and glucocorticoid-induced osteoporosis. Widespread adoption of Teriparatide over the last two decades means that there is now substantial experience of its use in routine clinical practice, which is summarized in this paper. Extensive real-world experience of Teriparatide in post-menopausal osteoporosis confirms the fracture and bone density benefits seen in clinical trials, with similar outcomes identified also in male and glucocorticoid-induced osteoporosis. Conversely, very limited experience has been reported in pre-menopausal osteoporosis or in the use of Teriparatide in combination with other therapies. Surveillance studies have identified no safety signals relating to the possible association of Teriparatide with osteosarcoma. We also review the evidence for predicting response to Teriparatide in order to inform the debate on where best to use Teriparatide in an increasingly crowded therapeutic landscape. Citation: Hauser, B.; Alonso, N.; Riches, P.L. Review of Current Keywords: Teriparatide; anabolic treatment; osteoporosis; fracture Real-World Experience with Teriparatide as Treatment of Osteoporosis in Different Patient Groups. -

The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands
The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands Clare Louise Wishart Submitted in accordance with the requirements for the degree of Doctor of Philosophy of Science University of Leeds School of Biomedical Sciences Faculty of Biological Sciences September 2013 I Intellectual Property and Publication Statements The candidate confirms that the work submitted is her own and that appropriate credit has been given where reference has been made to the work of others. This copy has been supplied on the understanding that it is copyright material and that no quotation from the thesis may be published without proper acknowledgement. The right of Clare Louise Wishart to be identified as Author of this work has been asserted by her in accordance with the Copyright, Designs and Patents Act 1988. © 2013 The University of Leeds and Clare Louise Wishart. II Acknowledgments Firstly I would like to offer my sincerest thanks and gratitude to my supervisor, Dr. Dan Donnelly, who has been nothing but encouraging and engaging from day one. I have thoroughly enjoyed every moment of working alongside him and learning from his guidance and wisdom. My thanks go to my academic assessor Professor Paul Milner whom I have known for several years, and during my time at the University of Leeds he has offered me invaluable advice and inspiration. Additionally I would like to thank my academic project advisor Dr. Michael Harrison for his friendship, help and advice. I would like to thank Dr. Rosalind Mann and Dr. Elsayed Nasr for welcoming me into the lab as a new PhD student and sharing their experimental techniques with me, these techniques have helped me no end in my time as a research student. -

Performance of the Insulin-Only Ilet Bionic Pancreas and The
e118 Diabetes Care Volume 44, June 2021 Performance of the Insulin-Only Luz E. Castellanos,1 Courtney A. Balliro,1 Jordan S. Sherwood,1 Rabab Jafri,1 iLet Bionic Pancreas and the Mallory A. Hillard,1 Evelyn Greaux,1 Rajendranath Selagamsetty,2 Hui Zheng,3 Bihormonal iLet Using Firas H. El-Khatib,2 Edward R. Damiano,2,4 and Dasiglucagon in Adults With Type Steven J. Russell1 1 Diabetes in a Home-Use Setting Diabetes Care 2021;44:e118–e120 | https://doi.org/10.2337/dc20-1086 Reductions in blood glucose levels in with insulin lispro (Eli Lilly) or aspart (Table 1). The mean CGM glucose and people with diabetes are often achieved (Novo Nordisk), the bihormonal iLet for time in range (70–180 mg/dL) were 149 at the expense of increased hypoglyce- 7dayswithdasiglucagon(4mg/mL) ±13mg/dLand72±8%,respectively,in mia. A novel approach is to automati- and insulin lispro or aspart, or both, us- the insulin-only period, and 139 ± 11 cally deliver microdose glucagon when ing the same glucose target (110 mg/ mg/dL and 79 ± 9%, respectively, in the automation of insulin delivery alone is dL), in random order. There were no re- bihormonal period. The mean daily car- not sufficient to prevent hypoglycemia. strictions on diet or exercise. The prima- bohydrates consumed to prevent or The approach requires a bihormonal de- ry outcomes were prespecified iLet treat hypoglycemia were 16 ± 13 g and vice and a stable form of glucagon or operational thresholds. The key second- 18 ± 21 g in the insulin-only and bihor- glucagon analog. -
Peptide Therapeutics Designing a Science-Led Strategic Quality Control Program
BioProcess International Peptide SPECIAL REPORT Therapeutics Designing a Science-Led Strategic Quality Control Program INTERTEK PHARMACEUTICAL SERVICES Your partner for regulatory-driven, phase appropriate analytical programs tailored to your molecule. Our experts help you to navigate the challenges of development, regulatory submission, and manufacturing. Peptide Therapeutics Designing a Science-Led Strategic Quality Control Program Shashank Sharma and Hannah Lee ince the emergence of peptide therapeutics in the 1920s with the advent of insulin therapy, the market for this product class has continued to expand with global revenues anticipatedS to surpass US$50 billion by 2024 (1). The growth of peptide therapeutics is attributed not only to improvements in manufacturing, but also to a rise in demand because of an increasingly aging population that is driving an increase in the occurrence of long-term diseases. The need for efficient and low-cost drugs and rising investments in research and development of novel drugs continues to boost market growth and fuel the emergence of generic versions that offer patients access to vital medicines at low costs. North America has been the dominant market for peptide therapeutics, with the Asia–Pacific region Insulin molecular model; the first therapeutic expected to grow at a faster rate. The global peptides use of this peptide hormone was in the market has attracted the attention of key players 1920s to treat diabetic patients. within the pharmaceutical industry, including Teva Pharmaceuticals, Eli Lilly, Novo Nordisk, Pfizer, amino acids to be peptides. Within that set, those Takeda, and Amgen. Those companies have made containing 10 or more are classed as polypeptides. -
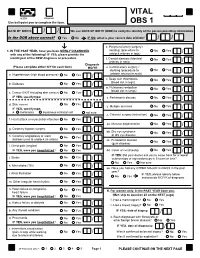
VITAL Jan 2019 Follow-Up
VITAL 6308 Request Use ball-point pen to complete the form. OBS 1 DATE OF BIRTH: / / We use DATE OF BIRTH (DOB) to verify the identity of the person providing information. Is the DOB above correct? Yes No IF NO, what is your correct date of birth? / / s. Peripheral artery surgery / 1. IN THE PAST YEAR, have you been NEWLY DIAGNOSED stenting (procedure to No Yes / with any of the following? IF YES, please provide the unblock arteries in legs) month/year of the NEW diagnosis or procedure. t. Carotid stenosis (blocked No Yes Answer NO/YES on each line. arteries in neck) / Diagnosis (Please complete either N/Y for each item) MO/YR u. Carotid artery surgery / stenting (procedure to No Yes / a. Hypertension (high blood pressure) No Yes / unblock arteries in neck) v. Deep vein thrombosis No Yes (blood clot in legs) / b. Diabetes No Yes / w. Pulmonary embolism No Yes (blood clot in lungs) / c. Cancer (NOT including skin cancer) No Yes / IF YES, specify type: _______________________ x. Parkinson's disease No Yes / d. Skin cancer No Yes / y. Multiple sclerosis No Yes IF YES, specify type: / e. melanoma squamous or basal cell not sure z. Cataract surgery (extraction) No Yes / f. Heart attack or myocardial infarction No Yes / aa. Macular degeneration No Yes / g. Coronary bypass surgery No Yes / bb. Dry eye syndrome No Yes or dry eye disease / h. Coronary angioplasty or stent No Yes (balloon used to unblock an artery) / cc. Periodontal disease No Yes (gum disease) / i. Chest pain (angina) No Yes / IF YES, were you hospitalized? No Yes dd. -

Peptides As Drug Candidates: Limitations and Recent Development Perspectives
ISSN: 2574-1241 Volume 5- Issue 4: 2018 DOI: 10.26717/BJSTR.2018.08.001694 Yusuf A Haggaga. Biomed J Sci & Tech Res Mini Rewiew Open Access Peptides as Drug Candidates: Limitations and Recent Development Perspectives Yusuf A. Haggag*1, Ahmed A. Donia1,2, Mohamed A. Osman1, Sanaa A. El-Gizawy1 1Department of Pharmaceutical Technology, Faculty of Pharmacy, Tanta University, Tanta, Egypt 2Department of Pharmaceutical Technology, Faculty of Pharmacy, Menofia University, Menofia, Egypt Received: Published: *Corresponding August author: 28, 2018; September 05, 2018 Yusuf A Haggag, Department of Pharmaceutical Technology, Faculty of Pharmacy, Tanta University, Egypt Abbreviations: GLP-1: Glucagon-Like Peptide-1; PEG: Polyethylene Glycol; Gamma IgG: Immunoglobulin; FcRn: Fc Receptor Introduction [4]. Discovery of several tumor-related peptides and proteins also Peptides can be defined as polypeptide chains of 50 or less protein/peptide receptors is supposed to create a new revolution amino acids or 5000 Da in molecular weight characterized by a wave of more promising, effective and selective anticancer drugs in high degree of secondary structure and lack of tertiary structure. the future. Therapeutic anticancer peptides will capture the largest Therapeutic peptides have traditionally been derived from nature share of the cancer therapeutic market [2]. This mode of cancer as naturally occurring peptide hormones (known as bioactive treatment including peptides, proteins and monoclonal antibodies peptides), genetic/recombinant libraries and chemical libraries is termed “biologics” treatment option [5]. [1]. The recent technologies used for peptides production include chemical synthesis, enzymatic synthesis, recombinant DNA About 75% from the whole peptide drugs in the market that biotechnology, cell-free expression and transgenic animal or plant gained total global sales over $1 billion are used directly in cancer There are several hundred peptide candidates under clinical species. -

Novel Therapies in Osteoporosis: PTH-Related Peptide Analogs and Inhibitors of Sclerostin
62 2 Journal of Molecular T D Rachner et al. Novel anabolic osteoporosis 62:2 R145–R154 Endocrinology treatments REVIEW Novel therapies in osteoporosis: PTH-related peptide analogs and inhibitors of sclerostin Tilman D Rachner1,2,3, Lorenz C Hofbauer1,2,3,4, Andy Göbel1,3 and Elena Tsourdi1,2,3 1Department of Medicine III, Technische Universität Dresden Medical Center, Dresden, Germany 2Center for Healthy Aging, Technische Universität Dresden Medical Center, Dresden, Germany 3German Cancer Consortium (DKTK), partner site Dresden and German Cancer Research Center (DKFZ), Dresden, Germany 4Center for Regenerative Therapies Dresden, Technische Universität Dresden, Dresden, Germany Correspondence should be addressed to T D Rachner: [email protected] Abstract Bone-forming approaches to treat patients with severe osteoporosis are effective, but Key Words treatment options are limited, and there is an unmet clinical need for additional drugs. f PTH This review discusses two novel and advanced anabolic therapeutic concepts that f PTH-related protein have successfully completed phase 3 trials. Romosozumab is a monoclonal antibody f abaloparatide that targets the Wnt inhibitor sclerostin. Two phase 3 trials (FRAME and ARCH) of f sclerostin romosozumab for the treatment of postmenopausal osteoporosis have been completed. f sclerostin antibody Both trials successfully reached their primary endpoint by reducing vertebral fractures by f romosozumab 75% compared to placebo (FRAME trial) and 48% compared to alendronate (ARCH trial), respectively. Abaloparatide is a PTH-related protein (PTHrP) analog that has displayed bone anabolic activity. In the phase 3 ACTIVE trial, abaloparatide was compared to placebo and teriparatide for 18 months in postmenopausal women who had already experienced an osteoporotic fracture. -

Design, Development, and Characterization of Novel Antimicrobial Peptides for Pharmaceutical Applications Yazan H
University of Arkansas, Fayetteville ScholarWorks@UARK Theses and Dissertations 8-2013 Design, Development, and Characterization of Novel Antimicrobial Peptides for Pharmaceutical Applications Yazan H. Akkam University of Arkansas, Fayetteville Follow this and additional works at: http://scholarworks.uark.edu/etd Part of the Biochemistry Commons, Medicinal and Pharmaceutical Chemistry Commons, and the Molecular Biology Commons Recommended Citation Akkam, Yazan H., "Design, Development, and Characterization of Novel Antimicrobial Peptides for Pharmaceutical Applications" (2013). Theses and Dissertations. 908. http://scholarworks.uark.edu/etd/908 This Dissertation is brought to you for free and open access by ScholarWorks@UARK. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of ScholarWorks@UARK. For more information, please contact [email protected], [email protected]. Design, Development, and Characterization of Novel Antimicrobial Peptides for Pharmaceutical Applications Design, Development, and Characterization of Novel Antimicrobial Peptides for Pharmaceutical Applications A Dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Cell and Molecular Biology by Yazan H. Akkam Jordan University of Science and Technology Bachelor of Science in Pharmacy, 2001 Al-Balqa Applied University Master of Science in Biochemistry and Chemistry of Pharmaceuticals, 2005 August 2013 University of Arkansas This dissertation is approved for recommendation to the Graduate Council. Dr. David S. McNabb Dissertation Director Professor Roger E. Koeppe II Professor Gisela F. Erf Committee Member Committee Member Professor Ralph L. Henry Dr. Suresh K. Thallapuranam Committee Member Committee Member ABSTRACT Candida species are the fourth leading cause of nosocomial infection. The increased incidence of drug-resistant Candida species has emphasized the need for new antifungal drugs. -

NMR Spectroscopy for Protein Higher Order Structure Similarity Assessment in Formulated Drug Products
molecules Article NMR Spectroscopy for Protein Higher Order Structure Similarity Assessment in Formulated Drug Products Deyun Wang 1, You Zhuo 2, Mike Karfunkle 3, Sharadrao M. Patil 2, Cameron J. Smith 4, David A. Keire 5 and Kang Chen 2,* 1 Northeast Medical Products Laboratory, Office of Regulatory Science, Office of Regulatory Affairs, U.S. Food and Drug Administration, Jamaica, NY 11433, USA; [email protected] 2 Division of Complex Drug Analysis, Office of Testing and Research, Office of Pharmaceutical Quality, Center for Drug Evaluation and Research, U.S. Food and Drug Administration, Silver Spring, MD 20993, USA; [email protected] (Y.Z.); [email protected] (S.M.P.) 3 Division of Pharmaceutical Analysis, Office of Testing and Research, Office of Pharmaceutical Quality, Center for Drug Evaluation and Research, U.S. Food and Drug Administration, St. Louis, MO 63110, USA; [email protected] 4 Division of Liquid Based Products I, Office of Lifecycle Drug Products, Office of Pharmaceutical Quality, Center for Drug Evaluation and Research, U.S. Food and Drug Administration, Silver Spring, MD 20993, USA; [email protected] 5 Office of Testing and Research, Office of Pharmaceutical Quality, Center for Drug Evaluation and Research, U.S. Food and Drug Administration, St. Louis, MO 63110, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-240-402-5550 Abstract: Peptide and protein drug molecules fold into higher order structures (HOS) in formulation and these folded structures are often critical for drug efficacy and safety. Generic or biosimilar drug Citation: Wang, D.; Zhuo, Y.; products (DPs) need to show similar HOS to the reference product. -

AACE Annual Meeting 2021 Abstracts Editorial Board
June 2021 Volume 27, Number 6S AACE Annual Meeting 2021 Abstracts Editorial board Editor-in-Chief Pauline M. Camacho, MD, FACE Suleiman Mustafa-Kutana, BSC, MB, CHB, MSC Maywood, Illinois, United States Boston, Massachusetts, United States Vin Tangpricha, MD, PhD, FACE Atlanta, Georgia, United States Andrea Coviello, MD, MSE, MMCi Karel Pacak, MD, PhD, DSc Durham, North Carolina, United States Bethesda, Maryland, United States Associate Editors Natalie E. Cusano, MD, MS Amanda Powell, MD Maria Papaleontiou, MD New York, New York, United States Boston, Massachusetts, United States Ann Arbor, Michigan, United States Tobias Else, MD Gregory Randolph, MD Melissa Putman, MD Ann Arbor, Michigan, United States Boston, Massachusetts, United States Boston, Massachusetts, United States Vahab Fatourechi, MD Daniel J. Rubin, MD, MSc Harold Rosen, MD Rochester, Minnesota, United States Philadelphia, Pennsylvania, United States Boston, Massachusetts, United States Ruth Freeman, MD Joshua D. Safer, MD Nicholas Tritos, MD, DS, FACP, FACE New York, New York, United States New York, New York, United States Boston, Massachusetts, United States Rajesh K. Garg, MD Pankaj Shah, MD Boston, Massachusetts, United States Staff Rochester, Minnesota, United States Eliza B. Geer, MD Joseph L. Shaker, MD Paul A. Markowski New York, New York, United States Milwaukee, Wisconsin, United States CEO Roma Gianchandani, MD Lance Sloan, MD, MS Elizabeth Lepkowski Ann Arbor, Michigan, United States Lufkin, Texas, United States Chief Learning Officer Martin M. Grajower, MD, FACP, FACE Takara L. Stanley, MD Lori Clawges The Bronx, New York, United States Boston, Massachusetts, United States Senior Managing Editor Allen S. Ho, MD Devin Steenkamp, MD Corrie Williams Los Angeles, California, United States Boston, Massachusetts, United States Peer Review Manager Michael F. -

MSM Chapter 1200 3/1/21
MEDICAID SERVICES MANUAL TRANSMITTAL LETTER February 23, 2021 TO: CUSTODIANS OF MEDICAID SERVICES MANUAL FROM: JESSICA KEMMERER, HIPAA PRIVACY AND CIVIL RIGHTS OFFICER /Jessica Kemmerer/ BACKGROUND AND EXPLANATION The DHCFP is proposing revisions to Medicaid Services Manual (MSM), Chapter 1200 – Prescribed Drugs, Appendix A, to reflect recommendations approved on October 22, 2020, by the Drug Use Review (DUR) Board. The proposed changes include the addition of new prior authorization criteria for Doxepine Topical, the addition of new prior authorization criteria for Zeposia® (ozanimod), addition of new prior authorization for Evenity® (romosozumab-aqqg), Prolia® (denosumab), Forteo® (teriparatide) and Tymlos® (abaloparatide) within a new combined osteoporosis agents section, and addition of new prior authorization criteria for Orilissa® (elagolix) and Oriahnn® (elagolix, estradiol, and norethindrone) within a new Gonadorpin Hormone Receptor (GnRH) Antagonist and Combinations section. Additionally, the DHCFP is proposing revisions to the existing prior authorization criteria for psychotropic medications for children and adolescents, and revision to the existing clinical criteria for Epidiolex® (cannabidiol). Throughout the chapter, grammar, punctuation and capitalization changes were made, duplications removed, acronyms used and standardized, and language reworded for clarity. Renumbering and re- arranging of sections was necessary. These changes are effective March 1, 2021. MATERIAL TRANSMITTED MATERIAL SUPERSEDED MTL N/A MTL N/A MSM Ch 1200 – Prescribed Drugs MSM Ch 1200 – Prescribed Drugs Background and Explanation of Policy Changes, Manual Section Section Title Clarifications and Updates Appendix A Psychotropic Added new policy language criteria on which specific Section N Medications for drug classes may bypass polypharmacy clinical criteria. Children and Adolescents Appendix A Reserved for Future Created a new section titled “Doxepin Topical.” Added Section W Use new prior authorization criteria for doxepin topical. -

Therapeutic Oligos & Peptides
Focus on Therapeutic Oligos & Peptides Enhancing the pharmaceutical properties of peptides To begin the discussion about enhancing or improving pharmaceutical properties, one must fi rst understand “the good, the bad, and the ugly” of peptides (1). The good. Peptides are generally highly potent, selective, and have a low potential for toxicity and low risk of drug-drug interaction. The bad. Peptides are generally not terribly stable in biological matrices, susceptible to protease degradation. The ugly. The polar nature of the peptide bond and the size of peptide molecules makes permeability across cell membranes challenging. In small molecule drug PEGylation development, we commonly think PEGylation refers to the attachment about Lipinski’s rule of fi ve (2), of poly(ethylene glycol) or PEG to which is based on the observation Keyw ds peptides or proteins and is able that most orally administered drugs to improve the pharmacokinetic have common physicochemical PEGylation, lipidation, properties of these molecules. characteristics, namely, glycosylation, PEG increases the hydration shell 1. a molecular mass less than 500 cyclization, of a peptide, making the peptide daltons non-natural amino less susceptible to renal clearance 2. a logP (octanol-water partition acid substitution and protease degradation. coeffi cient) less than 5 PEGylation can also decrease the 3. no more than 5 hydrogen bond immunogenicity potential. There are donors many diff erent PEG molecules that can be covalently 4. no more than 10 (2 x 5) hydrogen bond acceptors. attached to peptides including linear or branched, low Peptides violate each and every one of these rules, molecular weight or high molecular weight.