Synagis) Prophylaxis in Hospitalized Patients Evidence Summary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Journal Pre-Proof
Journal Pre-proof Neutralizing monoclonal antibodies for COVID-19 treatment and prevention Juan P. Jaworski PII: S2319-4170(20)30209-2 DOI: https://doi.org/10.1016/j.bj.2020.11.011 Reference: BJ 374 To appear in: Biomedical Journal Received Date: 2 September 2020 Revised Date: 6 November 2020 Accepted Date: 22 November 2020 Please cite this article as: Jaworski JP, Neutralizing monoclonal antibodies for COVID-19 treatment and prevention, Biomedical Journal, https://doi.org/10.1016/j.bj.2020.11.011. This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. © 2020 Chang Gung University. Publishing services by Elsevier B.V. TITLE: Neutralizing monoclonal antibodies for COVID-19 treatment and prevention Juan P. JAWORSKI Consejo Nacional de Investigaciones Científicas y Técnicas, Buenos Aires, Argentina Instituto Nacional de Tecnología Agropecuaria, Buenos Aires, Argentina KEYWORDS: SARS-CoV-2, Coronavirus, Monoclonal Antibody, mAb, Prophylaxis, Treatment CORRESPONDING AUTHOR: Dr. Juan Pablo Jaworski, DVM, MSc, PhD. Consejo Nacional de Investigaciones Científicas y Técnicas Instituto de Virología, Instituto Nacional de Tecnología Agropecuaria Las Cabañas y de los Reseros (S/N), Hurlingham (1686), Buenos Aires, Argentina Tel / Fax: 054-11-4621-1447 (int:3400) [email protected] ABSTRACT The SARS-CoV-2 pandemic has caused unprecedented global health and economic crises. -

Phage Display-Based Strategies for Cloning and Optimization of Monoclonal Antibodies Directed Against Human Pathogens
Int. J. Mol. Sci. 2012, 13, 8273-8292; doi:10.3390/ijms13078273 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Review Phage Display-based Strategies for Cloning and Optimization of Monoclonal Antibodies Directed against Human Pathogens Nicola Clementi *,†, Nicasio Mancini †, Laura Solforosi, Matteo Castelli, Massimo Clementi and Roberto Burioni Microbiology and Virology Unit, “Vita-Salute” San Raffaele University, Milan 20132, Italy; E-Mails: [email protected] (N.M.); [email protected] (L.S.); [email protected] (M.C.); [email protected] (M.C.); [email protected] (R.B.) † These authors contributed equally to this work. * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +39-2-2643-5082; Fax: +39-2-2643-4288. Received: 16 March 2012; in revised form: 25 June 2012 / Accepted: 27 June 2012 / Published: 4 July 2012 Abstract: In the last two decades, several phage display-selected monoclonal antibodies (mAbs) have been described in the literature and a few of them have managed to reach the clinics. Among these, the anti-respiratory syncytial virus (RSV) Palivizumab, a phage-display optimized mAb, is the only marketed mAb directed against microbial pathogens. Palivizumab is a clear example of the importance of choosing the most appropriate strategy when selecting or optimizing an anti-infectious mAb. From this perspective, the extreme versatility of phage-display technology makes it a useful tool when setting up different strategies for the selection of mAbs directed against human pathogens, especially when their possible clinical use is considered. -

Synagis, INN-Palivizumab;
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Synagis 50 mg/0.5 ml solution for injection Synagis 100 mg/1 ml solution for injection 2. QUALITATIVE AND QUANTITATIVE COMPOSITION 1 ml of Synagis solution contains 100 mg of palivizumab*. Each 0.5 ml vial contains 50 mg of palivizumab. Each 1 ml vial contains 100 mg of palivizumab. *Palivizumab is a recombinant humanised monoclonal antibody produced by DNA technology in mouse myeloma host cells. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection. The solution is clear or slightly opalescent. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Synagis is indicated for the prevention of serious lower respiratory tract disease requiring hospitalisation caused by respiratory syncytial virus (RSV) in children at high risk for RSV disease: Children born at 35 weeks of gestation or less and less than 6 months of age at the onset of the RSV season. Children less than 2 years of age and requiring treatment for bronchopulmonary dysplasia within the last 6 months. Children less than 2 years of age and with haemodynamically significant congenital heart disease. 4.2 Posology and method of administration Posology The recommended dose of palivizumab is 15 mg/kg of body weight, given once a month during anticipated periods of RSV risk in the community. The volume (expressed in ml) of // Palivizumab // to be administered at one-monthly intervals = [patient weight in kg] multiplied by 0.15. Where possible, the first dose should be administered prior to commencement of the RSV season. -

Medicines/Pharmaceuticals of Animal Origin V3.0 November 2020
Medicines/pharmaceuticals of animal origin V3.0 November 2020 Medicines/pharmaceuticals of animal origin - This guideline provides information for all clinical staff within Hospital and Health Services (HHS) on best practice for avoidance of issues related to animal products. Medicines/pharmaceuticals of animal origin - V3.0 November 2020 Published by the State of Queensland (Queensland Health), November 2020 This document is licensed under a Creative Commons Attribution 3.0 Australia licence. To view a copy of this licence, visit creativecommons.org/licenses/by/3.0/au © State of Queensland (Queensland Health) 2020 You are free to copy, communicate and adapt the work, as long as you attribute the State of Queensland (Queensland Health). For more information contact: Medication Services Queensland, Queensland Health, GPO Box 48, Brisbane QLD 4001, email [email protected] An electronic version of this document is available at https://www.health.qld.gov.au/__data/assets/pdf_file/0024/147507/qh-gdl-954.pdf Disclaimer: The content presented in this publication is distributed by the Queensland Government as an information source only. The State of Queensland makes no statements, representations or warranties about the accuracy, completeness or reliability of any information contained in this publication. The State of Queensland disclaims all responsibility and all liability (including without limitation for liability in negligence) for all expenses, losses, damages and costs you might incur as a result of the information being inaccurate -
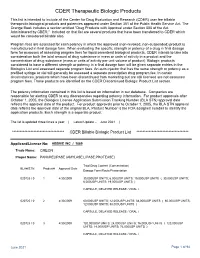
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database. -

Neutralizing Antibodies: the Elite Squad to Combat SARS-Cov-2
November 20, 2020 Health & Physiology Neutralizing antibodies: the Elite Squad to combat SARS-CoV-2 infection 1 1 1 by Guanqiao Li | Research Associate; Yang Liu | Research Associate; Linqi Zhang | Professor 1: Center for Global Health and Infectious Diseases, School of Medicine and Vanke School of Public Health, Tsinghua University, Beijing, China This Break was edited by Max Caine, Editor-in-chief - TheScienceBreaker The coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS -CoV-2) urgently calls for prevention and treatment interventions. Neutralizing antibodies isolated from recovered patients are capable of blocking the virus from entry into human cells, potentially acting as the “Elite Squad” to defeat SARS-CoV-2. Image credits: Alissa Eckert, MS; Dan Higgins, MAMS The rapid global transmission of SARS-CoV-2 poses a entering the cells. These antibodies are therefore severe health emergency affecting over 20 million called "neutralizing antibodies". Neutralizing people worldwide as of 12 August. The research antibodies hold a great promise for clinical communities have taken immediate and enormous intervention. A substantial number of investigational actions in search of therapeutic and prophylactic neutralizing antibodies are under development for interventions. The major strategies undertaken diverse infectious diseases. Notably, three have include repurposing “old” drugs, identifying "new" received approval to prevent respiratory syncytial drugs, and taking advantage of neutralizing virus (palivizumab) and prevent and treat anthrax antibodies produced in the plasma of survivors. (raxibacumab and obiltoxaximab). Ultimately, developing vaccines that provide sufficient and long protection against infection and Since the outbreak of COVID-19, we have been diseases. -
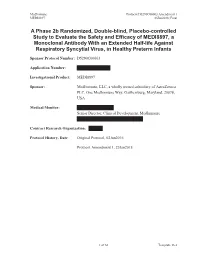
A Phase 2B Randomized, Double-Blind, Placebo-Controlled Study to Evaluate the Safety and Efficacy of MEDI8897, a Monoclonal Anti
MedImmune Protocol D5290C00003 Amendment 1 MEDI8897 25Jan2018; Final A Phase 2b Randomized, Double-blind, Placebo-controlled Study to Evaluate the Safety and Efficacy of MEDI8897, a Monoclonal Antibody With an Extended Half-life Against Respiratory Syncytial Virus, in Healthy Preterm Infants Sponsor Protocol Number: D5290C00003 Application Number: Investigational Product: MEDI8897 Sponsor: MedImmune, LLC, a wholly owned subsidiary of AstraZeneca PLC, One MedImmune Way, Gaithersburg, Maryland, 20878, USA Medical Monitor: Senior Director, Clinical Development, MedImmune Contract Research Organization: Protocol History, Date: Original Protocol, 02Jun2016 Protocol Amendment 1, 25Jan2018 1 of 66 Template 16.2 MedImmune Protocol D5290C00003 Amendment 1 MEDI8897 25Jan2018; Final PROTOCOL SYNOPSIS TITLE A Phase 2b Randomized, Double-blind, Placebo-controlled Study to Evaluate the Safety and Efficacy of MEDI8897, a Monoclonal Antibody With an Extended Half-life Against Respiratory Syncytial Virus, in Healthy Preterm Infants HYPOTHESES Primary Hypothesis: Compared to placebo, a single mg intramuscular (IM) dose of MEDI8897 will be efficacious in reducing medically attended lower respiratory tract infection (LRTI) caused by real-time reverse transcriptase polymerase chain reaction (RT-PCR)-confirmed respiratory syncytial virus (RSV) in healthy preterm infants born between 29 weeks 0 days and 34 weeks 6 days gestational age (GA) and entering their first RSV season, and the safety profile will be acceptable. Secondary Hypotheses: 1. There will be a -

Neutralizing Monoclonal Antibodies for Treatment of COVID-19
REVIEWS Neutralizing monoclonal antibodies for treatment of COVID-19 Peter C. Taylor 1 ✉ , Andrew C. Adams2, Matthew M. Hufford2, Inmaculada de la Torre2, Kevin Winthrop3 and Robert L. Gottlieb 4,5 Abstract | Several neutralizing monoclonal antibodies (mAbs) to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have been developed and are now under evaluation in clinical trials. With the US Food and Drug Administration recently granting emergency use authorizations for neutralizing mAbs in non-hospitalized patients with mild-to- moderate COVID-19, there is an urgent need to discuss the broader potential of these novel therapies and to develop strategies to deploy them effectively in clinical practice, given limited initial availability. Here, we review the precedent for passive immunization and lessons learned from using antibody therapies for viral infections such as respiratory syncytial virus, Ebola virus and SARS-CoV infections. We then focus on the deployment of convalescent plasma and neutralizing mAbs for treatment of SARS- CoV-2. We review specific clinical questions, including the rationale for stratification of patients, potential biomarkers, known risk factors and temporal considerations for optimal clinical use. To answer these questions, there is a need to understand factors such as the kinetics of viral load and its correlation with clinical outcomes, endogenous antibody responses, pharmacokinetic properties of neutralizing mAbs and the potential benefit of combining antibodies to defend against emerging viral variants. 3–5 Monoclonal antibodies In the midst of the current COVID-19 pandemic, a combination therapy . Therefore, several questions (mAbs). Clonal antibodies variety of prophylactic and therapeutic treatments are need to be addressed about the potential clinical use of recognizing a single epitope on being developed or repurposed to combat COVID-19. -

Nebraska Supplemental PDL June 2018
Applies to: Nebraska Supplemental PDL Albenza (albendazole) Albenza (albendazole) Covered uses All medically accepted indications Exclusion Criteria See age restrictions Required Medical Enterobiasis, ascariasis: Medical documentation indicating use Information for treatment for enterobiasis and previous trial and failure to ivermectin and Pin-X Intestinal strongyloidiasis, cutaneous larva migrans, or infection by loa loa: Medical documentation indicating use for treatment for intestinal strongyloidiasis, cutaneous larva migrans, or infection by loa loa and previous trial and failure to ivermectin. Approve for use as empiric treatment for presumptive strongyloides infection in Sub-Saharan Africa refugees from LoaLoa endemic countries, regardless of previous ivermectin use.2 Echinococcosis (Hydatid disease), neurocysticercosis: Medical documentation indicating the use for treatment of echinococcosis or neurocysticercosis. Age restrictions 1 year of age or older Prescriber None Restrictions Coverage Duration 6 months (Hytadid) 1 month for other indications Other Criteria None Reference 1. Albenza [package insert]. Amedra Pharmaceuticals. Horsham, PA. February, 2013 2. Centers for Disease Control and Prevention. Guidelines for Overseas Presumptive Treatment of Strongyloidiasis, Schistosomiasis, and Soil-Transmitted Helminth Infections. http://www.cdc.gov/immigrantrefugeehealth/guidelines/overseas/intestinalparasites- overseas.html. Accessed August 20, 2014. Updated 01/2017 Page 1 of 1 Applies to: Aristada (aripiprazole lauroxil) Nebraska -
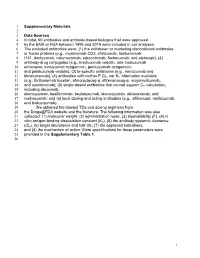
1 Supplementary Materials 1 2 Data Sources 3 in Total, 60 Antibodies
1 Supplementary Materials 2 3 Data Sources 4 In total, 60 antibodies and antibody-based biologics that were approved 5 by the EMA or FDA between 1995 and 2019 were included in our analyses. 6 The excluded antibodies were: (1) the withdrawn or marketing discontinued antibodies 7 or fusion proteins (e.g., muromonab-CD3, efalizumab, tositumomab- 8 I131, daclizumab, catumaxomab, edrecolomab, Nebacumab, and alefacept); (2) 9 antibody-drug conjugates (e.g., brentuximab vedotin, ado-trastuzumab 10 emtansine, inotuzumab ozogamicin, gemtuzumab ozogamicin, 11 and polatuzumab vedotin); (3) bi-specific antibodies (e.g., emicizumab and 12 blinatumomab); (4) antibodies with neither F CL, nor KD information available 13 (e.g., Ibritumomab tiuxetan, efmoroctocog-α, eftrenonacog-α, mogamulizumab, 14 and ustekinumab); (5) single-dosed antibodies that cannot support Css calculation, 15 including abciximab, 16 alemtuzumab, basiliximmab, bezlotoxumab, idarucizumab, obiloxaximab, and 17 raxibacumab; and (6) local dosing and acting antibodies (e.g., aflibercept, ranibizumab, 18 and brolucizumab). 19 We obtained the labeled TDs and dosing regimens from 20 the Drugs@FDA website and the literature. The following information was also 21 collected: (1) molecular weight, (2) administration route, (3) bioavailability (F), (4) in 22 vitro antigen-binding dissociation constant (KD), (5) the antibody systemic clearance 23 (CL), (6) target abundance and half-life, (7) the approved indications, 24 and (8) the mechanism of action. More specifications for these parameters were 25 provided in the Supplementary Table 1. 26 1 27 Supplementary Figure 1 28 29 30 Supplementary Figure 1. Target turnovers are not relevant to TEARs in four 31 disease-target scenarios. Dots represent the mean values. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Monoclonal Antibodies for Infectious Diseases
Monoclonal antibodies for infectious diseases Martin Friede 1890: Emil von Behring and Shibasaburo Kitasato From anti-toxin to the serotherapy of diptheria, tetanus Nobel prize for von Behring in 1901 2 | The birth of anti-infectives 3 | A century of trials and success Diptheria Influenza (pandemic) Tetanus Haemophilus influenza Rabies Pseudomonas Hepatitis A & B Malaria Varicella Polio RSV Hemorhagic fever Pneumococcus Ebola (?) Meningococcus …. And others 4 | And still a strong demand Procurement by PAHO revolving fund (doses) 2009 2010 2011 2012 Tetanus 14000 5000 17000 32000 Rabies 15000 16000 31000 40000 Hepatitis B 47000 48000 5000 72000 Varicella 12000 15000 23000 21000 5 | The Birth of Monoclonal antibodies 1975 Cesar Milstein and Georges Köhler develop technique for making monoclonal antibodies Nobel prize: 1982 "Developed as a "research tool…" Currently $140,000,000,000 / year market 6 | The pros and cons of monoclonal antibodies for infectious diseases Safety theoretically easy to predict (but not always…) Functions rapidly (unlike vaccines) Quicker to develop than vaccines Supply: limited ! Cost: !!!!! Especially when grams of product needed ! Time to development !! 7 | mAbs in infectious disease Palivizumab: anti-RSV mAb (Medimmune 1998) – First monoclonal approved for prophylaxis of infectious disease (RSV). – For premature infants (<29 weeks), CHF, bronchopulmonary dysplasia. – $7000-10,000 per treatment course (4-5 months). Raxibacumab: anti-anthrax mAb (GSK 2012) – Approved using animal rule – For treatment of inhalation anthrax. 8 | Improved production systems Murine myeloma NS0 cells Variable glycosylation CHO cells patterns -> immunogenicity, function PerC6 Tobacco plants Yield 0.1g/l 10g/l Technical skills barrier, Technology access barrier, Cost of goods: $10,000/g $100g CAPEX barrier.