Journal Pre-Proof
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

T. Franklin Williams Scholars Program
Developing a New Generation of Medical Subspecialists with Expertise in Aging and Care of the Elderly T. Franklin Williams Scholars Program Report to T. Franklin Williams Scholars Program Evaluation Team ASP Geriatrics Steering Committee Integrating Geriatrics Project Evaluation Team May 2011 Submitted by: Erika D. Tarver Project Administrator Association of Specialty Professors 330 John Carlyle Road Suite 610 Alexandria, VA 22314 T: (703) 341-4540 F: (703) 519-1890 [email protected] Kevin P. High, MD Principal Investigator William R. Hazzard, MD Co-Principal Investigator Table of Contents Narrative Progress Report Application and Award Progress Summary of Success of T. Williams Scholars Program Appendices A. 2008 Scholars 24-Month Progress Reports Neena S. Abraham, MD (Note: This is Dr. Abraham’s final report) Steven G. Coca, DO Jeffrey G. Horowitz, MD Danelle F. James, MD Heidi Klepin, MD George C. Wang, MD 2009 Williams Scholars Progress Reports and Summary of 18-Month Questionnaire B. Peter Abadir, MD 12-month Progress Report C. Kathleen M. Akgun, MD 12-Month Progress Report Publication D. Alison Huang, MD 12-Month Progress Report Publication E. Eswar Krishnan, MD 12-Month Progress Report Publication F. Rohit Loomba, MD Publication G. Sharmilee Nyenhuis, MD 12-Month Progress Report Publication H. Peter P. Reese, MD 12-Month Progress Report Publication I. Erik B. Schelbert, MD 12-Month Progress Report Publication J. Helen Keipp Talbot, MD 12-Month Progress Report Publication K. Summary of 18-Month Questionnaire 2010 Williams Scholars Mentor Interviews and Summary of Six-Month Questionnaire L. Kellie Hunter-Campbell, MD Six-Month Mentor Interview M. -

Phage Display-Based Strategies for Cloning and Optimization of Monoclonal Antibodies Directed Against Human Pathogens
Int. J. Mol. Sci. 2012, 13, 8273-8292; doi:10.3390/ijms13078273 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Review Phage Display-based Strategies for Cloning and Optimization of Monoclonal Antibodies Directed against Human Pathogens Nicola Clementi *,†, Nicasio Mancini †, Laura Solforosi, Matteo Castelli, Massimo Clementi and Roberto Burioni Microbiology and Virology Unit, “Vita-Salute” San Raffaele University, Milan 20132, Italy; E-Mails: [email protected] (N.M.); [email protected] (L.S.); [email protected] (M.C.); [email protected] (M.C.); [email protected] (R.B.) † These authors contributed equally to this work. * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +39-2-2643-5082; Fax: +39-2-2643-4288. Received: 16 March 2012; in revised form: 25 June 2012 / Accepted: 27 June 2012 / Published: 4 July 2012 Abstract: In the last two decades, several phage display-selected monoclonal antibodies (mAbs) have been described in the literature and a few of them have managed to reach the clinics. Among these, the anti-respiratory syncytial virus (RSV) Palivizumab, a phage-display optimized mAb, is the only marketed mAb directed against microbial pathogens. Palivizumab is a clear example of the importance of choosing the most appropriate strategy when selecting or optimizing an anti-infectious mAb. From this perspective, the extreme versatility of phage-display technology makes it a useful tool when setting up different strategies for the selection of mAbs directed against human pathogens, especially when their possible clinical use is considered. -

HIV?AIDS Researchers at the NIH Clinical Center
The NIH Clinical Center treats a diverse group of patients from all over the world. It also draws researchers from different cultures and backgrounds. Learn more about some of the many researchers who conduct their work on the human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) at the Clinical Center. Thomas C. Quinn, M.D., M.Sc., conducts research for the National Institute of Allergy and Infectious Diseases at the NIH Clinical Center. He is a senior investigator and chief of the International HIV/STD Section of the Laboratory of Immunoregulation. Dr. Quinn obtained his M.D. from Northwestern University. He was a research associate in infectious diseases in the NIAID Laboratory of Parasitic Diseases and completed a fellowship in infectious diseases at the University of Washington. Since 1981, he has been assigned to the division of infectious diseases at Johns Hopkins University, where he became a professor of medicine in 1991. Dr. Quinn is a member of the Institute of Medicine and the National Academy of Sciences and is a fellow of the American Association for the Advancement of Science. His major areas of research are: Definition of epidemiologic features of HIV-1 and HIV-2 infections in developing countries and the United States Assessment of biomedical interventions to control HIV, including circumcision, prevention of mother-to-child transmission, pre-exposure prophylaxis, and vaccine development Assessment of the frequency of Chlamydia trachomatis infections in selected populations using noninvasive sensitive nucleic-acid amplification assays for diagnosis Evaluations of interventions to control blinding trachoma due to Chlamydia trachomatis in sub-Saharan Africa See the full program description. -

That Record-Breaking Sprint to Create a COVID-19 Vaccine The
NATIONAL INSTITUTES OF HEALTH • OFFICE OF THE DIRECTOR | VOLUME 29 ISSUE 5 • SEPTEMBER-OCTOBER 2021 That Record-breaking The Intersection of Man and Machine Sprint to Create a Bionics Gives New Hope to Those Living With Physical Disabilities COVID-19 Vaccine BY MICHAEL TABASKO, OD BY MELISSA GLIM At the end of 2019, most people were looking forward to an exciting 2020, a new decade starting with those magic numbers, 20-20, that denote a sharpness of vision. There would be the Summer Olympics in Japan and the U.S. presidential election. Meanwhile, intramural scientists at the National Institute of Allergy and Infectious Diseases’ Vaccine Research Center (VRC) were designing vaccines for several coronaviruses using a promising, new platform based on messenger RNA (mRNA). Everything changed on a Saturday morning in early January. Chinese scientists CREDIT: TH0MAS BULEA (LEFT); NIH CLINCAL CENTER (RICHT) had isolated a new coronavirus that was (Left) The NIH pediatric exoskeleton for children with cerebral palsy and other movement disorders uses custom actuators causing a serious epidemic in China’s Wuhan from Agilik developed as part of a cooperative research and development agreement with NIH, along with embedded sensors and microcontrollers, to provide overground gait training while worn. (Right) Alexander Theodorakos, a participant province and released its genetic sequence to in a research protocol at the NIH Clinical Center that is evaluating the new pediatric exoskeleton, and Thomas Bulea, the the scientific community around the world. study’s principal investigator, discuss how the device changes the way the legs move when walking. Barney Graham, director of the VRC’s Viral Pathogenesis Laboratory (VPL), and If popular culture is any indication, the notion that bionic technology will VRC research fellow Kizzmekia Corbett someday redefine the boundaries of human function has long held our collective dropped everything and began using this fascination. -

Synagis, INN-Palivizumab;
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Synagis 50 mg/0.5 ml solution for injection Synagis 100 mg/1 ml solution for injection 2. QUALITATIVE AND QUANTITATIVE COMPOSITION 1 ml of Synagis solution contains 100 mg of palivizumab*. Each 0.5 ml vial contains 50 mg of palivizumab. Each 1 ml vial contains 100 mg of palivizumab. *Palivizumab is a recombinant humanised monoclonal antibody produced by DNA technology in mouse myeloma host cells. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection. The solution is clear or slightly opalescent. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Synagis is indicated for the prevention of serious lower respiratory tract disease requiring hospitalisation caused by respiratory syncytial virus (RSV) in children at high risk for RSV disease: Children born at 35 weeks of gestation or less and less than 6 months of age at the onset of the RSV season. Children less than 2 years of age and requiring treatment for bronchopulmonary dysplasia within the last 6 months. Children less than 2 years of age and with haemodynamically significant congenital heart disease. 4.2 Posology and method of administration Posology The recommended dose of palivizumab is 15 mg/kg of body weight, given once a month during anticipated periods of RSV risk in the community. The volume (expressed in ml) of // Palivizumab // to be administered at one-monthly intervals = [patient weight in kg] multiplied by 0.15. Where possible, the first dose should be administered prior to commencement of the RSV season. -

Medicines/Pharmaceuticals of Animal Origin V3.0 November 2020
Medicines/pharmaceuticals of animal origin V3.0 November 2020 Medicines/pharmaceuticals of animal origin - This guideline provides information for all clinical staff within Hospital and Health Services (HHS) on best practice for avoidance of issues related to animal products. Medicines/pharmaceuticals of animal origin - V3.0 November 2020 Published by the State of Queensland (Queensland Health), November 2020 This document is licensed under a Creative Commons Attribution 3.0 Australia licence. To view a copy of this licence, visit creativecommons.org/licenses/by/3.0/au © State of Queensland (Queensland Health) 2020 You are free to copy, communicate and adapt the work, as long as you attribute the State of Queensland (Queensland Health). For more information contact: Medication Services Queensland, Queensland Health, GPO Box 48, Brisbane QLD 4001, email [email protected] An electronic version of this document is available at https://www.health.qld.gov.au/__data/assets/pdf_file/0024/147507/qh-gdl-954.pdf Disclaimer: The content presented in this publication is distributed by the Queensland Government as an information source only. The State of Queensland makes no statements, representations or warranties about the accuracy, completeness or reliability of any information contained in this publication. The State of Queensland disclaims all responsibility and all liability (including without limitation for liability in negligence) for all expenses, losses, damages and costs you might incur as a result of the information being inaccurate -

Nci-Plan-2013.Pdf
THE NATIONAL CANCER PROGRAM MANAGING THE NATION’S RESEARCH PORTFOLIO AN ANNUAL PLAN AND BUDGET PROPOSAL FOR FISCAL YEAR 2013 National Cancer Institute U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health Contents 1 Foreword 4 Provocative Questions 8 Center for Cancer Genomics 16 Introduction to Cancer Profiles 18 Pancreatic Ductal Adenocarcinoma 22 Colorectal Cancer 26 B-Cell Lymphoma 30 Renal Cell (Kidney) Cancer 34 GI Stromal Cancer 39 Research Focus: Comorbidities 42 Research Focus: Circulating Tumor Cells 44 Research Focus: Reducing Cancer Health Disparities 50 The Frederick National Laboratory for Cancer Research 61 Small Business Innovation Research, Small BusinessTechnology Transfer (SBIR, STTR) 66 NCI Center for Global Health 72 NCI-Designated Cancer Centers 83 Glossary of Terms 84 Budget FOREWORD The National Cancer Program MANAGING THE NATION’S RESEARCH PORTFOLIO his year marks the 75th anniversary of the founding of the National Cancer Institute, the first so-called “categorical institute” of what has become the National Institutes of Health, with its 27 Institutes and Centers. Over the years, the Congress and the public have generously supported the TNCI—and the NIH generally—with sustained budgetary increases. This was especially true for the NCI during the rapid expansion of its budget following the National Cancer Act of 1971 and for the NIH, including the NCI, during the 5-year doubling of its budget, launched in 1998. Both of these eras of rapid growth were remarkably fruitful. The first launched the pursuit of cancer genes and the molecular basis of oncogenesis, laying the foundation for the transformation of clinical oncology that is now occurring. -

NIHAA Update 1Velco111es Lerters and Eastern Europe and at the Undergradu 1968, a Period of Considerable Growth News from Its Readers
The Newsletter of the L NIH Alumni Association Summer 1999 Vol. 11, No. 2 date NIHAA Members Enjoy June Annual Meeting with Henney, Morella Alumni attendi ng the 1999 annual meeting of the NIH.AA were given a first-band briefing on FDA by Dr. Jane E. Henney, the receml y appointed FDA commissioner. Tbe audience also participated in a question and answer exchange witb Rep. Constance A. Morella (R-Md.), who was presented with tbe NIHAA 1999 Public Service Award. Almost I00 alumni attended the June 12 morning meeting at the Mary Woodard Lasker Center on the NIH campus. Henney, wbo was NCI deputy director for five of her lO years at NIH (1985-1995) spoke infonnalJy on some of FDA's principal concerns at this time: the agency's efforts to speed Shown at the NIHAA annual meeting are (from I} NIH alumna Dr. Jane E. Henney, FDA up review without sacrifice of quality commissioner, who spoke on "Back Home Again via Indiana, Kansas and New Mexico," and safeguards; tbe need for recruiting Dr. John F. Sherman, Rep. Constance A. Morella (R-Md.), who received the 1999 NIHAA Public Service Award, and Dr. William S. Jordan, Jr., outgoing NIHAA president. (see A flflual Meeting, p. 12) Director's Advisors Bat 6 for 7 in June Meeting In This Issue Page Choppin To Give Third Research Festival '99 J By Rich McManus NIHAA Shannon Lecture Ca/e11dar 5 The scorecard at the end of a daylong Dr. Purnell W. Cboppin, president of .News .from a11d about Nlf/A;/ me111be1:r (f session of lhe advisory committee to the Howard Hughes Medical lnstirure, the NIH director (ACD) on June 3 read A le11erjro1111he 11e111 Nlf/AIJ preside111 IO will deliver the third James A. -

Study Protocol, Including Amendment
Document Type: Study Protocol, including Amendment (Informed Consent Template located in Appendix I of the Protocol Version 1.0 and Version 2.0) Official Title: A Phase I, Open-Label, Dose-Escalation Study of the Safety and Pharmacokinetics of a Human Monoclonal Antibody, VRC-EBOMAB092-00-AB (MAb114), Administered Intravenously to Healthy Adults NCT Number: NCT03478891 Document/Date: Protocol Amendment Version 2.0: April 6, 2018 Protocol Version 1.0: February 21, 2018 Version 2.0 April 6, 2018 VACCINE RESEARCH CENTER Protocol VRC 608 (NIH 18-I-0069) A PHASE I, OPEN-LABEL, DOSE-ESCALATION STUDY OF THE SAFETY AND PHARMACOKINETICS OF A HUMAN MONOCLONAL ANTIBODY, VRC-EBOMAB092-00-AB (MAB114), ADMINISTERED INTRAVENOUSLY TO HEALTHY ADULTS Study Product Provided by: Vaccine Research Center (VRC) National Institute of Allergy and Infectious Diseases (NIAID) National Institutes of Health (NIH) Bethesda, MD Clinical Trial Sponsored by: NIAID/VRC/NIH, Bethesda, Maryland IND 138,090 Sponsored by: VRC/NIAID/NIH, Bethesda, Maryland Principal Investigator: Martin Gaudinski, MD VRC/NIAID/NIH Bethesda, MD 20892 IRB Initial Review Date: January 8, 2018 PRODUCT: VRC-EBOMAB092-00-AB (MAb114) PROTOCOL: VRC 608, VERSION 2.0 PROTOCOL DATE: APRIL 6, 2018 TABLE OF CONTENTS Page ABBREVIATIONS....................................................................................................................... 5 PRÉCIS.......................................................................................................................................... 8 1. INTRODUCTION............................................................................................................ -
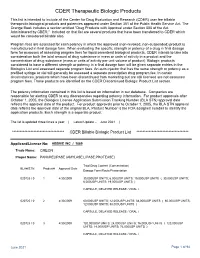
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database. -

See the Vaccine Research Center Brochure
Vaccine Research Center NIAID National Institute of Allergy and Infectious Diseases U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health Letter from John R. Mascola, M.D., NIAID Vaccine Research Center Director, and Anthony S. Fauci, M.D., NIAID Director The Dale and Betty Bumpers Vaccine Research Center (VRC) was created by Presidential Executive Order in 1997 to accelerate the development of a vaccine directed against the devastating global pandemic caused by HIV. The VRC began its vital HIV work in 2000 and has since further expanded its scope and capabilities to combat other high-burden diseases such as influenza, respiratory syncytial virus (RSV), malaria, and tuberculosis, as well as biodefense threats and emerging infectious diseases, including Ebola, chikungunya, severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), West Nile, and Zika. As an intramural research arm of the National Institute of Allergy and Infectious Diseases (NIAID), part of the U.S. National Institutes of Health (NIH), the VRC is led by an integrated team of specialists in various disciplines, including immunology, virology, structural biology, and bioengineering. By encompassing these scientific disciplines under one roof, together with the capability to conduct human clinical trials, the VRC accelerates the process of scientific discovery leading to the design and development of prototype vaccines and biologics to protect against infectious diseases. The VRC operates as the closest analog at NIH to a private -

Vaccine Research Center, NIAID, NIH
4/17/2018 PIPELINE OF HIV MONOCLONAL ANTIBODIES FOR PREVENTION OF HIV Session on Antibody‐Mediated Prevention 2018 Global Vaccine and Immunization Research Forum (GVIRF) 20‐22 March 2018 Bangkok, Thailand Barney S. Graham, MD, PhD Deputy Director Vaccine Research Center, NIAID, NIH Dale and Betty Bumpers Vaccine Research Center Vaccine Research Center National Institute of Allergy and Infectious Diseases National Institutes of Health 2017 VRC Principal Investigators and Program Directors 1 4/17/2018 VRC Research & Development: From AIDS to Zika August 2000 AIDS/HIV Chikungunya Ebola/Marburg Influenza Malaria MERS-CoV, SARS RSV Smallpox Tuberculosis W/E/V equine encephalitis viruses West Nile virus, Zika Engineering Lab Pilot Plant Vaccine Evaluation Clinic Immunology Lab Partners for Advanced Development Functional Activity of Anti-Viral Antibodies • Neutralization – Aggregation – Attachment blocking – Cleavage inhibition – Fusion inhibition – Preventing particle release • Fc‐mediated functions – Antibody dependent cell‐mediated cytotoxicity (NK, Macrophage, Neutrophil) – Complement binding and activation • Opsinization and clearance by non‐susceptible cells • Blocking pathogenic immunomodulatory molecules 2 4/17/2018 Long History of Using Antibodies to Treat Infectious Diseases (Serum Therapy) Shibasaburo Kitasato 1890: Emil von Behring and Shibasaburo Kitasato worked on “anti‐ toxins” for tetanus and diphtheria that led to concept for serum therapy 1901: Emil von Behring ‐ 1901 Nobel Prize in Physiology or Medicine “For his work on serum therapy, especially its application against diphtheria, by which he has opened a new road in the domain of Wernicke, Frosch, and medical science and thereby placed in the hands of the physician a Behring in Koch’s Berlin Lab victorious weapon against illness and deaths".