Development and Challenges to Monoclonal Antibodies for Passive Immunization
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

Where Do Novel Drugs of 2016 Fit In?
FORMULARY JEOPARDY: WHERE DO NOVEL DRUGS OF 2016 FIT IN? Maabo Kludze, PharmD, MBA, CDE, BCPS, Associate Director Elizabeth A. Shlom, PharmD, BCPS, SVP & Director Clinical Pharmacy Program Acurity, Inc. Privileged and Confidential August 15, 2017 Privileged and Confidential Program Objectives By the end of the presentation, the pharmacist or pharmacy technician participant will be able to: ◆ Identify orphan drugs and first-in-class medications approved by the FDA in 2016. ◆ Describe the role of new agents approved for use in oncology patients. ◆ Identify and discuss the role of novel monoclonal antibodies. ◆ Discuss at least two new medications that address public health concerns. Neither Dr. Kludze nor Dr. Shlom have any conflicts of interest in regards to this presentation. Privileged and Confidential 2016 NDA Approvals (NMEs/BLAs) ◆ Nuplazid (primavanserin) P ◆ Adlyxin (lixisenatide) ◆ Ocaliva (obeticholic acid) P, O ◆ Anthim (obitoxaximab) O ◆ Rubraca (rucaparib camsylate) P, O ◆ Axumin (fluciclovive F18) P ◆ Spinraza (nusinersen sodium) P, O ◆ Briviact (brivaracetam) ◆ Taltz (ixekizumab) ◆ Cinqair (reslizumab) ◆ Tecentriq (atezolizumab) P ◆ Defitelio (defibrotide sodium) P, O ◆ Venclexta (venetoclax) P, O ◆ Epclusa (sofosburvir and velpatasvir) P ◆ Xiidra (lifitigrast) P ◆ Eucrisa (crisaborole) ◆ Zepatier (elbasvir and grazoprevir) P ◆ Exondys 51 (eteplirsen) P, O ◆ Zinbyrta (daclizumab) ◆ Lartruvo (olaratumab) P, O ◆ Zinplava (bezlotoxumab) P ◆ NETSTPOT (gallium Ga 68 dotatate) P, O O = Orphan; P = Priority Review; Red = BLA Privileged and Confidential History of FDA Approvals Privileged and Confidential Orphan Drugs ◆FDA Office of Orphan Products Development • Orphan Drug Act (1983) – drugs and biologics . “intended for safe and effective treatment, diagnosis or prevention of rare diseases/disorders that affect fewer than 200,000 people in the U.S. -

Journal Pre-Proof
Journal Pre-proof Neutralizing monoclonal antibodies for COVID-19 treatment and prevention Juan P. Jaworski PII: S2319-4170(20)30209-2 DOI: https://doi.org/10.1016/j.bj.2020.11.011 Reference: BJ 374 To appear in: Biomedical Journal Received Date: 2 September 2020 Revised Date: 6 November 2020 Accepted Date: 22 November 2020 Please cite this article as: Jaworski JP, Neutralizing monoclonal antibodies for COVID-19 treatment and prevention, Biomedical Journal, https://doi.org/10.1016/j.bj.2020.11.011. This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. © 2020 Chang Gung University. Publishing services by Elsevier B.V. TITLE: Neutralizing monoclonal antibodies for COVID-19 treatment and prevention Juan P. JAWORSKI Consejo Nacional de Investigaciones Científicas y Técnicas, Buenos Aires, Argentina Instituto Nacional de Tecnología Agropecuaria, Buenos Aires, Argentina KEYWORDS: SARS-CoV-2, Coronavirus, Monoclonal Antibody, mAb, Prophylaxis, Treatment CORRESPONDING AUTHOR: Dr. Juan Pablo Jaworski, DVM, MSc, PhD. Consejo Nacional de Investigaciones Científicas y Técnicas Instituto de Virología, Instituto Nacional de Tecnología Agropecuaria Las Cabañas y de los Reseros (S/N), Hurlingham (1686), Buenos Aires, Argentina Tel / Fax: 054-11-4621-1447 (int:3400) [email protected] ABSTRACT The SARS-CoV-2 pandemic has caused unprecedented global health and economic crises. -

Phage Display-Based Strategies for Cloning and Optimization of Monoclonal Antibodies Directed Against Human Pathogens
Int. J. Mol. Sci. 2012, 13, 8273-8292; doi:10.3390/ijms13078273 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Review Phage Display-based Strategies for Cloning and Optimization of Monoclonal Antibodies Directed against Human Pathogens Nicola Clementi *,†, Nicasio Mancini †, Laura Solforosi, Matteo Castelli, Massimo Clementi and Roberto Burioni Microbiology and Virology Unit, “Vita-Salute” San Raffaele University, Milan 20132, Italy; E-Mails: [email protected] (N.M.); [email protected] (L.S.); [email protected] (M.C.); [email protected] (M.C.); [email protected] (R.B.) † These authors contributed equally to this work. * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +39-2-2643-5082; Fax: +39-2-2643-4288. Received: 16 March 2012; in revised form: 25 June 2012 / Accepted: 27 June 2012 / Published: 4 July 2012 Abstract: In the last two decades, several phage display-selected monoclonal antibodies (mAbs) have been described in the literature and a few of them have managed to reach the clinics. Among these, the anti-respiratory syncytial virus (RSV) Palivizumab, a phage-display optimized mAb, is the only marketed mAb directed against microbial pathogens. Palivizumab is a clear example of the importance of choosing the most appropriate strategy when selecting or optimizing an anti-infectious mAb. From this perspective, the extreme versatility of phage-display technology makes it a useful tool when setting up different strategies for the selection of mAbs directed against human pathogens, especially when their possible clinical use is considered. -

Bezlotoxumab (Zinplava®)
Zinplava Swiss Risk Management Plan Summary V1.5 Swiss Summary of the Risk Management Plan (RMP) for Zinplava® (Bezlotoxumab 1000mg) Concentrate for solution for infusion Version 1.5 (November 2016) The Risk Management Plan (RMP) is a comprehensive document submitted as part of the application dossier for market approval of a medicine. The RMP summary contains information on the medicine's safety profile and explains the measures that are taken in order to further investigate and follow the risks as well as to prevent or minimise them. The RMP summary of Zinplava® is a concise document and does not claim to be exhaustive. As the RMP is an international document, the summary might differ from the “Arzneimittelinformation / Information sur le médicament” approved and published in Switzerland, e.g. by mentioning risks occurring in populations or indications not included in the Swiss authorisation. Please note that the reference document which is valid and relevant for the effective and safe use of Zinplava® in Switzerland is the “Arzneimittelinformation / Information sur le médicament” (see www.swissmedicinfo.ch) approved and authorized by Swissmedic. MSD Merck Sharp & Dohme AG is fully responsible for the accuracy and correctness of the content of the published summary RMP of Zinplava®. Zinplava Swiss Risk Management Plan Summary V1.5 1 Elements for Summary Tables in the EPAR 1.1 Summary Table of Safety Concerns Table 1 Summary of Safety Concerns Important identified risks None Important potential risks Infusion-related Reactions Including -

The Effect of Raxibacumab on the Immunogenicity of Anthrax Vaccine Adsorbed: a Phase
The effect of raxibacumab on the immunogenicity of anthrax vaccine adsorbed: a Phase IV, randomised, open-label, parallel-group, non-inferiority study Nancy Skoura, PhD1, Jie Wang-Jairaj, MD2, Oscar Della Pasqua MD2, Vijayalakshmi Chandrasekaran, MS1, Julia Billiard, PhD1, Anne Yeakey, MD3, William Smith, MD4, Helen Steel, MD2, Lionel K Tan, FRCP2 1GlaxoSmithKline, Inc. Collegeville, PA, USA 2GlaxoSmithKline. Stockley Park West, Middlesex, UK 3GlaxoSmithKline, Inc. Rockville, MD, USA 4AMR, at University of TN Medical Center, Knoxville, TN; New Orleans Center for Clinical Research (NOCCR), USA Author for Correspondence: Dr Lionel K Tan GlaxoSmithKline Stockley Park West 1–3 Ironbridge Road Uxbridge Middlesex UB11 1BT UK Email: [email protected] Tel: +44 (0)7341 079 683 1 Abstract: 340/350 Body text: 4321/4500 words including Research in Context Table/Figures: 2/4 References: 30 2 Abstract Background Raxibacumab is a monoclonal antibody (Ab) which binds protective antigen (PA) of Bacillus anthracis and is approved for treatment and post-exposure prophylaxis (PEP) of inhalational anthrax. Anthrax vaccine adsorbed (AVA), for anthrax prophylaxis, consists primarily of adsorbed PA. This post-approval study evaluated the effect of raxibacumab on immunogenicity of AVA. Methods In this open-label, parallel-group, non-inferiority study in three centres in the USA, healthy volunteers (aged 18–65 years) with no evidence of PA pre-exposure were randomised 1:1 to receive either subcutaneous 0·5 mL AVA on Days 1, 15, and 29 or raxibacumab intravenous infusion (40 mg/kg) immediately before AVA on Day 1, followed by AVA only on Days 15 and 29. -

Revenue Codes with Special Linkages
INDIANA HEALTH COVERAGE PROGRAMS PROVIDER CODE TABLES Revenue Codes with Special Procedure Code Linkages Note: Due to possible changes in Indiana Health Coverage Programs (IHCP) policy or national coding updates, inclusion of a code on the code tables does not necessarily indicate current coverage. See IHCP Banner Pages and Bulletins and the IHCP Fee Schedules for updates to coding, coverage, and benefit information. For information about using this code table, see the Claim Submission and Processing provider reference module. Table 1 – Procedure Codes Linked to Revenue Code 260 – IV Therapy – General Table 2 – Procedure Codes Linked to Revenue Code 274 – Prosthetic/Orthotic Devices Table 3 – Procedure Codes Linked to Revenue Code 636 – Drugs Requiring Detailed Coding Table 4 – Procedure Code Linked to Revenue Code 724 – Labor Room/Delivery – Birthing Center Table 5 – Procedure Codes Linked to Revenue Code 920 – Other Diagnostic Services – General Table 6 – Procedure Codes Linked to Revenue Code 929 – Other Diagnostic Services Table 7 – Procedure Codes Linked to Revenue Code 940 – Other Therapeutic Services – General Table 8 – Procedure Codes Linked to Revenue Codes for Managed Care Billing Only (Revenue Codes 912, 913, and 960) Published: September 16, 2021 1 Indiana Health Coverage Programs Revenue Codes with Special Procedure Code Linkages Table 1 – Procedure Codes Linked to Revenue Code 260 – IV Therapy – General Reviewed/Updated: June 8, 2021 Note: The procedure codes in this table may be billed with revenue code 260 to receive separate reimbursement when billed on the same date of service as a treatment room revenue code. Injection administration (including vaccine administration) is included in the reimbursement for treatment rooms. -

Synagis, INN-Palivizumab;
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Synagis 50 mg/0.5 ml solution for injection Synagis 100 mg/1 ml solution for injection 2. QUALITATIVE AND QUANTITATIVE COMPOSITION 1 ml of Synagis solution contains 100 mg of palivizumab*. Each 0.5 ml vial contains 50 mg of palivizumab. Each 1 ml vial contains 100 mg of palivizumab. *Palivizumab is a recombinant humanised monoclonal antibody produced by DNA technology in mouse myeloma host cells. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection. The solution is clear or slightly opalescent. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Synagis is indicated for the prevention of serious lower respiratory tract disease requiring hospitalisation caused by respiratory syncytial virus (RSV) in children at high risk for RSV disease: Children born at 35 weeks of gestation or less and less than 6 months of age at the onset of the RSV season. Children less than 2 years of age and requiring treatment for bronchopulmonary dysplasia within the last 6 months. Children less than 2 years of age and with haemodynamically significant congenital heart disease. 4.2 Posology and method of administration Posology The recommended dose of palivizumab is 15 mg/kg of body weight, given once a month during anticipated periods of RSV risk in the community. The volume (expressed in ml) of // Palivizumab // to be administered at one-monthly intervals = [patient weight in kg] multiplied by 0.15. Where possible, the first dose should be administered prior to commencement of the RSV season. -

761046Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 761046Orig1s000 MICROBIOLOGY/VIROLOGY REVIEW(S) Division of Anti-Infective Products Clinical microbiology Review BLA761046 Bezlotoxumab BLA: 761046 Date Submitted: 11-22-15 Date Received by CDER: 11-23-15 Date Assigned: 12-1-15 Date Completed: 4-19-16 Reviewer: Kerian Grande Roche, Ph.D. APPLICANT: Merck Sharp and Dohme Corp., a subsidiary of Merck and Co., Inc. (Merck) DRUG PRODUCT NAMES: Proprietary: Bezlotoxumab Nonproprietary: CDB1, MK6072 Antibody Class: IgG1/kappa isotype subclass Molecular Weight: 148.2 kDa DRUG CATEGORY: Human monoclonal antibody to C. difficile Toxin B PROPOSED INDICATION: Prevention of Clostridium difficile infection (CDI) recurrence in patients 18 years or older receiving antibiotic therapy for CDI PROPOSED DOSAGE FORM, STRENGTH, ROUTE OF ADMINISTRATION AND DURATION OF TREATMENT: MK-6072 drug product is a sterile, aqueous solution. Vials contain a target deliverable dose of 40 mL of 25mg/mL MK-6072 for a total of 1000 mg per vial. MK-6072 drug product is diluted (b) (4) prior to administration. The recommended dose of bezlotoxumab is 10 mg/kg by intravenous infusion over 60 minutes in one dose. DISPENSED: Rx RELATED PRODUCTS: N/A REMARKS: This submission is for an original Biologics License Application (BLA) for bezlotoxumab injection for intravenous use. Bezlotoxumab (MK-6072) is a fully human monoclonal antibody (mAb) of the IgG1/kappa isotype subclass that binds to Clostridium difficile (C. difficile) toxin B. CONCLUSIONS AND RECOMMENDATIONS: From clinical microbiology perspective, this BLA submission is approvable pending an accepted version of the labeling. See FDA’s proposed version of the microbiology section of the labeling below (this may not be the final Agency label as discussions are still ongoing). -

Medicines/Pharmaceuticals of Animal Origin V3.0 November 2020
Medicines/pharmaceuticals of animal origin V3.0 November 2020 Medicines/pharmaceuticals of animal origin - This guideline provides information for all clinical staff within Hospital and Health Services (HHS) on best practice for avoidance of issues related to animal products. Medicines/pharmaceuticals of animal origin - V3.0 November 2020 Published by the State of Queensland (Queensland Health), November 2020 This document is licensed under a Creative Commons Attribution 3.0 Australia licence. To view a copy of this licence, visit creativecommons.org/licenses/by/3.0/au © State of Queensland (Queensland Health) 2020 You are free to copy, communicate and adapt the work, as long as you attribute the State of Queensland (Queensland Health). For more information contact: Medication Services Queensland, Queensland Health, GPO Box 48, Brisbane QLD 4001, email [email protected] An electronic version of this document is available at https://www.health.qld.gov.au/__data/assets/pdf_file/0024/147507/qh-gdl-954.pdf Disclaimer: The content presented in this publication is distributed by the Queensland Government as an information source only. The State of Queensland makes no statements, representations or warranties about the accuracy, completeness or reliability of any information contained in this publication. The State of Queensland disclaims all responsibility and all liability (including without limitation for liability in negligence) for all expenses, losses, damages and costs you might incur as a result of the information being inaccurate -
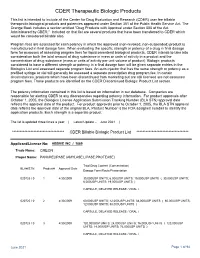
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database. -

A Review of the Efficacy of FDA-Approved B. Anthracis Anti
toxins Review A Review of the Efficacy of FDA-Approved B. anthracis Anti-Toxin Agents When Combined with Antibiotic or Hemodynamic Support in Infection- or Toxin-Challenged Preclinical Models Zoe Couse 1, Xizhong Cui 1, Yan Li 1, Mahtab Moayeri 2, Stephen Leppla 2 and Peter Q. Eichacker 1,* 1 Critical Care Medicine Department, Clinical Center, National Institutes of Health, Bethesda, MD 20892, USA; [email protected] (Z.C.); [email protected] (X.C.); [email protected] (Y.L.) 2 National Institutes of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, MD 20892, USA; [email protected] (M.M.); [email protected] (S.L.) * Correspondence: [email protected] Abstract: Anti-toxin agents for severe B. anthracis infection will only be effective if they add to the benefit of the two mainstays of septic shock management, antibiotic therapy and titrated hemody- namic support. Both of these standard therapies could negate benefits related to anti-toxin treatment. At present, three anthrax anti-toxin antibody preparations have received US Food and Drug Adminis- tration (FDA) approval: Raxibacumab, Anthrax Immune Globulin Intravenous (AIGIV) and ETI-204. Each agent is directed at the protective antigen component of lethal and edema toxin. All three agents were compared to placebo in antibiotic-treated animal models of live B. anthracis infection, and Raxibacumab and AIGIV were compared to placebo when combined with standard hemodynamic support in a 96 h canine model of anthrax toxin-associated shock. However, only AIG has actually Citation: Couse, Z.; Cui, X.; Li, Y.; been administered to a group of infected patients, and this experience was not controlled and offers Moayeri, M.; Leppla, S.; Eichacker, P.Q.