Studies on Antitoxin Use for Postexposure Prophylaxis (PEP)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

Where Do Novel Drugs of 2016 Fit In?
FORMULARY JEOPARDY: WHERE DO NOVEL DRUGS OF 2016 FIT IN? Maabo Kludze, PharmD, MBA, CDE, BCPS, Associate Director Elizabeth A. Shlom, PharmD, BCPS, SVP & Director Clinical Pharmacy Program Acurity, Inc. Privileged and Confidential August 15, 2017 Privileged and Confidential Program Objectives By the end of the presentation, the pharmacist or pharmacy technician participant will be able to: ◆ Identify orphan drugs and first-in-class medications approved by the FDA in 2016. ◆ Describe the role of new agents approved for use in oncology patients. ◆ Identify and discuss the role of novel monoclonal antibodies. ◆ Discuss at least two new medications that address public health concerns. Neither Dr. Kludze nor Dr. Shlom have any conflicts of interest in regards to this presentation. Privileged and Confidential 2016 NDA Approvals (NMEs/BLAs) ◆ Nuplazid (primavanserin) P ◆ Adlyxin (lixisenatide) ◆ Ocaliva (obeticholic acid) P, O ◆ Anthim (obitoxaximab) O ◆ Rubraca (rucaparib camsylate) P, O ◆ Axumin (fluciclovive F18) P ◆ Spinraza (nusinersen sodium) P, O ◆ Briviact (brivaracetam) ◆ Taltz (ixekizumab) ◆ Cinqair (reslizumab) ◆ Tecentriq (atezolizumab) P ◆ Defitelio (defibrotide sodium) P, O ◆ Venclexta (venetoclax) P, O ◆ Epclusa (sofosburvir and velpatasvir) P ◆ Xiidra (lifitigrast) P ◆ Eucrisa (crisaborole) ◆ Zepatier (elbasvir and grazoprevir) P ◆ Exondys 51 (eteplirsen) P, O ◆ Zinbyrta (daclizumab) ◆ Lartruvo (olaratumab) P, O ◆ Zinplava (bezlotoxumab) P ◆ NETSTPOT (gallium Ga 68 dotatate) P, O O = Orphan; P = Priority Review; Red = BLA Privileged and Confidential History of FDA Approvals Privileged and Confidential Orphan Drugs ◆FDA Office of Orphan Products Development • Orphan Drug Act (1983) – drugs and biologics . “intended for safe and effective treatment, diagnosis or prevention of rare diseases/disorders that affect fewer than 200,000 people in the U.S. -

Phage Display-Based Strategies for Cloning and Optimization of Monoclonal Antibodies Directed Against Human Pathogens
Int. J. Mol. Sci. 2012, 13, 8273-8292; doi:10.3390/ijms13078273 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Review Phage Display-based Strategies for Cloning and Optimization of Monoclonal Antibodies Directed against Human Pathogens Nicola Clementi *,†, Nicasio Mancini †, Laura Solforosi, Matteo Castelli, Massimo Clementi and Roberto Burioni Microbiology and Virology Unit, “Vita-Salute” San Raffaele University, Milan 20132, Italy; E-Mails: [email protected] (N.M.); [email protected] (L.S.); [email protected] (M.C.); [email protected] (M.C.); [email protected] (R.B.) † These authors contributed equally to this work. * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +39-2-2643-5082; Fax: +39-2-2643-4288. Received: 16 March 2012; in revised form: 25 June 2012 / Accepted: 27 June 2012 / Published: 4 July 2012 Abstract: In the last two decades, several phage display-selected monoclonal antibodies (mAbs) have been described in the literature and a few of them have managed to reach the clinics. Among these, the anti-respiratory syncytial virus (RSV) Palivizumab, a phage-display optimized mAb, is the only marketed mAb directed against microbial pathogens. Palivizumab is a clear example of the importance of choosing the most appropriate strategy when selecting or optimizing an anti-infectious mAb. From this perspective, the extreme versatility of phage-display technology makes it a useful tool when setting up different strategies for the selection of mAbs directed against human pathogens, especially when their possible clinical use is considered. -

The Effect of Raxibacumab on the Immunogenicity of Anthrax Vaccine Adsorbed: a Phase
The effect of raxibacumab on the immunogenicity of anthrax vaccine adsorbed: a Phase IV, randomised, open-label, parallel-group, non-inferiority study Nancy Skoura, PhD1, Jie Wang-Jairaj, MD2, Oscar Della Pasqua MD2, Vijayalakshmi Chandrasekaran, MS1, Julia Billiard, PhD1, Anne Yeakey, MD3, William Smith, MD4, Helen Steel, MD2, Lionel K Tan, FRCP2 1GlaxoSmithKline, Inc. Collegeville, PA, USA 2GlaxoSmithKline. Stockley Park West, Middlesex, UK 3GlaxoSmithKline, Inc. Rockville, MD, USA 4AMR, at University of TN Medical Center, Knoxville, TN; New Orleans Center for Clinical Research (NOCCR), USA Author for Correspondence: Dr Lionel K Tan GlaxoSmithKline Stockley Park West 1–3 Ironbridge Road Uxbridge Middlesex UB11 1BT UK Email: [email protected] Tel: +44 (0)7341 079 683 1 Abstract: 340/350 Body text: 4321/4500 words including Research in Context Table/Figures: 2/4 References: 30 2 Abstract Background Raxibacumab is a monoclonal antibody (Ab) which binds protective antigen (PA) of Bacillus anthracis and is approved for treatment and post-exposure prophylaxis (PEP) of inhalational anthrax. Anthrax vaccine adsorbed (AVA), for anthrax prophylaxis, consists primarily of adsorbed PA. This post-approval study evaluated the effect of raxibacumab on immunogenicity of AVA. Methods In this open-label, parallel-group, non-inferiority study in three centres in the USA, healthy volunteers (aged 18–65 years) with no evidence of PA pre-exposure were randomised 1:1 to receive either subcutaneous 0·5 mL AVA on Days 1, 15, and 29 or raxibacumab intravenous infusion (40 mg/kg) immediately before AVA on Day 1, followed by AVA only on Days 15 and 29. -
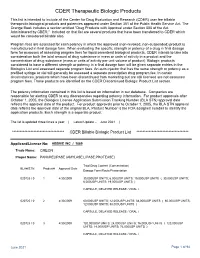
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database. -

A Review of the Efficacy of FDA-Approved B. Anthracis Anti
toxins Review A Review of the Efficacy of FDA-Approved B. anthracis Anti-Toxin Agents When Combined with Antibiotic or Hemodynamic Support in Infection- or Toxin-Challenged Preclinical Models Zoe Couse 1, Xizhong Cui 1, Yan Li 1, Mahtab Moayeri 2, Stephen Leppla 2 and Peter Q. Eichacker 1,* 1 Critical Care Medicine Department, Clinical Center, National Institutes of Health, Bethesda, MD 20892, USA; [email protected] (Z.C.); [email protected] (X.C.); [email protected] (Y.L.) 2 National Institutes of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, MD 20892, USA; [email protected] (M.M.); [email protected] (S.L.) * Correspondence: [email protected] Abstract: Anti-toxin agents for severe B. anthracis infection will only be effective if they add to the benefit of the two mainstays of septic shock management, antibiotic therapy and titrated hemody- namic support. Both of these standard therapies could negate benefits related to anti-toxin treatment. At present, three anthrax anti-toxin antibody preparations have received US Food and Drug Adminis- tration (FDA) approval: Raxibacumab, Anthrax Immune Globulin Intravenous (AIGIV) and ETI-204. Each agent is directed at the protective antigen component of lethal and edema toxin. All three agents were compared to placebo in antibiotic-treated animal models of live B. anthracis infection, and Raxibacumab and AIGIV were compared to placebo when combined with standard hemodynamic support in a 96 h canine model of anthrax toxin-associated shock. However, only AIG has actually Citation: Couse, Z.; Cui, X.; Li, Y.; been administered to a group of infected patients, and this experience was not controlled and offers Moayeri, M.; Leppla, S.; Eichacker, P.Q. -

RAXIBACUMAB Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all of the information needed to use RAXIBACUMAB safely and effectively. See full prescribing information --------------------DOSAGE FORMS AND STRENGTHS---------------- for RAXIBACUMAB. Single-use vial contains 1700 mg/34 mL (50 mg/mL) raxibacumab solution. (3) RAXIBACUMAB injection, for intravenous use Initial U.S. Approval: 2012 ----------------------------- CONTRAINDICATIONS--- ---------------------- None. (4) -------------------------- INDICATIONS AND USAGE--- ------------------- Raxibacumab is indicated for the treatment of adult and pediatric patients with ----------------------WARNINGS AND PRECAUTIONS--- --------------- inhalational anthrax due to Bacillus anthracis in combination with appropriate Infusion reactions may occur. Premedicate with diphenhydramine. Slow or antibacterial drugs, and for prophylaxis of inhalational anthrax when interrupt infusion and administer treatment based on severity of the reaction. alternative therapies are not available or are not appropriate. (1) (5.1) Limitations of Use: The effectiveness of raxibacumab is based solely on efficacy studies in -----------------------------ADVERSE REACTIONS--- ---------------------- animal models of inhalational anthrax. (1.2, 14.1) Common adverse reactions in healthy adult subjects (≥1.5%) were: rash, pain There have been no studies of raxibacumab in the pediatric population. in extremity, pruritus, and somnolence. (6.1) Dosing in pediatric patients was derived using a population PK approach. -

ENTRY WATCH 2016 Published by the Patented Medicine Prices Review Board June 2018 Meds Entry Watch, 2016 Is Available in Electronic Format on the PMPRB Website
MEDS ENTRY WATCH 2016 Published by the Patented Medicine Prices Review Board June 2018 Meds Entry Watch, 2016 is available in electronic format on the PMPRB website. Une traduction de ce document est également disponible en français sous le titre : Veille des médicaments mis en marché, 2016 Patented Medicine Prices Review Board Standard Life Centre Box L40 333 Laurier Avenue West Suite 1400 Ottawa, ON K1P 1C1 Tel.: 1-877-861-2350 TTY 613-288-9654 Email: [email protected] Web: www.pmprb-cepmb.gc.ca ISSN 2560-6204 Cat. No.: H79-12E-PDF © Her Majesty the Queen in Right of Canada, as represented by the NPDUIS initiative of the Patented Medicine Prices Review Board, 2018 MEDS ENTRY WATCH 2016 About the PMPRB Acknowledgements The Patented Medicine Prices Review Board This report was prepared by the Patented (PMPRB) is a respected public agency that makes Medicine Prices Review Board (PMPRB) a unique and valued contribution to sustainable as part of the National Prescription Drug spending on pharmaceuticals in Canada by: Utilization Information System (NPDUIS). ~ providing stakeholders with price, cost and The PMPRB would like to acknowledge the utilization information to help them make timely contributions of and knowledgeable drug pricing, purchasing and ~ The members of the NPDUIS Advisory reimbursement decisions; and Committee for their expert oversight and ~ acting as an effective check on the patent rights guidance in the preparation of this report. of pharmaceutical manufacturers through the ~ PMPRB NPDUIS staff for their contribution responsible and efficient use of its consumer to the analytical content of the report: protection powers. -

Boosting Anti-Infective Antibody and Vaccine Development
ADVERTISEMENT FEATURE YUMAB GmbH www.yumab.com YUMAB: boosting anti-infective antibody and vaccine development YUMAB, a global provider of fully human monoclonal antibody discovery and development, has relocated its headquarters to Germany’s hotspot of infectious research and is advancing new opportunities for the expedited development of prophylactic and therapeutic antibodies and vaccines to fight infectious diseases. Biotechnology company YUMAB, a global provider The combination of deep expertise in infectious of fully human monoclonal antibody (mAb) dis- Therapeutics disease and an advanced fully human mAb discov- covery and development, has recently relocated its ery and development platform makes YUMAB an profile headquarters and research and development labs to ideal partner to drive infectious disease programs Science Campus Braunschweig-South, Germany’s Pathogens YUMAB® PLATFORM Vaccines from basic research to clinical translation. The fully infectious disease research hotspot. YUMAB is now human mAbs developed at YUMAB can be tailored colocated with the Helmholtz Centre of Infection to the specific needs of any kind of mAb develop- Diagnostics Research (HZI), the Leibniz Institute-German ment program, at any stage, and with the properties Collection of Microorganisms and Cell Cultures needed for novel prophylactic or therapeutic strate- (DSMZ) and the German Centre for Infection Research gies against infectious diseases. (DZIF): three world leaders in the fight against infec- Fig. 1| Driving anti-infective mAbs with YUMAB’s tious diseases that provide an ideal environment for fully human mAb and target discovery and Partnering to fight infectious diseases YUMAB to expand its global collaboration network development platform. YUMAB is committed to accelerating the develop- in this space. -
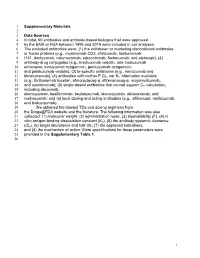
1 Supplementary Materials 1 2 Data Sources 3 in Total, 60 Antibodies
1 Supplementary Materials 2 3 Data Sources 4 In total, 60 antibodies and antibody-based biologics that were approved 5 by the EMA or FDA between 1995 and 2019 were included in our analyses. 6 The excluded antibodies were: (1) the withdrawn or marketing discontinued antibodies 7 or fusion proteins (e.g., muromonab-CD3, efalizumab, tositumomab- 8 I131, daclizumab, catumaxomab, edrecolomab, Nebacumab, and alefacept); (2) 9 antibody-drug conjugates (e.g., brentuximab vedotin, ado-trastuzumab 10 emtansine, inotuzumab ozogamicin, gemtuzumab ozogamicin, 11 and polatuzumab vedotin); (3) bi-specific antibodies (e.g., emicizumab and 12 blinatumomab); (4) antibodies with neither F CL, nor KD information available 13 (e.g., Ibritumomab tiuxetan, efmoroctocog-α, eftrenonacog-α, mogamulizumab, 14 and ustekinumab); (5) single-dosed antibodies that cannot support Css calculation, 15 including abciximab, 16 alemtuzumab, basiliximmab, bezlotoxumab, idarucizumab, obiloxaximab, and 17 raxibacumab; and (6) local dosing and acting antibodies (e.g., aflibercept, ranibizumab, 18 and brolucizumab). 19 We obtained the labeled TDs and dosing regimens from 20 the Drugs@FDA website and the literature. The following information was also 21 collected: (1) molecular weight, (2) administration route, (3) bioavailability (F), (4) in 22 vitro antigen-binding dissociation constant (KD), (5) the antibody systemic clearance 23 (CL), (6) target abundance and half-life, (7) the approved indications, 24 and (8) the mechanism of action. More specifications for these parameters were 25 provided in the Supplementary Table 1. 26 1 27 Supplementary Figure 1 28 29 30 Supplementary Figure 1. Target turnovers are not relevant to TEARs in four 31 disease-target scenarios. Dots represent the mean values. -

Therapeutic Monoclonal Antibodies for Respiratory Diseases: Current Challenges & Perspectives March 31 - April 1, 2016
Therapeutic Monoclonal Antibodies for Respiratory Diseases: Current Challenges & Perspectives March 31 - April 1, 2016 Janice M. Reichert, Ph.D. Executive Director, The Antibody Society Editor-in-Chief, mAbs 1 Topics for discussion Overview of the antibody therapeutics clinical pipeline* ‘Other’ disorders, incl. respiratory disorders Antibodies recently approved or in regulatory review Antibodies in clinical studies Prospects for 2016 *Disclaimer: Commercial development; only public domain information known as of Feb 15, 2016 is included. It should be noted that frequent changes to the data occur over time. 2 3 Novel antibodies entering clinic* 120 102 100 81 80 66 54 60 50 40 20 0 2011 2012 2013 2014 2015 Year of first clinical study *Commercial development only Antibodies in Phase 3 studies 60 53 50 39 40 33 29 30 26 25 25 20 Number of mAbs in Phase 3 Phase in mAbs of Number 10 0 2010 2011 2012 2013 2014 2015 2016 Year of article publication Data from ‘Antibodies to watch’ articles published in mAbs. 5 10 11 Number of first approvals for mAbs of mAbs US or EU approvals First 0 1 2 3 4 5 6 7 8 9 the US or EU (antibodysociety.org) or US the in or in review approved of antibodies Table Source: approvals. number of first *Projected 97 98 99 00 01 02 Year of first US EUor approval of first Year 03 04 05 06 07 08 09 10 11 12 13 14 15 10+ ? 6 16* Three approvals in 2016 so far… Obiltoxaximab, targeting PA of B. anthracis exotoxin approved by FDA on March 18 ANTHIM® is indicated in adult and pediatric patients for treatment of inhalational anthrax due to Bacillus anthracis in combination with appropriate antibacterial drugs, and for prophylaxis of inhalational anthrax when alternative therapies are not available or appropriate. -

Monoclonal Antibodies for Infectious Diseases
Monoclonal antibodies for infectious diseases Martin Friede 1890: Emil von Behring and Shibasaburo Kitasato From anti-toxin to the serotherapy of diptheria, tetanus Nobel prize for von Behring in 1901 2 | The birth of anti-infectives 3 | A century of trials and success Diptheria Influenza (pandemic) Tetanus Haemophilus influenza Rabies Pseudomonas Hepatitis A & B Malaria Varicella Polio RSV Hemorhagic fever Pneumococcus Ebola (?) Meningococcus …. And others 4 | And still a strong demand Procurement by PAHO revolving fund (doses) 2009 2010 2011 2012 Tetanus 14000 5000 17000 32000 Rabies 15000 16000 31000 40000 Hepatitis B 47000 48000 5000 72000 Varicella 12000 15000 23000 21000 5 | The Birth of Monoclonal antibodies 1975 Cesar Milstein and Georges Köhler develop technique for making monoclonal antibodies Nobel prize: 1982 "Developed as a "research tool…" Currently $140,000,000,000 / year market 6 | The pros and cons of monoclonal antibodies for infectious diseases Safety theoretically easy to predict (but not always…) Functions rapidly (unlike vaccines) Quicker to develop than vaccines Supply: limited ! Cost: !!!!! Especially when grams of product needed ! Time to development !! 7 | mAbs in infectious disease Palivizumab: anti-RSV mAb (Medimmune 1998) – First monoclonal approved for prophylaxis of infectious disease (RSV). – For premature infants (<29 weeks), CHF, bronchopulmonary dysplasia. – $7000-10,000 per treatment course (4-5 months). Raxibacumab: anti-anthrax mAb (GSK 2012) – Approved using animal rule – For treatment of inhalation anthrax. 8 | Improved production systems Murine myeloma NS0 cells Variable glycosylation CHO cells patterns -> immunogenicity, function PerC6 Tobacco plants Yield 0.1g/l 10g/l Technical skills barrier, Technology access barrier, Cost of goods: $10,000/g $100g CAPEX barrier.