(RSV F) to Elicit High Neutralizing Antibody Titers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Journal Pre-Proof
Journal Pre-proof Neutralizing monoclonal antibodies for COVID-19 treatment and prevention Juan P. Jaworski PII: S2319-4170(20)30209-2 DOI: https://doi.org/10.1016/j.bj.2020.11.011 Reference: BJ 374 To appear in: Biomedical Journal Received Date: 2 September 2020 Revised Date: 6 November 2020 Accepted Date: 22 November 2020 Please cite this article as: Jaworski JP, Neutralizing monoclonal antibodies for COVID-19 treatment and prevention, Biomedical Journal, https://doi.org/10.1016/j.bj.2020.11.011. This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. © 2020 Chang Gung University. Publishing services by Elsevier B.V. TITLE: Neutralizing monoclonal antibodies for COVID-19 treatment and prevention Juan P. JAWORSKI Consejo Nacional de Investigaciones Científicas y Técnicas, Buenos Aires, Argentina Instituto Nacional de Tecnología Agropecuaria, Buenos Aires, Argentina KEYWORDS: SARS-CoV-2, Coronavirus, Monoclonal Antibody, mAb, Prophylaxis, Treatment CORRESPONDING AUTHOR: Dr. Juan Pablo Jaworski, DVM, MSc, PhD. Consejo Nacional de Investigaciones Científicas y Técnicas Instituto de Virología, Instituto Nacional de Tecnología Agropecuaria Las Cabañas y de los Reseros (S/N), Hurlingham (1686), Buenos Aires, Argentina Tel / Fax: 054-11-4621-1447 (int:3400) [email protected] ABSTRACT The SARS-CoV-2 pandemic has caused unprecedented global health and economic crises. -

Phage Display-Based Strategies for Cloning and Optimization of Monoclonal Antibodies Directed Against Human Pathogens
Int. J. Mol. Sci. 2012, 13, 8273-8292; doi:10.3390/ijms13078273 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Review Phage Display-based Strategies for Cloning and Optimization of Monoclonal Antibodies Directed against Human Pathogens Nicola Clementi *,†, Nicasio Mancini †, Laura Solforosi, Matteo Castelli, Massimo Clementi and Roberto Burioni Microbiology and Virology Unit, “Vita-Salute” San Raffaele University, Milan 20132, Italy; E-Mails: [email protected] (N.M.); [email protected] (L.S.); [email protected] (M.C.); [email protected] (M.C.); [email protected] (R.B.) † These authors contributed equally to this work. * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +39-2-2643-5082; Fax: +39-2-2643-4288. Received: 16 March 2012; in revised form: 25 June 2012 / Accepted: 27 June 2012 / Published: 4 July 2012 Abstract: In the last two decades, several phage display-selected monoclonal antibodies (mAbs) have been described in the literature and a few of them have managed to reach the clinics. Among these, the anti-respiratory syncytial virus (RSV) Palivizumab, a phage-display optimized mAb, is the only marketed mAb directed against microbial pathogens. Palivizumab is a clear example of the importance of choosing the most appropriate strategy when selecting or optimizing an anti-infectious mAb. From this perspective, the extreme versatility of phage-display technology makes it a useful tool when setting up different strategies for the selection of mAbs directed against human pathogens, especially when their possible clinical use is considered. -

Pharmacokinetic-Pharmacodynamic Modelling of Systemic IL13 Blockade by Monoclonal Antibody Therapy: a Free Assay Disguised As Total
pharmaceutics Article Pharmacokinetic-Pharmacodynamic Modelling of Systemic IL13 Blockade by Monoclonal Antibody Therapy: A Free Assay Disguised as Total John Hood 1,*, Ignacio González-García 1 , Nicholas White 1, Leeron Marshall 1,2, Vincent F. S. Dubois 1 , Paolo Vicini 1,3 and Paul G. Baverel 1,4 1 Clinical Pharmacology and Quantitative Pharmacology, AstraZeneca, Cambridge CB21 6GH, UK; [email protected] (I.G.-G.); [email protected] (N.W.); [email protected] (L.M.); [email protected] (V.F.S.D.); [email protected] (P.V.); [email protected] (P.G.B.) 2 Salford Royal Foundation Trust, Salford M6 8HD, UK 3 Confo Therapeutics, 9052 Ghent, Zwijnaarde, Belgium 4 Roche Pharma Research and Early Development, Clinical Pharmacology, Pharmaceutical Sciences, Roche Innovation Center Basel F. Hoffmann-La Roche Ltd., CH-4070 Basel, Switzerland * Correspondence: [email protected]; Tel.: +44-1223-749-6288 Abstract: A sequential pharmacokinetic (PK) and pharmacodynamic (PD) model was built with Nonlinear Mixed Effects Modelling based on data from a first-in-human trial of a novel biologic, MEDI7836. MEDI7836 is a human immunoglobulin G1 lambda (IgG1λ-YTE) monoclonal antibody, Citation: Hood, J.; González-García, with an Fc modification to reduce metabolic clearance. MEDI7836 specifically binds to, and function- I.; White, N.; Marshall, L.; Dubois, ally neutralizes interleukin-13. Thirty-two healthy male adults were enrolled into a dose-escalation V.F.S.; Vicini, P.; Baverel, P.G. clinical trial. Four active doses were tested (30, 105, 300, and 600 mg) with 6 volunteers enrolled Pharmacokinetic-Pharmacodynamic per cohort. Eight volunteers received placebo as control. -

Synagis, INN-Palivizumab;
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Synagis 50 mg/0.5 ml solution for injection Synagis 100 mg/1 ml solution for injection 2. QUALITATIVE AND QUANTITATIVE COMPOSITION 1 ml of Synagis solution contains 100 mg of palivizumab*. Each 0.5 ml vial contains 50 mg of palivizumab. Each 1 ml vial contains 100 mg of palivizumab. *Palivizumab is a recombinant humanised monoclonal antibody produced by DNA technology in mouse myeloma host cells. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection. The solution is clear or slightly opalescent. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Synagis is indicated for the prevention of serious lower respiratory tract disease requiring hospitalisation caused by respiratory syncytial virus (RSV) in children at high risk for RSV disease: Children born at 35 weeks of gestation or less and less than 6 months of age at the onset of the RSV season. Children less than 2 years of age and requiring treatment for bronchopulmonary dysplasia within the last 6 months. Children less than 2 years of age and with haemodynamically significant congenital heart disease. 4.2 Posology and method of administration Posology The recommended dose of palivizumab is 15 mg/kg of body weight, given once a month during anticipated periods of RSV risk in the community. The volume (expressed in ml) of // Palivizumab // to be administered at one-monthly intervals = [patient weight in kg] multiplied by 0.15. Where possible, the first dose should be administered prior to commencement of the RSV season. -

Medicines/Pharmaceuticals of Animal Origin V3.0 November 2020
Medicines/pharmaceuticals of animal origin V3.0 November 2020 Medicines/pharmaceuticals of animal origin - This guideline provides information for all clinical staff within Hospital and Health Services (HHS) on best practice for avoidance of issues related to animal products. Medicines/pharmaceuticals of animal origin - V3.0 November 2020 Published by the State of Queensland (Queensland Health), November 2020 This document is licensed under a Creative Commons Attribution 3.0 Australia licence. To view a copy of this licence, visit creativecommons.org/licenses/by/3.0/au © State of Queensland (Queensland Health) 2020 You are free to copy, communicate and adapt the work, as long as you attribute the State of Queensland (Queensland Health). For more information contact: Medication Services Queensland, Queensland Health, GPO Box 48, Brisbane QLD 4001, email [email protected] An electronic version of this document is available at https://www.health.qld.gov.au/__data/assets/pdf_file/0024/147507/qh-gdl-954.pdf Disclaimer: The content presented in this publication is distributed by the Queensland Government as an information source only. The State of Queensland makes no statements, representations or warranties about the accuracy, completeness or reliability of any information contained in this publication. The State of Queensland disclaims all responsibility and all liability (including without limitation for liability in negligence) for all expenses, losses, damages and costs you might incur as a result of the information being inaccurate -
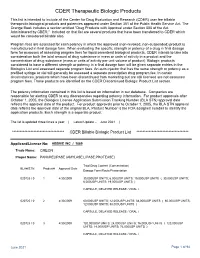
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database. -

Structural Basis for Nonneutralizing Antibody Competition at Antigenic
Structural basis for nonneutralizing antibody PNAS PLUS competition at antigenic site II of the respiratory syncytial virus fusion protein Jarrod J. Mousaa, Marion F. Sauerb, Alexander M. Sevyb, Jessica A. Finnc, John T. Batesa, Gabriela Alvaradoc, Hannah G. Kinga, Leah B. Loerinca, Rachel H. Fongd, Benjamin J. Doranzd, Bruno E. Correiae, Oleksandr Kalyuzhniye, Xiaolin Wenf, Theodore S. Jardetzkyf, William R. Schiefe, Melanie D. Ohig, Jens Meilerh, and James E. Crowe Jr.a,c,i,1 aVanderbilt Vaccine Center, Vanderbilt University Medical Center, Nashville, TN 37232; bChemical and Physical Biology Program, Vanderbilt University Medical Center, Nashville, TN 37232; cDepartment of Pathology, Microbiology, and Immunology, Vanderbilt University, Nashville, TN 37232; dIntegral Molecular, Inc., Philadelphia, PA 19104; eDepartment of Immunology and Microbial Science, The Scripps Research Institute, La Jolla, CA 92037; fDepartment of Structural Biology, Stanford University School of Medicine, Stanford, CA 94305; gDepartment of Cell and Developmental Biology, Vanderbilt University Medical Center, Nashville, TN 37232; hDepartment of Chemistry, Vanderbilt University, Nashville, TN 37232; and iDepartment of Pediatrics, Vanderbilt University School of Medicine, Nashville, TN 37232 Edited by Rino Rappuoli, GSK Vaccines, Siena, Italy, and approved September 20, 2016 (received for review June 10, 2016) Palivizumab was the first antiviral monoclonal antibody (mAb) rearrangement, resulting in fusion of the viral and cell mem- approved for therapeutic use in -

Motavizumab for Prophylaxis of Respiratory Syncytial Virus in High-Risk Children: a Noninferiority Trial
ARTICLES Motavizumab for Prophylaxis of Respiratory Syncytial Virus in High-Risk Children: A Noninferiority Trial AUTHORS: Xavier Carbonell-Estrany, MD, PhD,a Eric A. F. WHAT’S KNOWN ON THIS SUBJECT: Monthly prophylaxis with Simo˜es, MD, MB, BS, DCH,b,c Ron Dagan, MD,d Caroline B. palivizumab has been shown to reduce RSV hospitalizations by Hall, MD,e Brian Harris, MS,f Micki Hultquist, MS,f Edward ϳ50% overall compared with placebo in children at high risk for f f M. Connor, MD, and Genevieve A. Losonsky, MD, for the severe RSV disease. Motavizumab, a monoclonal antibody Motavizumab Study Group developed from palivizumab, has enhanced preclinical activity aNeonatology Service, Hospital Clínic, Agrupacio´Sanite`ria Clínic, against RSV. Hospital de Sant Joan de De´u, Barcelona, Spain; bDepartment of Pediatrics, University of Colorado School of Medicine, Denver, Colorado; cDivision of Infectious Diseases, Children’s Hospital, WHAT THIS STUDY ADDS: Motavizumab may offer an improved Denver, Colorado; dPediatric Infectious Disease Unit, Soroka alternative in prophylaxis for serious RSV disease in children at University Medical Center and Faculty of Health Sciences, Ben- high risk. Motavizumab was noninferior to palivizumab for Gurion University, Beer-Sheva, Israel; eDepartments of Pediatrics prevention of RSV hospitalization (primary end point) and and Medicine, University of Rochester Medical Center, superior to palivizumab for reduction of RSV-specific outpatient Rochester, New York; and fMedImmune, Gaithersburg, Maryland MALRI (a secondary end point). KEY WORDS clinical trial, motavizumab, palivizumab, pediatric, respiratory infection, respiratory syncytial virus ABBREVIATIONS RSV—respiratory syncytial virus CLD—chronic lung disease of prematurity abstract MALRI—medically attended lower respiratory tract infection OBJECTIVE: Palivizumab reduces respiratory syncytial virus (RSV) hospi- OM—otitis media ϳ AE—adverse event talization in children at high risk by 50% compared with placebo. -

(INN) for Biological and Biotechnological Substances
INN Working Document 05.179 Update 2013 International Nonproprietary Names (INN) for biological and biotechnological substances (a review) INN Working Document 05.179 Distr.: GENERAL ENGLISH ONLY 2013 International Nonproprietary Names (INN) for biological and biotechnological substances (a review) International Nonproprietary Names (INN) Programme Technologies Standards and Norms (TSN) Regulation of Medicines and other Health Technologies (RHT) Essential Medicines and Health Products (EMP) International Nonproprietary Names (INN) for biological and biotechnological substances (a review) © World Health Organization 2013 All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int ) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected] ). Requests for permission to reproduce or translate WHO publications – whether for sale or for non-commercial distribution – should be addressed to WHO Press through the WHO web site (http://www.who.int/about/licensing/copyright_form/en/index.html ). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

Neutralizing Antibodies: the Elite Squad to Combat SARS-Cov-2
November 20, 2020 Health & Physiology Neutralizing antibodies: the Elite Squad to combat SARS-CoV-2 infection 1 1 1 by Guanqiao Li | Research Associate; Yang Liu | Research Associate; Linqi Zhang | Professor 1: Center for Global Health and Infectious Diseases, School of Medicine and Vanke School of Public Health, Tsinghua University, Beijing, China This Break was edited by Max Caine, Editor-in-chief - TheScienceBreaker The coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS -CoV-2) urgently calls for prevention and treatment interventions. Neutralizing antibodies isolated from recovered patients are capable of blocking the virus from entry into human cells, potentially acting as the “Elite Squad” to defeat SARS-CoV-2. Image credits: Alissa Eckert, MS; Dan Higgins, MAMS The rapid global transmission of SARS-CoV-2 poses a entering the cells. These antibodies are therefore severe health emergency affecting over 20 million called "neutralizing antibodies". Neutralizing people worldwide as of 12 August. The research antibodies hold a great promise for clinical communities have taken immediate and enormous intervention. A substantial number of investigational actions in search of therapeutic and prophylactic neutralizing antibodies are under development for interventions. The major strategies undertaken diverse infectious diseases. Notably, three have include repurposing “old” drugs, identifying "new" received approval to prevent respiratory syncytial drugs, and taking advantage of neutralizing virus (palivizumab) and prevent and treat anthrax antibodies produced in the plasma of survivors. (raxibacumab and obiltoxaximab). Ultimately, developing vaccines that provide sufficient and long protection against infection and Since the outbreak of COVID-19, we have been diseases. -

List Item Synagis-H-C-257-P46-0036 : EPAR
21 November 2013 EMA/CHMP/780068/2013 Committee for Medicinal Products for Human Use (CHMP) Synagis (Palivizumab) Procedure no. EMA/H/C/000257/P46/036 CHMP assessment report for paediatric use studies submitted according to Article 46 of the Regulation (EC) No 1901/2006 Assessment Report as adopted by the CHMP with all information of a commercially confidential nature deleted 7 Westferry Circus ● Canary Wharf ● London E14 4HB ● United Kingdom Telephone +44 (0)20 7418 8400 Facsimile +44 (0)20 7 E -mail [email protected] Website www.ema.europa.eu An agency of the European Union © European Medicines Agency, 2014. Reproduction is authorised provided the source is acknowledged. Introduction On July 30, 2013, the MAH submitted seven completed paediatric studies for palivizumab, in accordance with Article 46 of Regulation (EC) No1901/2006, as amended. A short critical expert overview for each study has also been provided. The MAH states that four of the submitted paediatric studies (M12-420, W10-664, MI-CP118, MI- CP127) do not influence the benefit risk for palivizumab and that no consequential regulatory action is required. Studies MI-CP116, MI-CP110 and MI-CP124 will be submitted as supportive clinical experience in an extension application consisting of the full relevant data package to register the solution for injection formulation in the EU; expected to be submitted by October 2013. Scientific discussion Information on the development program The MAH stated that: Study M12-420, Multi-center, Open-label, Uncontrolled Clinical Study of -
Michigan Care Improvement Registry HL7 2.5.1 Specification Guide for Query by Parameter (QBP)
Michigan Care Improvement Registry HL7 2.5.1 Specification Guide for Query by Parameter (QBP) Version 1.5 JUNE 7, 2016 Document Description This guide is intended for immunization providers and their vendors to assist in connecting to the Michigan Care Improvement Registry (MCIR). MCIR is an immunization registry that compiles complete immunization histories for children and adults in Michigan. This document explains the technical details of how to Query MCIR for a patient records and receive the immunization history and forecast for next dose due for that patient. Message types supported: QBP Z44^CDC RSP Z42^CDC ACK Message formats supported: HL7 2.5.1 version 1.5 Revision history Revision Date Author Release 1.0 August 1, 2013 Therese Hoyle Release 1.1 January 7,2014 Therese Hoyle Release 1.5 June 7, 2016 Sallie Sims A list of changes may be found at the end of Implementation Guide 1 Michigan Care Improvement Registry Introduction and History MCIR was created in 1998 to collect reliable immunization information and make it accessible to authorized users online. In 2006, MCIR was expanded to include adults. By state law, providers are required to submit childhood immunizations within 72 hours of administration. In addition, providers are allowed and highly encouraged to report adult vaccinations. MCIR benefits health care organizations, schools, licensed childcare programs, and Michigan’s citizens by consolidating immunization information from multiple providers. This reduces vaccine-preventable diseases, over-vaccination, and allows providers to see up-to-date patient immunization history. MCIR also has the ability to assist with pandemic flu preparedness and can track vaccines and medications during a public health emergency.