Physical Activity, a Modulator of Aging Through Effects on Telomere Biology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HOLOHAN-DISSERTATION-2015.Pdf (6.419Mb)
IDENTIFYING, CHARACTERIZING AND INHIBITING THE TELOMERASE REGULATORY NETWORK APPROVED BY SUPERVISORY COMMITTEE Jerry Shay, PhD Woodring Wright, MD, PhD David Corey, PhD Rolf Brekken, PhD Melanie Cobb, PhD DEDICATION Dedicated to my parents, Mark and Tracy Holohan, as well as my siblings, Kelly Nudleman and Kyle Holohan for their support and encouragement. IDENTIFYING, CHARACTERIZING AND INHIBITING THE TELOMERASE REGULATORY NETWORK by BRODY CHRISTOPHER HOLOHAN DISSERTATION / THESIS Presented to the Faculty of the Graduate School of Biomedical Sciences The University of Texas Southwestern Medical Center at Dallas In Partial Fulfillment of the Requirements For the Degree of DOCTOR OF PHILOSOPHY The University of Texas Southwestern Medical Center at Dallas Dallas, Texas May, 2015 Copyright by Brody Christopher Holohan, 2015 All Rights Reserved ACKNOWLEDGEMENTS I would like the thank my mentors, Jerry Shay and Woodring Wright for their continuous support, advice and encouragement, as well as allowing me time and resources to pursue my ideas. They are a fantastic team, and I could not have asked for better mentors. I would also like to thank my lab-mates, particularly Dr. Andrew Ludlow, Dr. Yong Zhou, Dr. Tsung-Po Lai, Dr. Oliver Delgado, Dr. Wanil Kim, Dr. Guido Stadler, Kimberly Batten, Ryan Laranger and Neal Jones. I would also like to thank Kevin Kennon for administrative support. Without my collaborators much of this would have been impossible, so I would like to thank Dr. Tim De Meyer, Dr. Abraham Aviv, Dr. Fowzan Aklayura, Dr. Steve Hunt, Dr. Tim Spector, Dr. Massimo Mangino, Dr. Daphne Friedman and Dr. Daniel Eisenberg for their help, intellectual discussions and willingness to pursue challenenging ideas. -
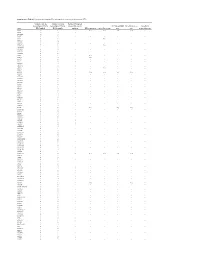
Supplementary Table S1. Prioritization of Candidate FPC Susceptibility Genes by Private Heterozygous Ptvs
Supplementary Table S1. Prioritization of candidate FPC susceptibility genes by private heterozygous PTVs Number of private Number of private Number FPC patient heterozygous PTVs in heterozygous PTVs in tumors with somatic FPC susceptibility Hereditary cancer Hereditary Gene FPC kindred BCCS samples mutation DNA repair gene Cancer driver gene gene gene pancreatitis gene ATM 19 1 - Yes Yes Yes Yes - SSPO 12 8 1 - - - - - DNAH14 10 3 - - - - - - CD36 9 3 - - - - - - TET2 9 1 - - Yes - - - MUC16 8 14 - - - - - - DNHD1 7 4 1 - - - - - DNMT3A 7 1 - - Yes - - - PKHD1L1 7 9 - - - - - - DNAH3 6 5 - - - - - - MYH7B 6 1 - - - - - - PKD1L2 6 6 - - - - - - POLN 6 2 - Yes - - - - POLQ 6 7 - Yes - - - - RP1L1 6 6 - - - - - - TTN 6 5 4 - - - - - WDR87 6 7 - - - - - - ABCA13 5 3 1 - - - - - ASXL1 5 1 - - Yes - - - BBS10 5 0 - - - - - - BRCA2 5 6 1 Yes Yes Yes Yes - CENPJ 5 1 - - - - - - CEP290 5 5 - - - - - - CYP3A5 5 2 - - - - - - DNAH12 5 6 - - - - - - DNAH6 5 1 1 - - - - - EPPK1 5 4 - - - - - - ESYT3 5 1 - - - - - - FRAS1 5 4 - - - - - - HGC6.3 5 0 - - - - - - IGFN1 5 5 - - - - - - KCP 5 4 - - - - - - LRRC43 5 0 - - - - - - MCTP2 5 1 - - - - - - MPO 5 1 - - - - - - MUC4 5 5 - - - - - - OBSCN 5 8 2 - - - - - PALB2 5 0 - Yes - Yes Yes - SLCO1B3 5 2 - - - - - - SYT15 5 3 - - - - - - XIRP2 5 3 1 - - - - - ZNF266 5 2 - - - - - - ZNF530 5 1 - - - - - - ACACB 4 1 1 - - - - - ALS2CL 4 2 - - - - - - AMER3 4 0 2 - - - - - ANKRD35 4 4 - - - - - - ATP10B 4 1 - - - - - - ATP8B3 4 6 - - - - - - C10orf95 4 0 - - - - - - C2orf88 4 0 - - - - - - C5orf42 4 2 - - - - -

Telomeres, Aging and Exercise: Guilty by Association?
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Federation ResearchOnline COPYRIGHT NOTICE FedUni ResearchOnline https://researchonline.federation.edu.au This is the published version of: Chilton, W., et.al. (2017) Telomeres, aging and exercise: Guilty by association. International Journal of Molecular Sciences, 18(12), p.1-32. Available online at https://doi.org/10.3390/ijms18122573 Copyright © 2017 Chilton, W., et.al. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0) (http://creativecommons.org/licenses/by/4.0/). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. International Journal of Molecular Sciences Review Telomeres, Aging and Exercise: Guilty by Association? Warrick Chilton 1,*, Brendan O’Brien 1 and Fadi Charchar 1,2,3,* ID 1 Faculty of Health Sciences and Faculty of Science and Technology, Federation University Australia, Ballarat, VIC 3350, Australia; [email protected] 2 Department of Physiology, University of Melbourne, Melbourne, VIC 3010, Australia 3 Department of Cardiovascular Sciences, University of Leicester, Leicester LE1 7RH, UK * Correspondence: [email protected] (W.C.); [email protected] (F.C.); Tel.: +61-3-5327-6254 (W.C.); +61-3-5327-6098 (F.C.) Received: 7 September 2017; Accepted: 25 November 2017; Published: 29 November 2017 Abstract: Telomeres are repetitive tandem DNA sequences that cap chromosomal ends protecting genomic DNA from enzymatic degradation. -

Localization of Glucokinase Gene Expression in the Rat Brain Ronald M
Localization of Glucokinase Gene Expression in the Rat Brain Ronald M. Lynch, Linda S. Tompkins, Heddwen L. Brooks, Ambrose A. Dunn-Meynell, and Barry E. Levin The brain contains a subpopulation of glucosensing neu- rons that alter their firing rate in response to elevated glucose concentrations. In pancreatic -cells, gluco- ammalian feeding behavior and general energy kinase (GK), the rate-limiting enzyme in glycolysis, medi- homeostasis appear to be regulated by circu- ates glucose-induced insulin release by regulating intra- lating levels of nutrients (glucose) and pep- cellular ATP production. A similar role for GK is pro- tides (e.g., leptin, insulin). Sensors to detect lev- posed to underlie neuronal glucosensing. Via in situ M els of these factors have been found to reside within specific hybridization, GK mRNA was localized to hypothalamic areas that are thought to contain relatively large popu- nuclei of the hypothalamus (1–8), where central regulation of lations of glucosensing neurons (the arcuate, ventrome- energy homeostasis is believed to be coordinated. For exam- dial, dorsomedial, and paraventricular nuclei and the lat- ple, large changes in blood glucose are correlated with cen- eral area). GK also was found in brain areas without trally mediated responses such as thermogenesis through known glucosensing neurons (the lateral habenula, the activation of the sympathetic nervous system. These changes bed nucleus stria terminalis, the inferior olive, the are monitored by the brain (9–11), and such responses are retrochiasmatic and medial preoptic areas, and the thal- altered in obesity-prone animals (11–13). Moreover, lesions amic posterior paraventricular, interpeduncular, oculo- of the ventromedial hypothalamus (VMH) prevent the hypo- motor, and anterior olfactory nuclei). -

A Specific N-Terminal Extension of the 8 Kda Domain Is Required for DNA End-Bridging by Human Polk and Polj
Published online 8 August 2013 Nucleic Acids Research, 2013, Vol. 41, No. 19 9105–9116 doi:10.1093/nar/gkt681 A specific N-terminal extension of the 8 kDa domain is required for DNA end-bridging by human Polk and Polj Maria Jose Martin*, Maria Victoria Garcia-Ortiz, Ana Gomez-Bedoya, Veronica Esteban, Susana Guerra and Luis Blanco* Centro de Biologia Molecular Severo Ochoa (CSIC-UAM), 28049 Madrid, Spain Received February 27, 2013; Revised July 12, 2013; Accepted July 14, 2013 ABSTRACT state [see Supplementary Figure S1A for an example with Polß; reviewed in (1)]. One role of this conformational Human DNA polymerases mu (Polk) and lambda change is to allow the rapid binding of substrates (and (Polj) are X family members involved in the repair release of products) in the open state, while inducing of double-strand breaks in DNA during non-homolo- optimal alignment of catalytic residues surrounding the gous end joining. Crucial abilities of these enzymes substrates in the closed state. The shape of the base pair include bridging of the two 30 single-stranded over- formed determines the fate of the weakly bound nucleotide hangs and trans-polymerization using one 30 end as during the conformational change step: only a correct base primer and the other as template, to minimize pair induces closing of the enzyme to form a tight catalytic sequence loss. In this context, we have studied complex; conversely, if a mismatched nucleotide is bound, the importance of a previously uncharacterised the enzyme does not close, but rather proceeds to release sequence (‘brooch’), located at the N-terminal the nucleotide while reducing the rate of catalysis. -

Involvement of DNA Polymerase K in the Repair of a Specific Subset of DNA Double-Strand Breaks in Mammalian Cells
Published online 5 May 2007 Nucleic Acids Research, 2007, Vol. 35, No. 11 3551–3560 doi:10.1093/nar/gkm243 Involvement of DNA polymerase k in the repair of a specific subset of DNA double-strand breaks in mammalian cells Jean-Pascal Capp1, Franc¸ ois Boudsocq1, Anne-Gaelle Besnard1, Bernard S. Lopez2, Christophe Cazaux1, Jean-Se´ bastien Hoffmann1 and Yvan Canitrot1,* 1Genetic instability and Cancer group, Institute of Pharmacology and Structural Biology, University Paul Sabatier, UMR CNRS 5089, 205 route de Narbonne, 31077 Toulouse cedex and 2De´ partement de Radiobiologie et Radiopathologie, 60-68 av. Ge´ ne´ ral Leclerc, UMR 217 CNRS-CEA, 92265 Fontenay aux Roses cedex, France Received February 27, 2007; Revised April 2, 2007; Accepted April 3, 2007 ABSTRACT the recently discovered DNA polymerase l (poll) (2,3). Polm and poll share some homology and both have been The repair of DNA double-strand breaks (DSB) described as participating in vitro in the repair of DNA requires processing of the broken ends to complete double-strand breaks (DSB) by non-homologous end the ligation process. Recently, it has been shown joining (NHEJ) (4,5). The hallmark of animals or cells that DNA polymerase k (polk) and DNA polymerase j defective in one of the components of the NHEJ pathway (polj) are both involved in such processing during is an increased sensitivity to ionizing radiation (IR) (6–8). non-homologous end joining in vitro. However, no However, cells isolated from animals knocked out for poll phenotype was observed in animal models defective or polm do not present differences in sensitivity to any for either polk and/or polj. -

The Diagnostic Potential of Dielectric Properties, Telomerase Activity and Cytokeratin 20 in Urine Cells of Bladder Cancer Patients Fakhry F
cer Scien an ce C & f o T h Ibrahim and Ghannam, J Cancer Sci Ther 2012, 4.8 l a e n r a Journal of r 1000148 p u DOI: 10.4172/1948-5956. y o J ISSN: 1948-5956 Cancer Science & Therapy Research Article Open Access The Diagnostic Potential of Dielectric Properties, Telomerase Activity and Cytokeratin 20 in Urine Cells of Bladder Cancer Patients Fakhry F. Ibrahim1,3 and Magdy M. Ghannam2,4* 1Department of Physics, College of Science, Shaqra University, Saudi Arabia 2Department of Physics and Astronomy, College of Science, King Saud University, Saudi Arabia 3Clinical Pathology Department, Cairo University Hospital, Cairo University, Egypt 4Department of Biophysics, Faculty of Science, Cairo University, Egypt Abstract Aim of the study: This work aims to search for mark ers suitable for the screening of bladder cancer, which should be specific, sensitive, reproducible, non-invasive and at acceptable cost. Patients and methods: The study included 45 patients diagnosed as bladder cancer (30 TCC, 15 SCC) of different stages and grades, 20 patients with various urothelial diseases, besides 15 healthy volunteers of matched age and sex to the malignant group. A random midstream urine sample was collected in a sterile container for the determination of telomerase by RT-PCR, keratin 20 by RT-PCR and immunohistochemical staining, urine cytology in addition to DNA dielectric properties. Results: All parameters (telomerase, K20, cytology and DNA dielectric properties) for the malignant group showed significant difference from both the benign and the control groups. With respect to the grade, only K20 showed a significant positive correlation with grade in both TCC and SCC. -

The Genetic Program of Pancreatic Beta-Cell Replication in Vivo
Page 1 of 65 Diabetes The genetic program of pancreatic beta-cell replication in vivo Agnes Klochendler1, Inbal Caspi2, Noa Corem1, Maya Moran3, Oriel Friedlich1, Sharona Elgavish4, Yuval Nevo4, Aharon Helman1, Benjamin Glaser5, Amir Eden3, Shalev Itzkovitz2, Yuval Dor1,* 1Department of Developmental Biology and Cancer Research, The Institute for Medical Research Israel-Canada, The Hebrew University-Hadassah Medical School, Jerusalem 91120, Israel 2Department of Molecular Cell Biology, Weizmann Institute of Science, Rehovot, Israel. 3Department of Cell and Developmental Biology, The Silberman Institute of Life Sciences, The Hebrew University of Jerusalem, Jerusalem 91904, Israel 4Info-CORE, Bioinformatics Unit of the I-CORE Computation Center, The Hebrew University and Hadassah, The Institute for Medical Research Israel- Canada, The Hebrew University-Hadassah Medical School, Jerusalem 91120, Israel 5Endocrinology and Metabolism Service, Department of Internal Medicine, Hadassah-Hebrew University Medical Center, Jerusalem 91120, Israel *Correspondence: [email protected] Running title: The genetic program of pancreatic β-cell replication 1 Diabetes Publish Ahead of Print, published online March 18, 2016 Diabetes Page 2 of 65 Abstract The molecular program underlying infrequent replication of pancreatic beta- cells remains largely inaccessible. Using transgenic mice expressing GFP in cycling cells we sorted live, replicating beta-cells and determined their transcriptome. Replicating beta-cells upregulate hundreds of proliferation- related genes, along with many novel putative cell cycle components. Strikingly, genes involved in beta-cell functions, namely glucose sensing and insulin secretion were repressed. Further studies using single molecule RNA in situ hybridization revealed that in fact, replicating beta-cells double the amount of RNA for most genes, but this upregulation excludes genes involved in beta-cell function. -

1 Novel Expression Signatures Identified by Transcriptional Analysis
ARD Online First, published on October 7, 2009 as 10.1136/ard.2009.108043 Ann Rheum Dis: first published as 10.1136/ard.2009.108043 on 7 October 2009. Downloaded from Novel expression signatures identified by transcriptional analysis of separated leukocyte subsets in SLE and vasculitis 1Paul A Lyons, 1Eoin F McKinney, 1Tim F Rayner, 1Alexander Hatton, 1Hayley B Woffendin, 1Maria Koukoulaki, 2Thomas C Freeman, 1David RW Jayne, 1Afzal N Chaudhry, and 1Kenneth GC Smith. 1Cambridge Institute for Medical Research and Department of Medicine, Addenbrooke’s Hospital, Hills Road, Cambridge, CB2 0XY, UK 2Roslin Institute, University of Edinburgh, Roslin, Midlothian, EH25 9PS, UK Correspondence should be addressed to Dr Paul Lyons or Prof Kenneth Smith, Department of Medicine, Cambridge Institute for Medical Research, Addenbrooke’s Hospital, Hills Road, Cambridge, CB2 0XY, UK. Telephone: +44 1223 762642, Fax: +44 1223 762640, E-mail: [email protected] or [email protected] Key words: Gene expression, autoimmune disease, SLE, vasculitis Word count: 2,906 The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non-exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd and its Licensees to permit this article (if accepted) to be published in Annals of the Rheumatic Diseases and any other BMJPGL products to exploit all subsidiary rights, as set out in their licence (http://ard.bmj.com/ifora/licence.pdf). http://ard.bmj.com/ on September 29, 2021 by guest. Protected copyright. 1 Copyright Article author (or their employer) 2009. -
Gain-Of-Function and Dominant-Negative Effects of Distinct P53 Mutations in Lung Tumours
Gain-of-function and dominant-negative effects of distinct p53 mutations in lung tumours Frances Kathryn Turrell Clare College, University of Cambridge This dissertation is submitted for the degree of Doctor of Philosophy December 2017 2 Gain-of-function and dominant-negative effects of distinct p53 mutations in lung tumours Frances Kathryn Turrell Lung cancer is the most common cause of cancer-related mortality worldwide with current treatments providing limited therapeutic benefit in most cases. TP53 (Trp53, p53) mutations occur in approximately 50% of lung adenocarcinoma cases and are associated with poor prognosis and so novel therapies that target these p53 mutant lung tumours are urgently needed. Despite the high frequency of p53 mutations in lung tumours, the impact these mutations have on response to therapy remains unclear in this cancer type. The aim of my project is to characterise the gain-of-function and dominant- negative effects of p53 mutations in lung tumours and to identify ways of therapeutically targeting these p53 mutant tumours based on dependencies and susceptibilities that our analysis uncovers. To characterise the gain-of-function and dominant-negative effects of p53 mutations I compared p53 mutant murine lung tumour cells that endogenously express either a contact (R270H, equivalent to R273H in humans) or conformational (R172H, equivalent to R175H in humans) p53 mutant protein and p53 null lung tumour cell lines; both in the presence and absence of wild-type p53. Interestingly, transcriptional and functional analysis uncovered metabolic gain-of-functions that are specific to the type of p53 mutation. Upregulation of mevalonate pathway expression was observed only in R270H lung tumours and consequently R172H and R270H lung tumours displayed distinct sensitivities to simvastatin, a mevalonate pathway inhibitor widely used in the clinic. -

Differential Mechanisms of Tolerance to Extreme Environmental
www.nature.com/scientificreports OPEN Diferential mechanisms of tolerance to extreme environmental conditions in tardigrades Dido Carrero*, José G. Pérez-Silva , Víctor Quesada & Carlos López-Otín * Tardigrades, also known as water bears, are small aquatic animals that inhabit marine, fresh water or limno-terrestrial environments. While all tardigrades require surrounding water to grow and reproduce, species living in limno-terrestrial environments (e.g. Ramazzottius varieornatus) are able to undergo almost complete dehydration by entering an arrested state known as anhydrobiosis, which allows them to tolerate ionic radiation, extreme temperatures and intense pressure. Previous studies based on comparison of the genomes of R. varieornatus and Hypsibius dujardini - a less tolerant tardigrade - have pointed to potential mechanisms that may partially contribute to their remarkable ability to resist extreme physical conditions. In this work, we have further annotated the genomes of both tardigrades using a guided approach in search for novel mechanisms underlying the extremotolerance of R. varieornatus. We have found specifc amplifcations of several genes, including MRE11 and XPC, and numerous missense variants exclusive of R. varieornatus in CHEK1, POLK, UNG and TERT, all of them involved in important pathways for DNA repair and telomere maintenance. Taken collectively, these results point to genomic features that may contribute to the enhanced ability to resist extreme environmental conditions shown by R. varieornatus. Tardigrades are small -

Gene Expression Profiles of Vesicant-Induced Skin Injury
Gene Expression Profiles of Vesicant-Induced Skin Injury D.R. Gerecke1, C.L.K. Sabourin2, Y.C. Chang1, J.D. Laskin1, M.K. Gordon1, and R.P. Casillas2 1CounterAct Research Center of Excellence UMDNJ/Robert Wood Johnson Medical School and Rutgers University EOHSI, Piscataway, NJ, USA 2Battelle Biomedical Research Center, Columbus, Ohio Department of Pharmacology & Toxicology, Rutgers University EOHSI Building, 170 Frelinghuysen Road Piscataway, New Jersey 08854, USA [email protected] ABSTRACT Cutaneous exposure to sulfur mustard [bis-(2-chloroethyl)-sulfide; SM, HD] results in characteristic blister formation in the exposed skin. The blister is not immediate, but develops within the first 24 hours after SM exposure. During this period there is a marked inflammatory response that involves a variety of cell types including neutrophils, macrophages, T-cells, B-cells, and fibroblasts. Skin from mice exposed to a high level (0.08 mg) of SM was collected at early (6, 12, and 24 h post exposure) or late (72 and 168 h post exposure) time intervals, the RNA isolated, and analyzed for gene expression analysis by the Affymetrix Murine high- density oligonucleotide array (46K genes and ESTs). Expression of more than 1000 independent mRNAs was upregulated greater than 2-fold in a minimum of one of the five timepoints in SM-exposed skin. Data was organized into four major groups based on cluster analysis: 1) those mRNAs with a 2-fold increase beginning within 24 h and persisting throughout the study; 2) those mRNAs with a 2-fold increase within 24 h that became down-regulated in at least one of the later timepoints; 3) those mRNAs with a 2-fold increase starting at 72 h; 4) those mRNAs with a 2-fold increase starting at 168 hr.