Gain-Of-Function and Dominant-Negative Effects of Distinct P53 Mutations in Lung Tumours
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

EGFR and Mtor As Therapeutic Targets in Glioblastoma
www.oncotarget.com Oncotarget, 2019, Vol. 10, (No. 46), pp: 4721-4723 Editorial EGFR and mTOR as therapeutic targets in glioblastoma Michael W. Ronellenfitsch, Anna-Luisa Luger and Joachim P. Steinbach The quest for new and improved therapies for mammalian target of rapamycin complex 1 (mTORC1) glioblastoma (GB) has been mostly unsuccessful in signaling were found in the majority of GBs [3]. more than a decade despite significant efforts. The few Therefore, many hopes have rested on targeted therapies. exceptions include the optimization of classical alkylating However, the results from clinical trials have been largely chemotherapy by including lomustine in the first line disappointing [4]. Nevertheless, unplanned retrospective regimen for GB with a methylated MGMT promoter and subgroup analyses of the patient cohorts of negative tumor treating fields [1, 2]. The GB signaling network has clinical trials indicated that dysregulation or activation been well-characterized and genetic alterations resulting of signaling could be a predictive factor for susceptibility in activation of receptor tyrosine kinases and especially to pathway inhibition: Tumors with enhanced levels of epidermal growth factor receptor (EGFR) and downstream mTORC1 activation markers, including phosphorylated Figure 1: Scheme of EGFR signaling and DDIT4-mediated adaptive processes. Conditions of the glioblastoma microenvironment including hypoxia, alkylating therapy or irradiation trigger induction of DDIT4 which activates TSC1/2 to inhibit mTORC1 and can counteract epidermal growth factor receptor (EGFR)-mediated TSC1/2 inhibition. Inhibition of mTORC1 ultimately induces adaptive processes to cope with external stressors. www.oncotarget.com 4721 Oncotarget ribosomal protein S6 and phosphorylated mTOR itself, of effects. Depending on the half life and pharmacokinetics appeared to respond to pathway inhibition by the EGFR of the drugs, stepwise treatment algorithms could be an antibody nimotuzumab or the mTORC1 inhibitor option to prevent antagonistic effects. -

HOLOHAN-DISSERTATION-2015.Pdf (6.419Mb)
IDENTIFYING, CHARACTERIZING AND INHIBITING THE TELOMERASE REGULATORY NETWORK APPROVED BY SUPERVISORY COMMITTEE Jerry Shay, PhD Woodring Wright, MD, PhD David Corey, PhD Rolf Brekken, PhD Melanie Cobb, PhD DEDICATION Dedicated to my parents, Mark and Tracy Holohan, as well as my siblings, Kelly Nudleman and Kyle Holohan for their support and encouragement. IDENTIFYING, CHARACTERIZING AND INHIBITING THE TELOMERASE REGULATORY NETWORK by BRODY CHRISTOPHER HOLOHAN DISSERTATION / THESIS Presented to the Faculty of the Graduate School of Biomedical Sciences The University of Texas Southwestern Medical Center at Dallas In Partial Fulfillment of the Requirements For the Degree of DOCTOR OF PHILOSOPHY The University of Texas Southwestern Medical Center at Dallas Dallas, Texas May, 2015 Copyright by Brody Christopher Holohan, 2015 All Rights Reserved ACKNOWLEDGEMENTS I would like the thank my mentors, Jerry Shay and Woodring Wright for their continuous support, advice and encouragement, as well as allowing me time and resources to pursue my ideas. They are a fantastic team, and I could not have asked for better mentors. I would also like to thank my lab-mates, particularly Dr. Andrew Ludlow, Dr. Yong Zhou, Dr. Tsung-Po Lai, Dr. Oliver Delgado, Dr. Wanil Kim, Dr. Guido Stadler, Kimberly Batten, Ryan Laranger and Neal Jones. I would also like to thank Kevin Kennon for administrative support. Without my collaborators much of this would have been impossible, so I would like to thank Dr. Tim De Meyer, Dr. Abraham Aviv, Dr. Fowzan Aklayura, Dr. Steve Hunt, Dr. Tim Spector, Dr. Massimo Mangino, Dr. Daphne Friedman and Dr. Daniel Eisenberg for their help, intellectual discussions and willingness to pursue challenenging ideas. -

Effects of Rapamycin on Social Interaction Deficits and Gene
Kotajima-Murakami et al. Molecular Brain (2019) 12:3 https://doi.org/10.1186/s13041-018-0423-2 RESEARCH Open Access Effects of rapamycin on social interaction deficits and gene expression in mice exposed to valproic acid in utero Hiroko Kotajima-Murakami1,2, Toshiyuki Kobayashi3, Hirofumi Kashii1,4, Atsushi Sato1,5, Yoko Hagino1, Miho Tanaka1,6, Yasumasa Nishito7, Yukio Takamatsu7, Shigeo Uchino1,2 and Kazutaka Ikeda1* Abstract The mammalian target of rapamycin (mTOR) signaling pathway plays a crucial role in cell metabolism, growth, and proliferation. The overactivation of mTOR has been implicated in the pathogenesis of syndromic autism spectrum disorder (ASD), such as tuberous sclerosis complex (TSC). Treatment with the mTOR inhibitor rapamycin improved social interaction deficits in mouse models of TSC. Prenatal exposure to valproic acid (VPA) increases the incidence of ASD. Rodent pups that are exposed to VPA in utero have been used as an animal model of ASD. Activation of the mTOR signaling pathway was recently observed in rodents that were exposed to VPA in utero, and rapamycin ameliorated social interaction deficits. The present study investigated the effect of rapamycin on social interaction deficits in both adolescence and adulthood, and gene expressions in mice that were exposed to VPA in utero. We subcutaneously injected 600 mg/kg VPA in pregnant mice on gestational day 12.5 and used the pups as a model of ASD. The pups were intraperitoneally injected with rapamycin or an equal volume of vehicle once daily for 2 consecutive days. The social interaction test was conducted in the offspring after the last rapamycin administration at 5–6 weeks of ages (adolescence) or 10–11 weeks of age (adulthood). -
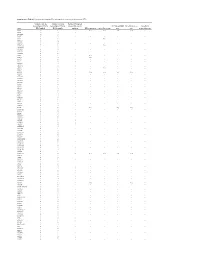
Supplementary Table S1. Prioritization of Candidate FPC Susceptibility Genes by Private Heterozygous Ptvs
Supplementary Table S1. Prioritization of candidate FPC susceptibility genes by private heterozygous PTVs Number of private Number of private Number FPC patient heterozygous PTVs in heterozygous PTVs in tumors with somatic FPC susceptibility Hereditary cancer Hereditary Gene FPC kindred BCCS samples mutation DNA repair gene Cancer driver gene gene gene pancreatitis gene ATM 19 1 - Yes Yes Yes Yes - SSPO 12 8 1 - - - - - DNAH14 10 3 - - - - - - CD36 9 3 - - - - - - TET2 9 1 - - Yes - - - MUC16 8 14 - - - - - - DNHD1 7 4 1 - - - - - DNMT3A 7 1 - - Yes - - - PKHD1L1 7 9 - - - - - - DNAH3 6 5 - - - - - - MYH7B 6 1 - - - - - - PKD1L2 6 6 - - - - - - POLN 6 2 - Yes - - - - POLQ 6 7 - Yes - - - - RP1L1 6 6 - - - - - - TTN 6 5 4 - - - - - WDR87 6 7 - - - - - - ABCA13 5 3 1 - - - - - ASXL1 5 1 - - Yes - - - BBS10 5 0 - - - - - - BRCA2 5 6 1 Yes Yes Yes Yes - CENPJ 5 1 - - - - - - CEP290 5 5 - - - - - - CYP3A5 5 2 - - - - - - DNAH12 5 6 - - - - - - DNAH6 5 1 1 - - - - - EPPK1 5 4 - - - - - - ESYT3 5 1 - - - - - - FRAS1 5 4 - - - - - - HGC6.3 5 0 - - - - - - IGFN1 5 5 - - - - - - KCP 5 4 - - - - - - LRRC43 5 0 - - - - - - MCTP2 5 1 - - - - - - MPO 5 1 - - - - - - MUC4 5 5 - - - - - - OBSCN 5 8 2 - - - - - PALB2 5 0 - Yes - Yes Yes - SLCO1B3 5 2 - - - - - - SYT15 5 3 - - - - - - XIRP2 5 3 1 - - - - - ZNF266 5 2 - - - - - - ZNF530 5 1 - - - - - - ACACB 4 1 1 - - - - - ALS2CL 4 2 - - - - - - AMER3 4 0 2 - - - - - ANKRD35 4 4 - - - - - - ATP10B 4 1 - - - - - - ATP8B3 4 6 - - - - - - C10orf95 4 0 - - - - - - C2orf88 4 0 - - - - - - C5orf42 4 2 - - - - -

Transcriptional Changes in Huntington Disease Identified Using Genome
Human Molecular Genetics, 2010, Vol. 19, No. 8 1438–1452 doi:10.1093/hmg/ddq018 Advance Access published on January 20, 2010 Transcriptional changes in Huntington disease identified using genome-wide expression profiling and cross-platform analysis Kristina Becanovic1, Mahmoud A. Pouladi1, Raymond S. Lim2, Alexandre Kuhn3, Paul Pavlidis2, Ruth Luthi-Carter3, Michael R. Hayden1 and Blair R. Leavitt1,Ã 1Centre for Molecular Medicine and Therapeutics, Child and Family Research Institute, Department of Medical Genetics, University of British Columbia, Vancouver, BC, Canada V5Z 4H4 2Centre for High-throughput Biology and Department of Psychiatry, University of British Columbia, Vancouver, BC, Canada V6T 1Z4 and 3Brain Mind Institute, E´ cole Polytechnique Fe´de´rale de Lausanne (EPFL), Station 15, CH1015 Lausanne, Switzerland Received September 10, 2009; Revised and Accepted January 18, 2010 Evaluation of transcriptional changes in the striatum may be an effective approach to understanding the natural history of changes in expression contributing to the pathogenesis of Huntington disease (HD). We have performed genome-wide expression profiling of the YAC128 transgenic mouse model of HD at 12 and 24 months of age using two platforms in parallel: Affymetrix and Illumina. The data from these two powerful platforms were integrated to create a combined rank list, thereby revealing the identity of additional genes that proved to be differentially expressed between YAC128 and control mice. Using this approach, we ident- ified 13 genes to be differentially expressed between YAC128 and controls which were validated by quanti- tative real-time PCR in independent cohorts of animals. In addition, we analyzed additional time points relevant to disease pathology: 3, 6 and 9 months of age. -

Telomeres, Aging and Exercise: Guilty by Association?
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Federation ResearchOnline COPYRIGHT NOTICE FedUni ResearchOnline https://researchonline.federation.edu.au This is the published version of: Chilton, W., et.al. (2017) Telomeres, aging and exercise: Guilty by association. International Journal of Molecular Sciences, 18(12), p.1-32. Available online at https://doi.org/10.3390/ijms18122573 Copyright © 2017 Chilton, W., et.al. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0) (http://creativecommons.org/licenses/by/4.0/). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. International Journal of Molecular Sciences Review Telomeres, Aging and Exercise: Guilty by Association? Warrick Chilton 1,*, Brendan O’Brien 1 and Fadi Charchar 1,2,3,* ID 1 Faculty of Health Sciences and Faculty of Science and Technology, Federation University Australia, Ballarat, VIC 3350, Australia; [email protected] 2 Department of Physiology, University of Melbourne, Melbourne, VIC 3010, Australia 3 Department of Cardiovascular Sciences, University of Leicester, Leicester LE1 7RH, UK * Correspondence: [email protected] (W.C.); [email protected] (F.C.); Tel.: +61-3-5327-6254 (W.C.); +61-3-5327-6098 (F.C.) Received: 7 September 2017; Accepted: 25 November 2017; Published: 29 November 2017 Abstract: Telomeres are repetitive tandem DNA sequences that cap chromosomal ends protecting genomic DNA from enzymatic degradation. -

An Integrative Transcriptome Study Reveals Ddit4/Redd1 As a Key Regulator of Cancer Cachexia in Rodent Models
www.nature.com/cddis ARTICLE OPEN An integrative transcriptome study reveals Ddit4/Redd1 as a key regulator of cancer cachexia in rodent models 1,2,4 1,2,4 3 1,2 1,2 1,2 2 1,2 Mengyuan Niu ,LiLi , Zhonglan✉ Su , Lulu Wei✉ , Wenyuan Pu , Chen Zhao✉ , Yibing Ding , Junaid Wazir , Wangsen Cao 2, Shiyu Song 1,2 , Qian Gao 2 and Hongwei Wang 1,2 © The Author(s) 2021 Cancer cachexia is a multifactorial metabolic syndrome that causes up to 20% of cancer-related deaths. Muscle atrophy, the hallmark of cancer cachexia, strongly impairs the quality of life of cancer patients; however, the underlying pathological process is still poorly understood. Investigation of the disease pathogenesis largely relies on cachectic mouse models. In our study, the transcriptome of the cachectic gastrocnemius muscle in the C26 xenograft model was integrated and compared with that of 5 more different datasets. The bioinformatic analysis revealed pivotal gene ontology (GO) terms and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathways of the disease, and the key genes were validated. Construction of the protein-protein interaction network and the comparison of pathways enriched in cancer cachexia with 5 other muscle atrophy models revealed Ddit4 (DNA damage-inducible transcript 4), as a key protein in cancer cachexia. The higher expression of Ddit4 in cachectic muscle was further validated in animal models and cachectic cancer patients. Further study revealed that p38 induced the expression of Ddit4, which in turn inhibited the mTOR pathway in atrophic cells. Cell Death and Disease (2021)12:652 ; https://doi.org/10.1038/s41419-021-03932-0 INTRODUCTION the overall transcription profile between cancer or noncancer- Cancer cachexia is a multifactorial metabolic syndrome that affects induced muscle atrophy will be greatly helpful in revealing the approximately 50–80% of cancer patients, especially in the uniqueness of the disease. -

Localization of Glucokinase Gene Expression in the Rat Brain Ronald M
Localization of Glucokinase Gene Expression in the Rat Brain Ronald M. Lynch, Linda S. Tompkins, Heddwen L. Brooks, Ambrose A. Dunn-Meynell, and Barry E. Levin The brain contains a subpopulation of glucosensing neu- rons that alter their firing rate in response to elevated glucose concentrations. In pancreatic -cells, gluco- ammalian feeding behavior and general energy kinase (GK), the rate-limiting enzyme in glycolysis, medi- homeostasis appear to be regulated by circu- ates glucose-induced insulin release by regulating intra- lating levels of nutrients (glucose) and pep- cellular ATP production. A similar role for GK is pro- tides (e.g., leptin, insulin). Sensors to detect lev- posed to underlie neuronal glucosensing. Via in situ M els of these factors have been found to reside within specific hybridization, GK mRNA was localized to hypothalamic areas that are thought to contain relatively large popu- nuclei of the hypothalamus (1–8), where central regulation of lations of glucosensing neurons (the arcuate, ventrome- energy homeostasis is believed to be coordinated. For exam- dial, dorsomedial, and paraventricular nuclei and the lat- ple, large changes in blood glucose are correlated with cen- eral area). GK also was found in brain areas without trally mediated responses such as thermogenesis through known glucosensing neurons (the lateral habenula, the activation of the sympathetic nervous system. These changes bed nucleus stria terminalis, the inferior olive, the are monitored by the brain (9–11), and such responses are retrochiasmatic and medial preoptic areas, and the thal- altered in obesity-prone animals (11–13). Moreover, lesions amic posterior paraventricular, interpeduncular, oculo- of the ventromedial hypothalamus (VMH) prevent the hypo- motor, and anterior olfactory nuclei). -

A Specific N-Terminal Extension of the 8 Kda Domain Is Required for DNA End-Bridging by Human Polk and Polj
Published online 8 August 2013 Nucleic Acids Research, 2013, Vol. 41, No. 19 9105–9116 doi:10.1093/nar/gkt681 A specific N-terminal extension of the 8 kDa domain is required for DNA end-bridging by human Polk and Polj Maria Jose Martin*, Maria Victoria Garcia-Ortiz, Ana Gomez-Bedoya, Veronica Esteban, Susana Guerra and Luis Blanco* Centro de Biologia Molecular Severo Ochoa (CSIC-UAM), 28049 Madrid, Spain Received February 27, 2013; Revised July 12, 2013; Accepted July 14, 2013 ABSTRACT state [see Supplementary Figure S1A for an example with Polß; reviewed in (1)]. One role of this conformational Human DNA polymerases mu (Polk) and lambda change is to allow the rapid binding of substrates (and (Polj) are X family members involved in the repair release of products) in the open state, while inducing of double-strand breaks in DNA during non-homolo- optimal alignment of catalytic residues surrounding the gous end joining. Crucial abilities of these enzymes substrates in the closed state. The shape of the base pair include bridging of the two 30 single-stranded over- formed determines the fate of the weakly bound nucleotide hangs and trans-polymerization using one 30 end as during the conformational change step: only a correct base primer and the other as template, to minimize pair induces closing of the enzyme to form a tight catalytic sequence loss. In this context, we have studied complex; conversely, if a mismatched nucleotide is bound, the importance of a previously uncharacterised the enzyme does not close, but rather proceeds to release sequence (‘brooch’), located at the N-terminal the nucleotide while reducing the rate of catalysis. -

DDIT4 Antibody (N-Term) Purified Rabbit Polyclonal Antibody (Pab) Catalog # AP6268A
10320 Camino Santa Fe, Suite G San Diego, CA 92121 Tel: 858.875.1900 Fax: 858.622.0609 DDIT4 Antibody (N-term) Purified Rabbit Polyclonal Antibody (Pab) Catalog # AP6268A Specification DDIT4 Antibody (N-term) - Product Information Application WB, IHC-P,E Primary Accession Q9NX09 Reactivity Human Host Rabbit Clonality Polyclonal Isotype Rabbit Ig Antigen Region 20-49 DDIT4 Antibody (N-term) - Additional Information Gene ID 54541 Other Names DNA damage-inducible transcript 4 protein, HIF-1 responsive protein RTP801, Protein regulated in development and DNA damage Anti-DDIT4 Antibody (N-term) at 1:2000 response 1, REDD-1, DDIT4, REDD1, dilution + Hela whole cell lysate RTP801 Lysates/proteins at 20 µg per lane. Secondary Goat Anti-Rabbit IgG, (H+L), Target/Specificity Peroxidase conjugated at 1/10000 dilution. This DDIT4 antibody is generated from Predicted band size : 25 kDa rabbits immunized with a KLH conjugated Blocking/Dilution buffer: 5% NFDM/TBST. synthetic peptide between 20-49 amino acids from the N-terminal region of human DDIT4. Dilution WB~~1:2000 IHC-P~~1:25 Format Purified polyclonal antibody supplied in PBS with 0.09% (W/V) sodium azide. This antibody is purified through a protein A column, followed by peptide affinity purification. Storage Maintain refrigerated at 2-8°C for up to 2 weeks. For long term storage store at -20°C in small aliquots to prevent freeze-thaw cycles. AP6268a staining DDIT4 in human kidney tissue sections by Immunohistochemistry Precautions (IHC-P - paraformaldehyde-fixed, DDIT4 Antibody (N-term) is for research use paraffin-embedded sections). Tissue was Page 1/3 10320 Camino Santa Fe, Suite G San Diego, CA 92121 Tel: 858.875.1900 Fax: 858.622.0609 only and not for use in diagnostic or fixed with formaldehyde and blocked with 3% therapeutic procedures. -

Downloaded from the UCSC PRO-Seq Library Preparation and Sequencing
ARTICLE https://doi.org/10.1038/s41467-021-21687-2 OPEN Multi-omics analysis reveals contextual tumor suppressive and oncogenic gene modules within the acute hypoxic response ✉ ✉ Zdenek Andrysik1,2, Heather Bender1,2, Matthew D. Galbraith 1,2 & Joaquin M. Espinosa 1,2,3 Cellular adaptation to hypoxia is a hallmark of cancer, but the relative contribution of hypoxia- inducible factors (HIFs) versus other oxygen sensors to tumorigenesis is unclear. We employ 1234567890():,; a multi-omics pipeline including measurements of nascent RNA to characterize transcrip- tional changes upon acute hypoxia. We identify an immediate early transcriptional response that is strongly dependent on HIF1A and the kinase activity of its cofactor CDK8, includes indirect repression of MYC targets, and is highly conserved across cancer types. HIF1A drives this acute response via conserved high-occupancy enhancers. Genetic screen data indicates that, in normoxia, HIF1A displays strong cell-autonomous tumor suppressive effects through a gene module mediating mTOR inhibition. Conversely, in advanced malignancies, expression of a module of HIF1A targets involved in collagen remodeling is associated with poor prog- nosis across diverse cancer types. In this work, we provide a valuable resource for investi- gating context-dependent roles of HIF1A and its targets in cancer biology. 1 Department of Pharmacology, School of Medicine, University of Colorado Anschutz Medical Campus, Aurora, CO, USA. 2 Linda Crnic Institute for Down Syndrome, School of Medicine, University -

Involvement of DNA Polymerase K in the Repair of a Specific Subset of DNA Double-Strand Breaks in Mammalian Cells
Published online 5 May 2007 Nucleic Acids Research, 2007, Vol. 35, No. 11 3551–3560 doi:10.1093/nar/gkm243 Involvement of DNA polymerase k in the repair of a specific subset of DNA double-strand breaks in mammalian cells Jean-Pascal Capp1, Franc¸ ois Boudsocq1, Anne-Gaelle Besnard1, Bernard S. Lopez2, Christophe Cazaux1, Jean-Se´ bastien Hoffmann1 and Yvan Canitrot1,* 1Genetic instability and Cancer group, Institute of Pharmacology and Structural Biology, University Paul Sabatier, UMR CNRS 5089, 205 route de Narbonne, 31077 Toulouse cedex and 2De´ partement de Radiobiologie et Radiopathologie, 60-68 av. Ge´ ne´ ral Leclerc, UMR 217 CNRS-CEA, 92265 Fontenay aux Roses cedex, France Received February 27, 2007; Revised April 2, 2007; Accepted April 3, 2007 ABSTRACT the recently discovered DNA polymerase l (poll) (2,3). Polm and poll share some homology and both have been The repair of DNA double-strand breaks (DSB) described as participating in vitro in the repair of DNA requires processing of the broken ends to complete double-strand breaks (DSB) by non-homologous end the ligation process. Recently, it has been shown joining (NHEJ) (4,5). The hallmark of animals or cells that DNA polymerase k (polk) and DNA polymerase j defective in one of the components of the NHEJ pathway (polj) are both involved in such processing during is an increased sensitivity to ionizing radiation (IR) (6–8). non-homologous end joining in vitro. However, no However, cells isolated from animals knocked out for poll phenotype was observed in animal models defective or polm do not present differences in sensitivity to any for either polk and/or polj.