The Special Senses Objectives • Describe the Sensory Organs of Smell, and Olfaction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

New Theory on Facial Beauty: Ideal Dimensions in the Face and Its Application to Your Practice by Dr
New Theory on Facial Beauty: Ideal Dimensions in the Face And its application to your practice By Dr. Philip Young Aesthetic Facial Plastic Surgery 2015 Bellevue, Washington American Brazilian Aesthetic Meeting • Hello my presentation is on studying some further elements of a new theory on facial beauty called the Circles of Prominence. • Specifically we are going to be studying some key dimensions in the face that I think could possibly help your practice. • I’m from Bellevue Washington Home of Bill Gates, Microsoft and Starbucks. Beauty In my opinion Beauty is the most important trait that we have and it is the one trait that can have the most dramatic impact in our lives. Obviously finding the answer for Beauty is essential in our industry. The answers have alluded us: the magic number of Phi, cephalometrics, the neo classical canons by Leonardo Da Vinci, the averageness theory, etc. have all come short in finding what makes a face beautiful. • The Circles of Prominence is a theory that I discovered in 2003-2005 and was published in the Archives of Facial Plastic Surgery in 2006 and Received the Sir Harold Delf Gillies Award from the American Academy of Facial Plastic Surgery. The Circles of Prominence • Original published Archives FPS 2006 • Based on the idea that there is an ideal • Everything on the face has an ideal as well • Because we spend so much time looking at the iris • All dimensions of the face are related to the width of the iris • Obviously with a better definition of beauty our results in plastic surgery can be improved • The circles of prominence is based on the belief that there is an ideal. -

Acquired Etiologies of Lacrimal System Obstructions
5 Acquired Etiologies of Lacrimal System Obstructions Daniel P. Schaefer Acquired obstructions of the lacrimal excretory outfl ow system will produce the symptoms of epiphora, mucopurulent discharge, pain, dacryocystitis, and even cellulitis, prompting the patient to seek the ophthalmologist for evaluation and treatment. Impaired tear outfl ow may be functional, structural, or both. The causes may be primary – those resulting from infl ammation of unknown causes that lead to occlusive fi brosis—or secondary, resulting from infections, infl amma- tion, trauma, malignancies, toxicity, or mechanical causes. Secondary acquired dacryostenosis and obstruction may result from many causes, both common and obscure. Occasionally, the precise pathogenesis of nasolacrimal duct obstruction will, despite years of investigations, be elusive. To properly evaluate and appropriately treat the patient, the ophthal- mologist must have knowledge and comprehension of the lacrimal anatomy, the lacrimal apparatus, pathophysiology, ocular and nasal relationships, ophthalmic and systemic disease process, as well as the topical and systemic medications that can affect the nasolacrimal duct system. One must be able to assess if the cause is secondary to outfl ow anomalies, hypersecretion or refl ex secretion, pseudoepiphora, eyelid malposition abnormalities, trichiasis, foreign bodies and conjunctival concretions, keratitis, tear fi lm defi ciencies or instability, dry eye syn- dromes, ocular surface abnormalities, irritation or tumors affecting the trigeminal nerve, allergy, medications, or environmental factors. Abnormalities of the lacrimal pump function can result from involu- tional changes, eyelid laxity, facial nerve paralysis, or fl oppy eyelid syndrome, all of which displace the punctum from the lacrimal lake. If the cause is secondary to obstruction of the nasolacrimal duct system, the ophthalmologist must be able to determine where the anomaly is and what the cause is, in order to provide the best treatment possible for the patient. -

The Lacrimal System Terms
The Lacrimal System Lynn E. Lawrence, CPOT, ABOC, COA, OSC Terms • Etiology – the cause of a disease or abnormal condition • Dacryocystitis – inflammation of the lacrimal sac • Epiphora – watering of eyes due to excess secretion of tears or obstruction of the lacrimal passage Tear Film Layers oil aqueous snot What functions does each layer of the tear perform? Lacrimal System: Tear Film Layers LIPID DEFICIENCY ‐ evaporates TEAR DEFICIENCY – fails to hydrate properly oil aqueous snot What functions does each layer of the tear perform? What are functions of tears? Tear Components • Lipid Layer – prevents evaporation • Aqueous Layer ‐ hydration • Mucus Layer – sticks tear to the eye • Other components Lacrimal Apparatus • Sometimes a person cannot produce natural tears they might need punctal plugs to prevent the tears from draining off the eye. • Faucet • Action • Drain Obstructive – vs‐ non‐obstructive Tear Production – Secretory • Lacrimal gland – Reflex tearing – Too much tearing…epiphora • Gland of Krause – Superior fornix • Gland of Wolfring – Superior tarsal plate Two Primary Forms of Dry Eye 800 nm 8,000 nm 100 nm The two primary forms of dry eye are Evaporative Dry Eye, also known as Meibomian Gland Dysfunction or MGD and Aqueous Dry Eye. The majority of dry eye sufferers have MGD. Oil & Water Remember science class? Oil floats. Oil does not mix with water, but rather sits on top of water. Oil is what keeps water from evaporating. Need three volunteers TEST TIME http://optometrytimes.modernmedicine.com/optometrytimes/news/treating‐dry‐eye‐ lipid‐based‐eye‐drops Lipid Secretion: Meibomian Glands Left: Transillumination of eyelid showing meibomian glands Right: Secretion of lipid at lid margin • The lipid layer restricts evaporation to 5‐10% of tear flow – Also helps lubricate Mucin Secretion: Goblet Cells Superficial layer of bulbar conjunctiva. -
Abducens Nerve Lesion • Right LR Is Disabled
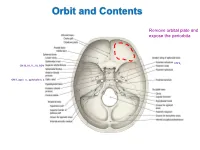
Orbit and Contents Remove orbital plate and expose the periorbita CN V2 CN III, IV, V1, VI, SOV CN II, optic n., ophthalmic a. Orbit and Contents Contents of orbit: • Eyeball and extraocular mm • Nerves to mm and orbital contents • Optic nerve (CN II) – retina; vision • Ciliary ganglion – PS supply to sphincter pupillae and ciliary mm • Ophthalmic artery and veins • Lacrimal gland and ducts • Lacrimal sac and canaliculi • FAT!! Bony Orbit and Walls The orbit is a 4-sided pyramid: Base (orbital margin) – anterolaterally • Frontal, Maxilla, Zygomatic bones Apex - posteromedially Walls: Roof – frontal bone Lateral – zygomatic, greater wing of sphenoid Medial – lesser wing of sphenoid, ethmoid (lamina papyracea), lacrimal, part of maxilla Floor – maxilla (“roof of maxillary sinus”) Three of the four sides are bounded by paranasal sinuses: Superiorly – Frontal sinus (behind eyebrows) Medially – Ethmoidal sinuses (air cells) Inferiorly – Maxillary sinus Bones are thin and vulnerable to “blowout” fractures Bony Orbit and Openings Orbital and Optical Axes and Position of Eyeball in Orbit = visual axis Axes about which movements of the eyeball occur 1. Vertical axis (superior/inferior poles) – rotation of pupil toward nose (=adduction) – rotation of pupil away from nose (=abduction) 2. Transverse axis (mediolateral; at equator) – rotate pupil upward (=elevation) – rotate pupil downward (=depression) 3. Anterior-posterior axis (optical axis, line of sight) – rotate superior pole medially (=intorsion) – rotate superior pole laterally (=extorsion) Only the medial rectus and lateral rectus have pure, singular actions. All others move the eyeball on 3 different axes. Extraocular Muscles Muscle Origin Insertion Innervation Function Levator palpebrae Lesser wing of sphenoid Skin of upper eyelid Oculomotor n. -

ORGAN of VISION the Organ of Vision Includes: 1) Eyeball 2
ORGAN OF VISION The organ of vision includes: 1) Eyeball 2) Auxiliary apparatus (eyebrows, palpebrae, conjunctiva, lacrimal apparatus, extrinsic eye muscles, fat tissue of an orbit), 3) Optic nerve and visual pathway. EYEBALL The eyeball is located in the orbit. It is surrounded by a fibrous sheath (Tenon’s capsule). Between the capsule and the walls of an orbit adipose tissue is located, between the capsule and the eyeball – episcleral (Tenon’s) spase. Eyeball has two poles: anterior and posterior. The line connecting these poles outside – external axis of the eye (an average of about 24 mm), inside – internal axis of the eye (about 22 mm). Thus, external axis connects the convex part of the external surface of the cornea to the convex part of the external surface of the sclera. Internal axis connects the convex part of the internal surface of the cornea to the convex part of the internal surface of the sclera. The line connecting the anterior pole (the convex part of the cornea) with the point of the best vision (center of yellow spot of the retina) - optic axis. Equator of the eye divides it into anterior and posterior segments. The eyeball consists of the nucleus and tunics (layers). LAYERS OF THE EYEBALL: 1. Fibrous tunic 2. Vascular tunic 3. Internal tunic 1.FIBROUS TUNIC It is divided on two parts: the anterior – cornea, posterior – sclera. Cornea is transparent. It hasn’t blood vessels, its shape is convex and thus it refracts light rays coming into the eye. Posterior large part is a sclera (sclerous or albuminous shell = «white»). -

Journalajtcvm(Issue 2)
Neuroanatomic Structure and Function of Acupuncture Points around the Eye Narda G. Robinson, DO, DVM, MS, Jessica Pederson, Ted Burghardt, L. Ray Whalen, DVM PhD ABSTRACT The locations of eight human periocular acupuncture points were transposed to the dog. Canine dissections exposed acupoint-nerve relationships that were compared to those previously identified in the human. Two comparative anatomical differences in periocular points include 1) lack of a complete bony orbit in the dog and absence of cranial nerve foramina, and 2) longer distance between the canine infraorbital foramen and ipsilateral eye than in the human, requiring a different location for ST 2. Traditional Chinese Veterinary Medicine (TCVM) actions assigned to each point were compared to the neurophysiologic results expected after stimulating these nerves. Nerve structure-function relationships of the periocular acupuncture points explain the theoretical TCVM descriptions of point actions. This finding emphasizes the relevance of ensuring that a transpositional point system is based on comparative neuroanatomical precision. Differences exist in periorbital bony anatomy between the dog and the human that call for a re-evaluation of the topographical anatomy of canine periocular acupuncture points. Key Words: Neuroanatomical acupuncture, transpositional points, veterinary acupuncture, Traditional Chinese Veterinary Medicine, TCVM, ophthalmology The effects of acupuncture are associated nervous system and out again through somatic and with “neuromodulation”, which involve the autonomic pathways. Predictable neuromodulation physiologic changes caused by acupuncture that depends upon the accuracy of acupuncture point relate directly to the nerves stimulated.1 Peripheral and nerve stimulation. Obtaining a reliable clinical nerves at acupuncture points impact the body as a outcome with acupuncture requires that the target whole through reflex connections into the central acupuncture point affects the appropriate nerves. -

Clinical Evaluation of Microscintigraphy of the Lacrimal Drainage Apparatus
CLINICAL EVALUATION OF MICROSCINTIGRAPHY OF THE LACRIMAL DRAINAGE APPARATUS William H. Canton, Jon H. Trueblood, and Roger M. Rossomondo Medical College of Georgia, A ugusta, Georgia Lacrimal drainage was studied by sequential paper is to report on microscintigraphy as a clinical imaging (“microscintigraphy―) of the orbit diagnostic tool in the study of the lacrimal drainage after PsmTc was placed in the eyes of 62 patients. system. Specific criteria of normal drainage were de veloped from observations in 28 individuals. MATERIALS AND METHODS Thirty-four epiphoric patients in several cate Approximately 100 @@Ciof 99mTc was placed in gories of lacrimal drainage symptomology were the eye in the form of a 15-d drop. The patient was studied. This technique of microscintigraphy of positioned in front of the gamma camera and record the lacrimal apparatus was shown to be a valu ing was begun approximately 3 sec after the admin able diagnostic tool. istration of the drop. Two-second exposure frames were recorded with a 35-mm camera for the first 20 sec and 40-sec exposure frames were recorded there Many methods have been used to determine the after. After the first 5-mm the patient was allowed to patency of the lacnmal drainage apparatus in man, rest and was repositioned for each additional frame. notably the fluorescein dye test by Jones (1 ), dacryo The field of view of each scintiphoto was approxi cystography described by Campbell (2), Milder mately from the middle of the cornea to the nasal and Demorest (3,4), and Francois and Neetens (5), midline. and the pressure transducer described by Callahan, Forbath, and Besser (6) . -

Anatomy and Physiology of the Nasolacrimal Ducts 1
ChapterAnatomy and 1 Physiology of the Nasolacrimal Ducts Chapter 1 1 Anatomy and Physiology of the Nasolacrimal Ducts 1 Friedrich Paulsen Core Messages! Q The lacrimal sac and nasolacrimal duct are surrounded by a cavernous body. While Q The tear film is produced by the lacrimal regulating the blood flow, the specialized gland and the different structures of the eye blood vessels permit opening and closing of lid. Its composition is controlled by the the lumen of the lacrimal passage affected by lacrimal functional unit. the bulging and subsiding of the cavernous body, while at the same time regulating tear Q The ocular surface epithelia together with outflow. The blood vessels are connected to the lacrimal gland produce a unique subset the vessels of the outer eye and could act as a of membrane bound and secretory mucins feedback signal for tear-fluid production. that stabilize the tear film, fix it to the epithelia, support binding of bacteria, and are of great importance to tear physiology. Q TFF peptides TFF1 and TFF3 of conjunctival Contents origin influence the rheological properties of 1.1 Introduction ................................... 1 the tear film. 1.2 Anatomy and Physiology Q Drainage of tears involves a number of of the Ocular Surface and Adnexa ................ 2 1.2.1 Ocular Surface ................................. 3 different mechanisms; of these the action of 1.2.2 Lacrimal Gland ................................ 4 the lacrimal part of the orbicularis oculi 1.2.3 Eyelid ......................................... 4 muscle is most important to bring tear fluid 1.2.4 The Lacrimal Functional Unit .................... 5 into the lacrimal sac. Epithelial secretion 1.3 Anatomy and Physiology products, the surrounding cavernous body, of the Nasolacrimal Ducts ...................... -
The Gross and Microscopic Structure of the Hamster Eye with Special
AN ABSTRACT OP T1L THESIS OP Lydia Byer1ein for the Master of Arts in Zoology (N&ie) Tbegre) (Major) Date thesis is presented 14 May 1953 Title The gross and microscoic structure of the hamster !2L with special reference to_acomLLdation Abstract approved Recíacted fot'pricy (Major Professor) Gross and histologic studies were made of the hamster eye and of its adnexa. The structure was found to resemble in general the eye of most marnmals An extensive cornea and strategic placement of pigi.ient give it a striking brilLiance. The greater portion of the orbit is filled with a bulky, bi- lobed Harderian gland. Lacrimal and. ileibomian glands are as commonly described. uioptric features are those of' an accommodating eye. Ciliary processes are well developed but a diminutive cil- iary muscle was noted. The muscle cells are slightly atica1 and few in nrnnber and lack an obvious functional arrange- ment. The lens is of moderate size and centrally located.. A circular pupil is ca:ble of changing its diameter. etina1 composition is that of a seeing eye but is probably adaptea scotopically. No cones were recognized and neither macula lutea nor fovea centralis is present. Insertion of the extrinsic ocular muscles of Liesocri- cetus auratus is not via the c1.ssic tendon. No siooth mus- de or structure cf the cardiac type is present in the region of the insertions. Other modifications that could serve a involuntary contractile elements associated. with these mue- cies viere sought but nothing was found. Recti and oblique muscles were not differentiated structurally from the re- tractor bulbi muscle. -

Diagnostic Imaging of the Nasolacrimal Drainage System. Part
REVIEW ARTICLES e-ISSN 1643-3750 © Med Sci Monit, 2014; 20: 628-638 DOI: 10.12659/MSM.890098 Received: 2013.11.27 Accepted: 2014.01.16 Diagnostic imaging of the nasolacrimal drainage Published: 2014.04.17 system. Part I. Radiological anatomy of lacrimal pathways. Physiology of tear secretion and tear outflow Authors’ Contribution: ABCDEFG 1 Artur Maliborski 1 Department of Medical Radiology, Military Institute of Medicine, Warsaw, Poland Study Design A ABCG 2 Radosław Różycki 2 Department of Ophthalmology, Military Institute of Medicine, Warsaw, Poland Data Collection B Statistical Analysis C Data Interpretation D Manuscript Preparation E Literature Search F Funds Collection G Corresponding Author: Artur Maliborski, e-mail: [email protected] Source of support: Departmental sources Excessive watering of the eye is a common condition in ophthalmological practice. It may be the result of ex- cessive production of tear fluid or obstruction and insufficiency of efferent tear pathways. The differentia- tion between obstruction and insufficiency of the lacrimal pathways is still clinically questionable. In the -di agnostic process it is necessary to perform clinical tests and additional diagnostic imaging is often needed. Dacryocystography, with or without the extension of the dynamic phase or subtraction option, still remains the criterion standard for diagnostic imaging of the lacrimal obstruction. It may help to clarify the cause and exact place of the obstruction and provide information for further management, especially surgical treatment. Increasingly, new techniques are used in diagnostic imaging of the lacrimal tract, such as computed tomogra- phy, magnetic resonance, and isotopic methods. Adequate knowledge of the anatomy and physiology of the lacrimal system and the secretion and outflow of tears is the basis for proper diagnostic imaging. -

A Study of the Impact of Eyelid Opening and Closing on The
iseases D an e d y E D f i s o o l r a d n e Wu W et al., J Eye Dis Disord 2018, 3:2 r r s u o J Journal of Eye Diseases and Disorders Research article Open Access A Study of the impact of Eyelid Opening and Closing on the Volume and Morphology of the Lacrimal Sac Tu Yunhai, Wu W*, Chen Y and Shi J Eye Hospital of Wenzhou Medical University, Wenzhou City, China *Corresponding author: Wu W, Eye Hospital of Wenzhou Medical University, Wenzhou City, China, E-mail: [email protected] Received date: March 12, 2018; Accepted date: March 23, 2018; Published date: March 30, 2018 Copyright: ©2018 Wu W, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Purpose: To study the impact of eyelid opening and closing on the volume and morphology of the lacrimal sac using computed tomography (CT) dacryocystography. Method: All of the patients underwent CT dacryocystography. After the contrast agents was injected into a patient's lacrimal sac, the orbit was first scanned with the eye open. And then the patient was told to close the eye firmly for a second scan of the orbit. The volume of the lacrimal sac was calculated by the image processing program which came with the CT machine. At the same time, the anteroposterior and transverse diameters of the lacrimal sac at 3 mm and 7 mm from the top of the lacrimal sac were measured. -

Lacrimal Outflow Physiology
3/16/2018 LACRIMAL OUTFLOW PHYSIOLOGY ASHRAF SABRY, MD , FRCS (ED) . FELLOW OF BASCOM PALMER EYE INSTITUTE , MIAMI UNI .USA . OPHTHALMIC CONSULTANT . HEAD OF OCULOPLASTIC AND EXTERNAL DISEASE UNIT MAGRABI EYE CENTRE JEDDAH ,KSA . LACRIMAL SYSTEM • The function of the lacrimal system is to create an ideal environment for visual functions of the eye. • And optimizing the nutrition and defence of the ocular surface. • It accomplished by balance between the lacrimal secretion and drainage system . • both components of the system are linked functionally and anatomically by continuity of the epithelia, by innervation, and by the endocrine, vascular and immune systems • failure of drainage system , produces not only epiphora but also compromises the functional balance of the entire ocular surface . 1 3/16/2018 TEAR FACTS • Average tear flow of 1.2 µl /min with a range of 0.5 to 2.2 µl /min • The average normal tear volume is 6.2 ± 2.0 µl. • So The entire tear volume in the eye turns over every 2 to 3 minutes. • Capacity of conjunctival sac 25-30 ul which when exceeded tearing occurs . CHALLENGES OF LACRIMAL DRAINING CHALLENGING ASPECTS IDEAL DRAINAGE SYSTEM IN TEAR DRAINAGE • How to push the tear in the very narrow 0.3 mm wide • Should have a pump to push the tears into the lacrimal opening (punctum) system. • How to drain a Diversity of viscosity and rheological • Fits for drainage of different viscosity and different rheological structures. characteristic of tear components (mucin ,aqueous and lipid layer. ) • Should have non adhering properties . • How to Drain the debris and F,B without adhering to • Should have antimicrobial capabilities .