Chapter 17 the Special Senses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Taste and Smell Disorders in Clinical Neurology
TASTE AND SMELL DISORDERS IN CLINICAL NEUROLOGY OUTLINE A. Anatomy and Physiology of the Taste and Smell System B. Quantifying Chemosensory Disturbances C. Common Neurological and Medical Disorders causing Primary Smell Impairment with Secondary Loss of Food Flavors a. Post Traumatic Anosmia b. Medications (prescribed & over the counter) c. Alcohol Abuse d. Neurodegenerative Disorders e. Multiple Sclerosis f. Migraine g. Chronic Medical Disorders (liver and kidney disease, thyroid deficiency, Diabetes). D. Common Neurological and Medical Disorders Causing a Primary Taste disorder with usually Normal Olfactory Function. a. Medications (prescribed and over the counter), b. Toxins (smoking and Radiation Treatments) c. Chronic medical Disorders ( Liver and Kidney Disease, Hypothyroidism, GERD, Diabetes,) d. Neurological Disorders( Bell’s Palsy, Stroke, MS,) e. Intubation during an emergency or for general anesthesia. E. Abnormal Smells and Tastes (Dysosmia and Dysgeusia): Diagnosis and Treatment F. Morbidity of Smell and Taste Impairment. G. Treatment of Smell and Taste Impairment (Education, Counseling ,Changes in Food Preparation) H. Role of Smell Testing in the Diagnosis of Neurodegenerative Disorders 1 BACKGROUND Disorders of taste and smell play a very important role in many neurological conditions such as; head trauma, facial and trigeminal nerve impairment, and many neurodegenerative disorders such as Alzheimer’s, Parkinson Disorders, Lewy Body Disease and Frontal Temporal Dementia. Impaired smell and taste impairs quality of life such as loss of food enjoyment, weight loss or weight gain, decreased appetite and safety concerns such as inability to smell smoke, gas, spoiled food and one’s body odor. Dysosmia and Dysgeusia are very unpleasant disorders that often accompany smell and taste impairments. -

Oral Cavity Histology Histology > Digestive System > Digestive System
Oral Cavity Histology Histology > Digestive System > Digestive System Oral Cavity LINGUAL PAPILLAE OF THE TONGUE Lingual papillae cover 2/3rds of its anterior surface; lingual tonsils cover its posterior surface. There are three types of lingual papillae: - Filiform, fungiform, and circumvallate; a 4th type, called foliate papillae, are rudimentary in humans. - Surface comprises stratified squamous epithelia - Core comprises lamina propria (connective tissue and vasculature) - Skeletal muscle lies deep to submucosa; skeletal muscle fibers run in multiple directions, allowing the tongue to move freely. - Taste buds lie within furrows or clefts between papillae; each taste bud comprises precursor, immature, and mature taste receptor cells and opens to the furrow via a taste pore. Distinguishing Features: Filiform papillae • Most numerous papillae • Their role is to provide a rough surface that aids in chewing via their keratinized, stratified squamous epithelia, which forms characteristic spikes. • They do not have taste buds. Fungiform papillae • "Fungi" refers to its rounded, mushroom-like surface, which is covered by stratified squamous epithelium. Circumvallate papillae • Are also rounded, but much larger and more bulbous. • On either side of the circumvallate papillae are wide clefts, aka, furrows or trenches; though not visible in our sample, serous Ebner's glands open into these spaces. DENTITION Comprise layers of calcified tissues surrounding a cavity that houses neurovascular structures. Key Features Regions 1 / 3 • The crown, which lies above the gums • The neck, the constricted area • The root, which lies within the alveoli (aka, sockets) of the jaw bones. • Pulp cavity lies in the center of the tooth, and extends into the root as the root canal. -

Description of the Chemical Senses of the Florida Manatee, Trichechus Manatus Latirostris, in Relation to Reproduction
DESCRIPTION OF THE CHEMICAL SENSES OF THE FLORIDA MANATEE, TRICHECHUS MANATUS LATIROSTRIS, IN RELATION TO REPRODUCTION By MEGHAN LEE BILLS A DISSERTATION PRESENTED TO THE GRADUATE SCHOOL OF THE UNIVERSITY OF FLORIDA IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY UNIVERSITY OF FLORIDA 2011 1 © 2011 Meghan Lee Bills 2 To my best friend and future husband, Diego Barboza: your support, patience and humor throughout this process have meant the world to me 3 ACKNOWLEDGMENTS First I would like to thank my advisors; Dr. Iskande Larkin and Dr. Don Samuelson. You showed great confidence in me with this project and allowed me to explore an area outside of your expertise and for that I thank you. I also owe thanks to my committee members all of whom have provided valuable feedback and advice; Dr. Roger Reep, Dr. David Powell and Dr. Bruce Schulte. Thank you to Patricia Lewis for her histological expertise. The Marine Mammal Pathobiology Laboratory staff especially Drs. Martine deWit and Chris Torno for sample collection. Thank you to Dr. Lisa Farina who observed the anal glands for the first time during a manatee necropsy. Thank you to Astrid Grosch for translating Dr. Vosseler‟s article from German to English. Also, thanks go to Mike Sapper, Julie Sheldon, Kelly Evans, Kelly Cuthbert, Allison Gopaul, and Delphine Merle for help with various parts of the research. I also wish to thank Noelle Elliot for the chemical analysis. Thank you to the Aquatic Animal Health Program and specifically: Patrick Thompson and Drs. Ruth Francis-Floyd, Nicole Stacy, Mike Walsh, Brian Stacy, and Jim Wellehan for their advice throughout this process. -

UC Davis Dermatology Online Journal
UC Davis Dermatology Online Journal Title Goodness, gracious, great balls of fire: A case of transient lingual papillitis following consumption of an Atomic Fireball Permalink https://escholarship.org/uc/item/91j9n0kt Journal Dermatology Online Journal, 22(5) Authors Raji, Kehinde Ranario, Jennifer Ogunmakin, Kehinde Publication Date 2016 DOI 10.5070/D3225030941 License https://creativecommons.org/licenses/by-nc-nd/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Volume 22 Number 5 May 2016 Case Report Goodness, gracious, great balls of fire: A case of transient lingual papillitis following consumption of an Atomic Fireball. Kehinde Raji MD MPH, 1 Jennifer Ranario MD,2 Kehinde Ogunmakin MD2 Dermatology Online Journal 22 (5): 3 1 Scripps Clinic/Scripps Green Hospital, Department of Medicine, San Diego, CA 2 Texas Tech University Health Sciences Center, Department of Dermatology, Lubbock TX Correspondence: Kehinde Raji, MD MPH. Scripps Green Hospital 10666 North Torrey Pines Rd San Diego, CA 92037. Tel. +1 (858)-554-3236. Fax. +1 (858)-554-3232 Email: [email protected] Abstract Transient lingual papillitis is a benign condition characterized by the inflammation of one or more fungiform papillae on the dorsolateral tongue. Although it is a common condition that affects more than half of the population, few cases have been reported in the dermatological literature. Therefore, it is a condition uncommonly recognized by dermatologists though it has a distinct clinical presentation that may be easily diagnosed by clinicians familiar with the entity. We report an interesting case of transient lingual papillitis in a 27 year-old healthy woman following the consumption of the hard candy, Atomic Fireball. -

New Theory on Facial Beauty: Ideal Dimensions in the Face and Its Application to Your Practice by Dr
New Theory on Facial Beauty: Ideal Dimensions in the Face And its application to your practice By Dr. Philip Young Aesthetic Facial Plastic Surgery 2015 Bellevue, Washington American Brazilian Aesthetic Meeting • Hello my presentation is on studying some further elements of a new theory on facial beauty called the Circles of Prominence. • Specifically we are going to be studying some key dimensions in the face that I think could possibly help your practice. • I’m from Bellevue Washington Home of Bill Gates, Microsoft and Starbucks. Beauty In my opinion Beauty is the most important trait that we have and it is the one trait that can have the most dramatic impact in our lives. Obviously finding the answer for Beauty is essential in our industry. The answers have alluded us: the magic number of Phi, cephalometrics, the neo classical canons by Leonardo Da Vinci, the averageness theory, etc. have all come short in finding what makes a face beautiful. • The Circles of Prominence is a theory that I discovered in 2003-2005 and was published in the Archives of Facial Plastic Surgery in 2006 and Received the Sir Harold Delf Gillies Award from the American Academy of Facial Plastic Surgery. The Circles of Prominence • Original published Archives FPS 2006 • Based on the idea that there is an ideal • Everything on the face has an ideal as well • Because we spend so much time looking at the iris • All dimensions of the face are related to the width of the iris • Obviously with a better definition of beauty our results in plastic surgery can be improved • The circles of prominence is based on the belief that there is an ideal. -

Tongue Anatomy 25/03/13 11:05
Tongue Anatomy 25/03/13 11:05 Medscape Reference Reference News Reference Education MEDLINE Tongue Anatomy Author: Eelam Aalia Adil, MD, MBA; Chief Editor: Arlen D Meyers, MD, MBA more... Updated: Jun 29, 2011 Overview The tongue is basically a mass of muscle that is almost completely covered by a mucous membrane. It occupies most of the oral cavity and oropharynx. It is known for its role in taste, but it also assists with mastication (chewing), deglutition (swallowing), articulation (speech), and oral cleaning. Five cranial nerves contribute to the complex innervation of this multifunctional organ. The embryologic origins of the tongue first appear at 4 weeks' gestation.[1] The body of the tongue forms from derivatives of the first branchial arch. This gives rise to 2 lateral lingual swellings and 1 median swelling (known as the tuberculum impar). The lateral lingual swellings slowly grow over the tuberculum impar and merge, forming the anterior two thirds of the tongue. Parts of the second, third, and fourth branchial arches give rise to the base of the tongue. Occipital somites give rise to myoblasts, which form the intrinsic tongue musculature. Gross Anatomy From anterior to posterior, the tongue has 3 surfaces: tip, body, and base. The tip is the highly mobile, pointed anterior portion of the tongue. Posterior to the tip lies the body of the tongue, which has dorsal (superior) and ventral (inferior) surfaces (see the image and the video below). Tongue, dorsal view. View of ventral (top) and dorsal (bottom) surfaces of tongue. On dorsal surface, taste buds (vallate papillae) are visible along junction of anterior two thirds and posterior one third of the tongue. -

Acquired Etiologies of Lacrimal System Obstructions
5 Acquired Etiologies of Lacrimal System Obstructions Daniel P. Schaefer Acquired obstructions of the lacrimal excretory outfl ow system will produce the symptoms of epiphora, mucopurulent discharge, pain, dacryocystitis, and even cellulitis, prompting the patient to seek the ophthalmologist for evaluation and treatment. Impaired tear outfl ow may be functional, structural, or both. The causes may be primary – those resulting from infl ammation of unknown causes that lead to occlusive fi brosis—or secondary, resulting from infections, infl amma- tion, trauma, malignancies, toxicity, or mechanical causes. Secondary acquired dacryostenosis and obstruction may result from many causes, both common and obscure. Occasionally, the precise pathogenesis of nasolacrimal duct obstruction will, despite years of investigations, be elusive. To properly evaluate and appropriately treat the patient, the ophthal- mologist must have knowledge and comprehension of the lacrimal anatomy, the lacrimal apparatus, pathophysiology, ocular and nasal relationships, ophthalmic and systemic disease process, as well as the topical and systemic medications that can affect the nasolacrimal duct system. One must be able to assess if the cause is secondary to outfl ow anomalies, hypersecretion or refl ex secretion, pseudoepiphora, eyelid malposition abnormalities, trichiasis, foreign bodies and conjunctival concretions, keratitis, tear fi lm defi ciencies or instability, dry eye syn- dromes, ocular surface abnormalities, irritation or tumors affecting the trigeminal nerve, allergy, medications, or environmental factors. Abnormalities of the lacrimal pump function can result from involu- tional changes, eyelid laxity, facial nerve paralysis, or fl oppy eyelid syndrome, all of which displace the punctum from the lacrimal lake. If the cause is secondary to obstruction of the nasolacrimal duct system, the ophthalmologist must be able to determine where the anomaly is and what the cause is, in order to provide the best treatment possible for the patient. -

The Lacrimal System Terms
The Lacrimal System Lynn E. Lawrence, CPOT, ABOC, COA, OSC Terms • Etiology – the cause of a disease or abnormal condition • Dacryocystitis – inflammation of the lacrimal sac • Epiphora – watering of eyes due to excess secretion of tears or obstruction of the lacrimal passage Tear Film Layers oil aqueous snot What functions does each layer of the tear perform? Lacrimal System: Tear Film Layers LIPID DEFICIENCY ‐ evaporates TEAR DEFICIENCY – fails to hydrate properly oil aqueous snot What functions does each layer of the tear perform? What are functions of tears? Tear Components • Lipid Layer – prevents evaporation • Aqueous Layer ‐ hydration • Mucus Layer – sticks tear to the eye • Other components Lacrimal Apparatus • Sometimes a person cannot produce natural tears they might need punctal plugs to prevent the tears from draining off the eye. • Faucet • Action • Drain Obstructive – vs‐ non‐obstructive Tear Production – Secretory • Lacrimal gland – Reflex tearing – Too much tearing…epiphora • Gland of Krause – Superior fornix • Gland of Wolfring – Superior tarsal plate Two Primary Forms of Dry Eye 800 nm 8,000 nm 100 nm The two primary forms of dry eye are Evaporative Dry Eye, also known as Meibomian Gland Dysfunction or MGD and Aqueous Dry Eye. The majority of dry eye sufferers have MGD. Oil & Water Remember science class? Oil floats. Oil does not mix with water, but rather sits on top of water. Oil is what keeps water from evaporating. Need three volunteers TEST TIME http://optometrytimes.modernmedicine.com/optometrytimes/news/treating‐dry‐eye‐ lipid‐based‐eye‐drops Lipid Secretion: Meibomian Glands Left: Transillumination of eyelid showing meibomian glands Right: Secretion of lipid at lid margin • The lipid layer restricts evaporation to 5‐10% of tear flow – Also helps lubricate Mucin Secretion: Goblet Cells Superficial layer of bulbar conjunctiva. -
Abducens Nerve Lesion • Right LR Is Disabled
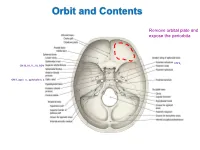
Orbit and Contents Remove orbital plate and expose the periorbita CN V2 CN III, IV, V1, VI, SOV CN II, optic n., ophthalmic a. Orbit and Contents Contents of orbit: • Eyeball and extraocular mm • Nerves to mm and orbital contents • Optic nerve (CN II) – retina; vision • Ciliary ganglion – PS supply to sphincter pupillae and ciliary mm • Ophthalmic artery and veins • Lacrimal gland and ducts • Lacrimal sac and canaliculi • FAT!! Bony Orbit and Walls The orbit is a 4-sided pyramid: Base (orbital margin) – anterolaterally • Frontal, Maxilla, Zygomatic bones Apex - posteromedially Walls: Roof – frontal bone Lateral – zygomatic, greater wing of sphenoid Medial – lesser wing of sphenoid, ethmoid (lamina papyracea), lacrimal, part of maxilla Floor – maxilla (“roof of maxillary sinus”) Three of the four sides are bounded by paranasal sinuses: Superiorly – Frontal sinus (behind eyebrows) Medially – Ethmoidal sinuses (air cells) Inferiorly – Maxillary sinus Bones are thin and vulnerable to “blowout” fractures Bony Orbit and Openings Orbital and Optical Axes and Position of Eyeball in Orbit = visual axis Axes about which movements of the eyeball occur 1. Vertical axis (superior/inferior poles) – rotation of pupil toward nose (=adduction) – rotation of pupil away from nose (=abduction) 2. Transverse axis (mediolateral; at equator) – rotate pupil upward (=elevation) – rotate pupil downward (=depression) 3. Anterior-posterior axis (optical axis, line of sight) – rotate superior pole medially (=intorsion) – rotate superior pole laterally (=extorsion) Only the medial rectus and lateral rectus have pure, singular actions. All others move the eyeball on 3 different axes. Extraocular Muscles Muscle Origin Insertion Innervation Function Levator palpebrae Lesser wing of sphenoid Skin of upper eyelid Oculomotor n. -

Chorda Tympani Nerve Transection at Different Developmental Ages Produces Differential Effects on Taste Bud Volume and Papillae Morphology in the Rat Suzanne I
University of Nebraska at Omaha DigitalCommons@UNO Psychology Faculty Publications Department of Psychology 2005 Chorda tympani nerve transection at different developmental ages produces differential effects on taste bud volume and papillae morphology in the rat Suzanne I. Sollars University of Nebraska at Omaha, [email protected] Follow this and additional works at: https://digitalcommons.unomaha.edu/psychfacpub Part of the Psychology Commons Recommended Citation Sollars, Suzanne I., "Chorda tympani nerve transection at different developmental ages produces differential effects on taste bud volume and papillae morphology in the rat" (2005). Psychology Faculty Publications. 223. https://digitalcommons.unomaha.edu/psychfacpub/223 This Article is brought to you for free and open access by the Department of Psychology at DigitalCommons@UNO. It has been accepted for inclusion in Psychology Faculty Publications by an authorized administrator of DigitalCommons@UNO. For more information, please contact [email protected]. HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author J Neurobiol Manuscript Author . Author manuscript; Manuscript Author available in PMC 2016 July 28. Published in final edited form as: J Neurobiol. 2005 September 5; 64(3): 310–320. doi:10.1002/neu.20140. Chorda Tympani Nerve Transection at Different Developmental Ages Produces Differential Effects on Taste Bud Volume and Papillae Morphology in the Rat Suzanne I. Sollars Department of Psychology, 418 Allwine Hall, University of Nebraska Omaha, Omaha, Nebraska 68182 Abstract Chorda tympani nerve transection (CTX) results in morphological changes to fungiform papillae and associated taste buds. When transection occurs during neonatal development in the rat, the effects on fungiform taste bud and papillae structure are markedly more severe than observed following a comparable surgery in the adult rat. -

The Special Senses Objectives • Describe the Sensory Organs of Smell, and Olfaction
The Special Senses Objectives • Describe the sensory organs of smell, and olfaction. • Identify the accessory and internal structures of the eye, and explain their function. • Explain how light stimulates the production of nerve impulses and vision. • Describe the structures of the external and middle ear and explain how they function. • Describe the parts of the inner ear and their roles in equilibrium and hearing. Olfactory organs • Contain olfactory epithelium with olfactory receptors, supporting cells, basal cells • Olfactory receptors are modified neurons • Olfaction detects dissolved chemicals as they interact with odorant binding proteins Olfaction • Olfactory pathways • No synapse in the thalamus for arriving information • Olfactory discrimination • Can distinguish thousands of chemical stimuli • CNS interprets smells by pattern of receptor activity • Olfactory receptor population shows considerable turnover • Number of receptors declines with age Gustation Taste receptors • Clustered in taste buds • Associated with lingual papillae Taste buds • Gustatory cells extend taste hairs through a narrow taste pore Gustatory pathways • Taste buds are monitored by cranial nerves • Synapse with the medulla oblongata, then thalamus and the primary sensory cortex Gustatory discrimination • Primary taste sensations • Sweet, sour, salty, bitter • Receptors also exist for umami and water • Taste sensitivity shows significant individual differences, some of which are inherited • The number of taste buds declines with age 82 Vision Accessory structures -

ORGAN of VISION the Organ of Vision Includes: 1) Eyeball 2
ORGAN OF VISION The organ of vision includes: 1) Eyeball 2) Auxiliary apparatus (eyebrows, palpebrae, conjunctiva, lacrimal apparatus, extrinsic eye muscles, fat tissue of an orbit), 3) Optic nerve and visual pathway. EYEBALL The eyeball is located in the orbit. It is surrounded by a fibrous sheath (Tenon’s capsule). Between the capsule and the walls of an orbit adipose tissue is located, between the capsule and the eyeball – episcleral (Tenon’s) spase. Eyeball has two poles: anterior and posterior. The line connecting these poles outside – external axis of the eye (an average of about 24 mm), inside – internal axis of the eye (about 22 mm). Thus, external axis connects the convex part of the external surface of the cornea to the convex part of the external surface of the sclera. Internal axis connects the convex part of the internal surface of the cornea to the convex part of the internal surface of the sclera. The line connecting the anterior pole (the convex part of the cornea) with the point of the best vision (center of yellow spot of the retina) - optic axis. Equator of the eye divides it into anterior and posterior segments. The eyeball consists of the nucleus and tunics (layers). LAYERS OF THE EYEBALL: 1. Fibrous tunic 2. Vascular tunic 3. Internal tunic 1.FIBROUS TUNIC It is divided on two parts: the anterior – cornea, posterior – sclera. Cornea is transparent. It hasn’t blood vessels, its shape is convex and thus it refracts light rays coming into the eye. Posterior large part is a sclera (sclerous or albuminous shell = «white»).