Pre-Orthodontic Periodontal Augmentation for Lower Incisor Introducing Invisalign® First Advancement in Adolescent Patients Clear Aligners, Specifically JAMES B
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Class III Malocclusion Treated Non-Surgically with Invisalign, Mandibular Fixed Appliances and Mandibular Tads by Randy J
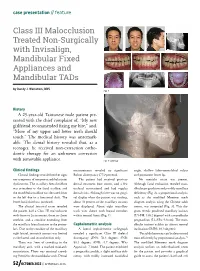
case presentation // feature Class III Malocclusion Treated Non-Surgically with Invisalign, Mandibular Fixed Appliances and Mandibular TADs by Randy J. Weinstein, DDS Fig. 1 History A 25-year-old Taiwanese male patient pre- sented with the chief complaint of, “My new girlfriend recommended fixing my bite,” and, “More of my upper and lower teeth should touch.” The medical history was unremark- able. The dental history revealed that, as a teenager, he received non-extraction ortho- dontic therapy for an unknown correction with removable appliance. Fig. 2: Overlay Clinical findings measurements revealed no significant angle, shallow labio-mentolabial sulcus Clinical findings revealed neither signs Bolton discrepancy (77.9 percent). and prominent lower lip. nor symptoms of temporomandibular joint The patient had received previous No mentalis strain was present. dysfunction. The maxillary dental midline dental treatment (one crown, and a few Although facial evaluation revealed man- was coincident to the facial midline, and occlusal restorations) and had regular dibular prognathism and possibly maxillary the mandibular midline was deviated 2mm dental visits. Although there was no gingi- deficiency (Fig. 2), a proportional analysis, to the left due to a functional shift. The val display when the patient was smiling, such as the modified Moorrees mesh lower facial third was increased. about 70 percent of the maxillary incisors diagram analysis using the Chinese adult The clinical intraoral exam revealed were displayed. About eight maxillary norms, was computed (Fig. 3). This dia- the patient had a Class III malocclusion teeth were shown with buccal corridors gram reveals proclined maxillary incisors with 0mm to 2mm overjet, 0mm to -2mm within normal limits (Fig. -

An Overview on Interproximal Enamel Reduction
DENTISTRY ISSN 2377-1623 http://dx.doi.org/10.17140/DOJ-1-104 Open Journal Review An Overview on Interproximal Enamel *Corresponding author Reduction Yanqi Yang Assistant Professor in Orthodontics Faculty of Dentistry, the University of Deborah Chee#, Chong Ren# and Yanqi Yang* Hong Kong, 2/F, Prince Philip Dental Hospital, 34 Hospital Road, Sai Ying #equally contributed Pun, Hong Kong, China Tel. +852-28590252 Orthodontics, Faculty of Dentistry, the University of Hong Kong, 34 Hospital Road, Hong Kong Fax: +852-25593803 SAR, China E-mail: [email protected] Volume 1 : Issue 1 ABSTRACT Article Ref. #: 1000DOJ1104 Ever since its first introduction seven decades ago, there has been continuous advance- ment of the concept and technique of Interproximal enamel reduction (IPR). It’s demonstrated Article History that with correct case selection and clinical performance, IPR is safe and effective for alleviat- Received: October 28th, 2014 ing crowding, improving dental and gingival aesthetics as well as facilitating post-treatment Accepted: December 5th, 2014 stability. The fulfilment of treatment outcomes depends on careful pre-treatment examination Published: December 8th, 2014 and planning, appropriate clinical procedures and effective post-treatment protection. This re- view aims to provide a general introduction to IPR in terms of its history background, risks and Citation benefits and clinical performance. Chee D, Ren C, Yang Y. An overview on interproximal enamel reduction. Dent Open J. 2014; 1(1): 14-18. doi: KEYWORDS: Interproximal enamel reduction; Orthodontic treatment; Crowding; Tooth re- 10.17140/DOJ-1-104 contouring. INTRODUCTION Interproximal enamel reduction (IPR) also described as “stripping”, “reproximation” and “slenderizing” has been applied in clinical orthodontics for almost seven decades.1,2 By removing part of the enamel tissue from the interproximal contact area, this technique has been proved to be effective in improving dental alignment, stability and aesthetics. -

Orthodontics & Esthetic Dentistry
SCIENTIFIC SESSION TORONTO 2016 ORTHODONTICS & ESTHETIC DENTISTRY: MISSION POSSIBLE! A Broader Approach to Interdisciplinary Esthetic Treatment David M. Sarver, DMD, MS AACD 2016 TORONTO: THURSDAY MORNING “TRIPLE PLAY!” One Session. One Theme. Three Big Hitters. Dr. David M. Sarver, along with Dr. J. William Robbins and Dr. Jeffrey Rouse, will “cover the bases” on diagnosis, decision making, and treatment planning. These three “big hitters” will be presenting sequentially in the same room on Thursday, April 28, 2016. Dr. Sarver will present “Orthodontics— How it Has Changed and What You Really Want to Know!” This article discusses how orthodontics is incorporating smile design principles into its overall functional and esthetic treatment goals. Abstract For decades, dentistry has been evolving into a Patients seeking esthetic profession that is extremely multifaceted and varied in its approach to both smile and facial esthetics. treatment today wish to The coordination of macro esthetics (the face), mini enhance their appearance esthetics (the smile), and micro esthetics (the dental for improved self-esteem esthetic component) offers a complete approach to esthetic planning. This article presents an expanded and quality of life. vision of esthetic treatment designed to take readers to another level of facial, smile, and dental esthetic planning that can elevate patient outcomes. Key Words: macro esthetics, mini esthetics, micro esthetics, orthodontics, smile design 14 Winter 2016 • Volume 31 • Number 4 Sarver Figure 1: In both multidisciplinary and orthodontic diagnosis, three esthetic divisions are advocated: macro esthetics (the face), mini esthetics (the smile), and micro esthetics (the teeth). …there are principles of cosmetic dentistry that orthodontists can use to enhance their work to provide a superior esthetic outcome. -

An Overview on Interproximal Enamel Reduction Review
DENTISTRY ISSN 2377-1623 http://dx.doi.org/10.17140/DOJ-1-104 Open Journal Review An Overview on Interproximal Enamel *Corresponding author Reduction Yanqi Yang Assistant Professor in Orthodontics Faculty of Dentistry, the University of Deborah Chee#, Chong Ren# and Yanqi Yang* Hong Kong, 2/F, Prince Philip Dental Hospital, 34 Hospital Road, Sai Ying #equally contributed Pun, Hong Kong, China Tel. +852-28590252 Orthodontics, Faculty of Dentistry, the University of Hong Kong, 34 Hospital Road, Hong Kong Fax: +852-25593803 SAR, China E-mail: [email protected] Volume 1 : Issue 1 ABSTRACT Article Ref. #: 1000DOJ1104 Ever since its first introduction seven decades ago, there has been continuous advance- ment of the concept and technique of Interproximal enamel reduction (IPR). It’s demonstrated Article History that with correct case selection and clinical performance, IPR is safe and effective for alleviat- Received: October 28th, 2014 ing crowding, improving dental and gingival aesthetics as well as facilitating post-treatment Accepted: December 5th, 2014 stability. The fulfilment of treatment outcomes depends on careful pre-treatment examination Published: December 8th, 2014 and planning, appropriate clinical procedures and effective post-treatment protection. This re- view aims to provide a general introduction to IPR in terms of its history background, risks and Citation benefits and clinical performance. Chee D, Ren C, Yang Y. An overview on interproximal enamel reduction. Dent Open J. 2014; 1(1): 14-18. doi: KEYWORDS: Interproximal enamel reduction; Orthodontic treatment; Crowding; Tooth re- 10.17140/DOJ-1-104 contouring. INTRODUCTION Interproximal enamel reduction (IPR) also described as “stripping”, “reproximation” and “slenderizing” has been applied in clinical orthodontics for almost seven decades.1,2 By removing part of the enamel tissue from the interproximal contact area, this technique has been proved to be effective in improving dental alignment, stability and aesthetics. -

Movingnot Removing Enamel
VOLUME 01 / ISSUE 01 The Academy for Clear Aligner Therapy the AmericanJournal Academy of Cosmetic Orthodontics MOVING not removing ENAMEL. PEER-REVIEWED SOLUTIONS that will make Clear Aligner Treatment THAT MUCH EASIER. Like this Journal? start receiving your quarterly issue today! The official academy for Clear Aligner Therapy. Become a member TODAY! www.aacortho.com AACO Board Members Dr. David Galler: President the Dr. Mark Hodge: Vice President Dr. Perry Jones: Director of Education Dr. Jeffrey Galler: Editor AmericanJournal Academy of Cosmetic Orthodontics Dr. Len Tau: Director of Media Relations Dr. Bruce McFarlane: Orthodontist, Advisory Board Article is Peer Reviewed Article offers CE Credit at www.aacortho.com Dr. David Harrnick: Orthodontist, Advisory Board Dr. Sandi Bosin: Orthodontist, Editorial Board Case Reports Dr. Peter Rivolli: ClearCorrect Clinical Expert Dr. Yana Shampanksy: Invisalign Expert 2 Upper Lateral Incisor Crossbite with Dr. Lori Trost: MTM Clinical Expert Lower Premolar in Lingual Version by Dr. Cathy Sherry 4 Invisalign Correction of a Teenager’s Class 2 Division 1 Malocclusion by Dr. David J. Harnick 8 Upper Arch Spacing and Lower Editorial Arch Overcrowding I’ve been reading numerous by Dr. David Galler dental journals every Practice Development month for many years, 14 The Economics of Buying vs. but don’t remember ever Renting Your Next Office actually reading an editorial completely, from beginning by Jake Jacklich to end. 16 “Doctor, I’ve been your patient for I resolved that in this, my first 10 years; how come you never editorial for the Journal of the American mentioned orthodontics before?” Academy of Cosmetic Orthodontics, by Gary Kadi I would write an editorial that readers Retention would, in fact, read from the very first to the very last word. -

Orthodontic Treatment of Class Three Malocclusion Using Clear Aligners
Journal of Oral Biology and Craniofacial Research 9 (2019) 360–362 Contents lists available at ScienceDirect Journal of Oral Biology and Craniofacial Research journal homepage: www.elsevier.com/locate/jobcr Case study Orthodontic treatment of class three malocclusion using clear aligners: A case report T ∗ Edoardo Staderini , Simonetta Meuli, Patrizia Gallenzi Institute of Dentistry and Maxillofacial Surgery, Fondazione Policlinico Universitario A. Gemelli IRCCS, Università Cattolica del Sacro Cuore, Largo A, Gemelli N°1, Rome, RM, 00168, Italy ARTICLE INFO ABSTRACT Keywords: Class III malocclusion is a growth-related challenging condition for orthodontists. We present a case of a 11-year- Angle class III old girl with a skeletal class III malocclusion with bilateral cross bite, and a functional shift of the lower dental Clear aligner midline. A multiphase clear aligners' treatment was scheduled with the aim of removing all dental interferences Interceptive orthodontic treatment which involved an anterior displacement of the mandible. At one-year follow-up, clear aligners’ therapy resulted in skeletal and dental improvements. Clear aligners therapy represents a valid alternative to fixed appliance therapy in the early interception of class III malocclusion. The present manuscript was prepared following the CARE guidelines. 1. Introduction relation was noticed.4 At intraoral evaluation, the patient presented a late mixed dentition with a bilateral class III malocclusion, along with a Class III malocclusion is a challenging dentoalveolar growth defor- functional mandibular lateral deviation towards the patient's left side, mity, affecting between 5.5% and 19.4% of the population.1 Early without any sign or symptom of temporomandibular joint disorders. -
3D Airway Changes Using CBCT in Patients Following Mandibular Setback Surgery ± Maxillary Advancement
Received: 5 December 2018 | Accepted: 7 December 2018 DOI: 10.1111/ocr.12291 SUPPLEMENT ARTICLE 3D Airway changes using CBCT in patients following mandibular setback surgery ± maxillary advancement Andrew G. Havron1 | Sharon Aronovich2 | Anita V. Shelgikar3 | H. Ludia Kim4 | R. Scott Conley5 1Department of Orthodontics and Pediatric Dentistry, University of Michigan, Ann Structured Abstract Arbor, Michigan Introduction: The aim of this study was to determine the 3D airway changes that 2 Department of Oral and Maxillofacial occur following mandibular setback surgery alone vs bimaxillary surgery in patients Surgery, University of Michigan, Ann Arbor, Michigan with similar skeletal start forms. 3Department of Neurology, University of Setting and Sample Population: The University of Michigan School of Dentistry and Michigan, Ann Arbor, Michigan Medical Center. A total of 85 patients undergoing mandibular setback with or with- 4Private Practice, Ann Arbor, Michigan out simultaneous maxillary advancement. 5Department of Orthodontics, University at Buffalo, Buffalo, New York Materials and Methods: A retrospective evaluation of pre- and post- surgical CBCT scans for patients undergoing mandibular setback surgery alone (14) vs bimaxillary Correspondence R. Scott Conley, University at Buffalo School surgery (71) was performed. Cross- sectional evaluation at standardized locations, of Dental Medicine, Buffalo, NY. minimum cross section and volumetric analysis were performed (Dolphin Imaging & Email: [email protected] Management Solutions). Results: Patients who underwent mandibular setback surgery alone showed a statis- tically significant average increase of 47.5 mm2 in minimum axial area. Patients who underwent bimaxillary surgery showed a statistically significant increase in airway volume, minimum axial area, location of minimum axial area, and axial area at the re- tropalatal and retroglossal regions. -

Journal of Cosmetic Dentistry
Journal of Cosmetic Dentistry Rubber Dam First Calin Pop, DDS Analysis with Imaging & Photography Conservative Composite Bonding 2020 VOLUME 36 ISSUE 3 “We asked, they delivered!” Based on AACD members’ feedback, Ivoclar Vivadent developed a NEW Higher Viscocity Veneer Cement. Amanda Seay, DDS, FAACD INTRODUCING Variolink® Esthetic LC HV Higher viscosity light curing cement • Controlled seating GET YOUR FREE REFILL AT • Precise cleanup blog.ivoclarvivadent.us/free-variolink-sample • Ideal for veneers ivoclarvivadent.com For more information, call us at 1-800-533-6825 in the U.S., 1-800-263-8182 in Canada. © 2020 Ivoclar Vivadent, Inc. Ivoclar Vivadent and Variolink are registered trademarks of Ivoclar Vivadent, Inc. 13722_VE LC HV_JCD.indd 1 11/3/20 3:51 PM A PEER-REVIEWED PUBLICATION OF THE AMERICAN ACADEMY OF COSMETIC DENTISTRY EDITORIAL REVIEW BOARD Pinhas Adar, MDT, CDT, Atlanta, GA Irfan Ahmad, BDS, Middlesex, United Kingdom Somkiat Aimplee, DDS, MSc, AAACD, Bangkok, Thailand volume 36 issue 3 Gary Alex, DMD, AAACD, Huntington, NY Journal of Cosmetic Dentistry Edward P. Allen, DDS, PhD, Dallas, TX Chad J. Anderson, DMD, MS, Fresno, CA Elizabeth M. Bakeman, DDS, FAACD, Grand Rapids, MI Lee Ann Brady, DMD, Glendale, AZ Kevin M. Brown, DDS, AAACD, Bellevue, WA Ricardo M. Carvalho, DDS, PhD, Vancouver, BC, Canada EDITOR-IN-CHIEF Edward Lowe, DMD, AAACD Christian Coachman, DDS, CDT, Sáo Paulo, Brazil Vancouver, BC, Canada, [email protected] John C. Cranham, DDS, Chesapeake, VA EXECUTIVE DIRECTOR Barbara J. Kachelski, MBA, CAE, [email protected] Michael W. Davis, DDS, Santa Fe, NM Newton Fahl Jr., DDS, MS, Curitiba-PR, Brazil CHIEF MARKETING OFFICER Mike DiFrisco, CAE, [email protected] Jonathan L. -

Topics in Pediatric Dentistry
Chapter 6: Topics in Pediatric Dentistry 8 CE Hours By: Elite Staff Learning objectives Identify the primary ways pediatric dentistry differs from treating List potential risks and contraindications for local anesthesia. adults. Discuss recent findings regarding xylitol and caries risk reduction. List the goals of behavior guidance. List a recommended use for restorative procedures described in List and describe the main components and objectives of the dental this course. consultation. List the clinical examination steps for unfavorable developing List four nonpharmacological behavior guidance strategies and dentition and occlusion. explain what is involved in each method. List the primary objectives for occlusion for each stage of Discuss some of the pros and cons of having parents present dentition. during treatment. Discuss the protocol for supernumerary teeth from infancy to Explain why nitrous oxide is typically preferred over protective young adolescent. stabilization as an advanced behavior guidance strategy. Describe the characteristics, causes and management of List contraindications and potential adverse effects for nitrous odontogenic infections in children. oxide/oxygen inhalation. Discuss the risks associated with excessive antibiotic therapy. List documentation requirements for deep sedation/general anesthesia. Introduction Pediatric dentistry differs from treating adults in a number of ● Nitrous oxide use. significant ways. While the dental professional’s primary objective is ● Local anesthesia use. always to facilitate optimum oral health for the patient through the best ● Caries risk-assessment and management. prevention and treatment methods, practitioners working with children ● Restorative dentistry. also have the priority of creating a positive formative experience, ● Management of the developing dentition and occlusion. placing additional emphasis on establishing a safe, comfortable ● Oral surgery. -

CHAPTER 9 Special Considerations in Diagnosis and Treatment Planning 277
CHAPTER 9 Special Considerations in Diagnosis and Treatment Planning 277 A B C FIGURE 9-38 A, The frontal smile relationship demonstrates diminished incisor display on smile. B, On sagittal smile, the flare and proclination of the upper incisors are apparent. C, Before treat- ment, a mild anterior open bite was present, and the flare of the maxillary incisors contributes to the open bite and the incomplete incisor display on smile. After interproximal reduction and retraction and uprighting of the maxillary incisors, the amount of incisor display increased. 278 CHAPTER 9 Special Considerations in Diagnosis and Treatment Planning D E F FIGURE 9-38, cont’d D, Interproximal incisor reshaping and retraction of incisors result in uprighting of the anterior teeth, reduced flare, and increase incisor display on smile.E, The saggi- tal smile demonstrates how uprighting of the maxillary incisor improves the smile arc relationship as well. F, This uprighting also results in closure of the anterior open bite. CHAPTER 9 Special Considerations in Diagnosis and Treatment Planning 279 B A C EG D F FIGURE 9-39 A, This 12-year-old, prior to treatment, had a nice smile with consonant smile arc but short incisal crown height, B, The close-up smile demonstrates the short crown height and slight gingival display on smile. C, Her initial intraoral image reflects the diminished crown height. In order to protect her already ideal smile arc, her brackets were place slightly closer to the gingival margin than standard protocol. D, Nearing completion of treatment, while the smile arc was ideal, the gingival hypertrophy secondary to oral hygiene issues (possibly exacer- bated by the bracket proximity interfering with ideal oral hygiene technique) created periodontal pseudopocketing as well as unaesthetic gingival display and form. -

Facial Deformity With16 Mm Reverse Overjet Treated by Le Fort I & Evro
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 18, Issue 2 Ser. 2 (February. 2019), PP 44-48 www.iosrjournals.org Facial Deformity With16 Mm Reverse Overjet Treated By Le Fort I & Evro: A Pictorial Case Report. 1Dr. (Brig.) Supriyo Roy, 2Dr. (Surg Cdr) Sheosevak Pandey, 3Dr. Ankush Mahajan, 4Dr. Arpita Sahu 1Chief Oral and Maxillofacial Surgeon, Department of Oral and Maxillofacial Surgery, Clove Dental, Delhi NCR. 2Head of Implantology, Department of Oral and Maxillofacial surgery, Clove Dental, Delhi NCR. 3Consultant Oral and Maxillofacial Surgeon, Clove Dental, Delhi NCR. 4Consultant Orthodontist, Clove Dental, Delhi NCR. Corresponding Author: Dr. (Brig.) Supriyo Roy Abstract: Orthognathic Surgery is used to treat mild to severe jaw deformity cases combining orthodontia and oral and maxillofacial surgery to give esthetics, function and stability. Here by we present a severely deformed case with 16 mm reverse overjet requiring bijaw surgery combining le fort I advancement and extra oral vertical ramus osteotomy of mandible for set-back. --------------------------------------------------------------------------------------------------------------------------------------- Date of Submission: 25-01-2019 Date of acceptance: 07-02-2019 --------------------------------------------------------------------------------------------------------------------------------------- I. Introduction Dentofacial deformities and malocclusion are corrected by orthognathic surgery that includes orthodontic and surgical operation of facial skeleton. Correcting malocclusion helps in achieving functional efficiency, structural balance and esthetics.1 Patient with severe malocclusion has compromised physical health, masticatory dysfunction, upper airway resistance, sleep disorders, oral hygiene issues and may also have dysfunctional TMJ.2 Majority of the malocclusion cases have skeletal class III, which are corrected using maxillary advancement, mandibular set back or a combination of both in certain cases. -

Invisalign Treatment Planning Guide 1 Align Technology, Inc
Table of Contents INTRODUCTION . 2 Getting Quality Clinical Outcomes with Invisalign. 2 Invisalign Applicability . 3 DIAGNOSIS AND TREATMENT OPTIONS 1. Crowding . 4 2. Spacing. 10 3. Narrow Arches . 16 4. Crossbite. 20 5. Deep Bite . 24 6. Open Bite . 28 7. Class II . 32 Invisalign 8. Class III . 38 CLINICAL NOTES Treatment IPR . 5 Tooth Size Discrepancy . 11 Planning Staging . 12 Auxiliary Treatment. 12 Guide Expansion . 17 Attachments. 25 Anchorage . 42 APPENDIX Prescription Form Tips. 44 Glossary . 46 Index. 48 Credits . 54 Invisalign Treatment Planning Guide 1 Align Technology, Inc. Introduction HOW TO USE THIS GUIDE Getting Quality Clinical The guide is organized by patient diagnosis. ABOUT THIS GUIDE Match your patient’s diagnosis to the appropriate Outcomes with Invisalign The goal of this guide is to provide you with a diagnosis decision tree to see some possible treat- decision making tool you can use while selecting ment options. Read the accompanying treatment Successful clinical outcomes with Invisalign and treatment planning your Invisalign cases. notes and evaluate your options given your start with attention to detail during case By outlining typically used Invisalign approaches Invisalign experience level. See Figure A, below. selection and treatment planning. Here are and discussing their complexity and predict- five guidelines for setting up your cases that ABOUT THIS SERIES ability, we hope to make the treatment planning pay great dividends later: This guide is the first in a three-part series options and implications more clear for you of Invisalign patient care references, comple- to evaluate. 1. Submit high quality records. Accurate menting the ClinCheck® Evaluation Guide PVS impressions and clear patient photos and (D4458) and the Invisalign Clinical Monitoring Align Technology is not a provider of medical, radiographs are critical for the creation of your Guide (D4219).