A Resolution to the Limitations of Orthodontics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Class III Malocclusion Treated Non-Surgically with Invisalign, Mandibular Fixed Appliances and Mandibular Tads by Randy J
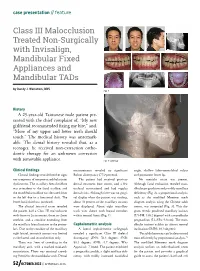
case presentation // feature Class III Malocclusion Treated Non-Surgically with Invisalign, Mandibular Fixed Appliances and Mandibular TADs by Randy J. Weinstein, DDS Fig. 1 History A 25-year-old Taiwanese male patient pre- sented with the chief complaint of, “My new girlfriend recommended fixing my bite,” and, “More of my upper and lower teeth should touch.” The medical history was unremark- able. The dental history revealed that, as a teenager, he received non-extraction ortho- dontic therapy for an unknown correction with removable appliance. Fig. 2: Overlay Clinical findings measurements revealed no significant angle, shallow labio-mentolabial sulcus Clinical findings revealed neither signs Bolton discrepancy (77.9 percent). and prominent lower lip. nor symptoms of temporomandibular joint The patient had received previous No mentalis strain was present. dysfunction. The maxillary dental midline dental treatment (one crown, and a few Although facial evaluation revealed man- was coincident to the facial midline, and occlusal restorations) and had regular dibular prognathism and possibly maxillary the mandibular midline was deviated 2mm dental visits. Although there was no gingi- deficiency (Fig. 2), a proportional analysis, to the left due to a functional shift. The val display when the patient was smiling, such as the modified Moorrees mesh lower facial third was increased. about 70 percent of the maxillary incisors diagram analysis using the Chinese adult The clinical intraoral exam revealed were displayed. About eight maxillary norms, was computed (Fig. 3). This dia- the patient had a Class III malocclusion teeth were shown with buccal corridors gram reveals proclined maxillary incisors with 0mm to 2mm overjet, 0mm to -2mm within normal limits (Fig. -

Treatment Options for Jaw Growth Variations
TREATMENT OPTIONS FOR JAW GROWTH VARIATIONS An Editorial by Robert M. Mason, DMD, PhD PROBLEMS OF OVERGROWTH OF A JAW: It is well known among orthodontists that where there is a growth process involving overgrowth of a jaw, the rule is that growth should be allowed to proceed and then treat the situation after growth has ceased. The reason for this is that growth cannot be effectively stopped or otherwise modified to the extent that jaw growth can be overpowered; that is, “Mother Nature” is smarter than any of us in dentistry. What can be accomplished with an overgrowth of a jaw, however, is orthodontic “remodeling” of some of the parts which are expressing overgrowth. An example is a Class III “growing” mandible. Functional appliances, such as the Frankel or Bionator, can influence the shape of the growing mandible by remodeling, which may give the appearance of manipulating growth, while instead, long-term studies show that such jaw shape changes are only temporary. Over time, the overgrowth pattern returns. Hence, the orthodontic caveat: it is best to let a mandible grow to its full extent and then treat it either by a combination of jaw surgery and orthodontics, or orthodontics alone which may amount to “camouflaging” the problem. What happens dentally in the example of overgrowth of the mandible is that in an attempt for the body to try to maintain dental contacts, the lower incisors tip lingually and the upper incisors tip labially (facially) in an attempt to maintain anterior dental contact relationships as lower jaw growth continues. If the treatment decision is to try to correct the problem with orthodontics alone, Class III elastics would be used along with orthodontic fixed appliances to maintain the lingual tipping and maxillary flaring of incisors. -

An Overview on Interproximal Enamel Reduction
DENTISTRY ISSN 2377-1623 http://dx.doi.org/10.17140/DOJ-1-104 Open Journal Review An Overview on Interproximal Enamel *Corresponding author Reduction Yanqi Yang Assistant Professor in Orthodontics Faculty of Dentistry, the University of Deborah Chee#, Chong Ren# and Yanqi Yang* Hong Kong, 2/F, Prince Philip Dental Hospital, 34 Hospital Road, Sai Ying #equally contributed Pun, Hong Kong, China Tel. +852-28590252 Orthodontics, Faculty of Dentistry, the University of Hong Kong, 34 Hospital Road, Hong Kong Fax: +852-25593803 SAR, China E-mail: [email protected] Volume 1 : Issue 1 ABSTRACT Article Ref. #: 1000DOJ1104 Ever since its first introduction seven decades ago, there has been continuous advance- ment of the concept and technique of Interproximal enamel reduction (IPR). It’s demonstrated Article History that with correct case selection and clinical performance, IPR is safe and effective for alleviat- Received: October 28th, 2014 ing crowding, improving dental and gingival aesthetics as well as facilitating post-treatment Accepted: December 5th, 2014 stability. The fulfilment of treatment outcomes depends on careful pre-treatment examination Published: December 8th, 2014 and planning, appropriate clinical procedures and effective post-treatment protection. This re- view aims to provide a general introduction to IPR in terms of its history background, risks and Citation benefits and clinical performance. Chee D, Ren C, Yang Y. An overview on interproximal enamel reduction. Dent Open J. 2014; 1(1): 14-18. doi: KEYWORDS: Interproximal enamel reduction; Orthodontic treatment; Crowding; Tooth re- 10.17140/DOJ-1-104 contouring. INTRODUCTION Interproximal enamel reduction (IPR) also described as “stripping”, “reproximation” and “slenderizing” has been applied in clinical orthodontics for almost seven decades.1,2 By removing part of the enamel tissue from the interproximal contact area, this technique has been proved to be effective in improving dental alignment, stability and aesthetics. -

Elastics and Elastomeric in Orthodontics Practice REVIEW ARTICLE
IJPCDR Elastics and Elastomeric in Orthodontics Practice REVIEW ARTICLE Elastics and Elastomeric in Orthodontics Practice 1Sagar Mapare, 2Kanish Bansal, 3Ranjit Pawar, 4Richa Mishra, 5Ashutosh Sthapak, 6Sayed F Khadri ABSTRACT provides the clinician with the ability to correct both Elastics and elastomeric are an important part of orthodontic anteroposterior and vertical discrepancies. treatment with patients’ cooperation; they are used for Both natural rubber and synthetic elastomers are correction of anteroposterior and vertical discrepancies; there widely used in orthodontic therapy. Naturally produced are many types of elastics placement in relation with treatment latex elastics are used in the Begg technique to provide requirements. Elastics can be classified in many ways: intermaxillary traction and intramaxillary forces. Syn- according to the material, their availability, their uses, and force. Elastomer is a general term that encompasses materials that, thetic elastomeric materials in the form of chains find their after substantial deformation, rapidly return to their original greatest application with edgewise mechanics where they dimensions. Natural rubber is the first known elastomeric, are used to move the teeth along the arch wire. used by the ancient Incan and Mayan civilizations. Rubber-like The links of chain fit firmly under the wings of an materials that are made from chemicals were called synthetic edgewise bracket so that chain elastomers also serve to rubber because they were intended as substitutes for natural rubber. replace metal as the ligating force that holds the arch The types of elastic based on their use are class I, II, III, wire to the teeth. Since they are so positively located on palatal, lingual, cross, etc. -

Orthodontics & Esthetic Dentistry
SCIENTIFIC SESSION TORONTO 2016 ORTHODONTICS & ESTHETIC DENTISTRY: MISSION POSSIBLE! A Broader Approach to Interdisciplinary Esthetic Treatment David M. Sarver, DMD, MS AACD 2016 TORONTO: THURSDAY MORNING “TRIPLE PLAY!” One Session. One Theme. Three Big Hitters. Dr. David M. Sarver, along with Dr. J. William Robbins and Dr. Jeffrey Rouse, will “cover the bases” on diagnosis, decision making, and treatment planning. These three “big hitters” will be presenting sequentially in the same room on Thursday, April 28, 2016. Dr. Sarver will present “Orthodontics— How it Has Changed and What You Really Want to Know!” This article discusses how orthodontics is incorporating smile design principles into its overall functional and esthetic treatment goals. Abstract For decades, dentistry has been evolving into a Patients seeking esthetic profession that is extremely multifaceted and varied in its approach to both smile and facial esthetics. treatment today wish to The coordination of macro esthetics (the face), mini enhance their appearance esthetics (the smile), and micro esthetics (the dental for improved self-esteem esthetic component) offers a complete approach to esthetic planning. This article presents an expanded and quality of life. vision of esthetic treatment designed to take readers to another level of facial, smile, and dental esthetic planning that can elevate patient outcomes. Key Words: macro esthetics, mini esthetics, micro esthetics, orthodontics, smile design 14 Winter 2016 • Volume 31 • Number 4 Sarver Figure 1: In both multidisciplinary and orthodontic diagnosis, three esthetic divisions are advocated: macro esthetics (the face), mini esthetics (the smile), and micro esthetics (the teeth). …there are principles of cosmetic dentistry that orthodontists can use to enhance their work to provide a superior esthetic outcome. -

Non-Surgical Treatment of an Adult Class III Malocclusion Patient with Facial Asymmetry by Unilateral Mandibular Arch Distalization
Volume 29 Issue 2 Article 4 2017 Non-surgical Treatment of an Adult Class III Malocclusion Patient with Facial Asymmetry by Unilateral Mandibular Arch Distalization Chi-Yu Tsai Department of Orthodontics, Kaohsiung Chang Gung Memorial Hospital, Chang Gung University College of Medicine, Kaohsiung, Taiwan Shiu-Shiung Lin Department of Orthodontics, Kaohsiung Chang Gung Memorial Hospital, Chang Gung University College of Medicine, Kaohsiung, Taiwan Yi-Hao Lee Department of Orthodontics, Kaohsiung Chang Gung Memorial Hospital, Chang Gung University College of Medicine, Kaohsiung, Taiwan Li-Tyng Sun Department of Orthodontics, Kaohsiung Chang Gung Memorial Hospital, Chang Gung University College of Medicine, Kaohsiung, Taiwan Yu-Jen Chang Department of Orthodontics, Kaohsiung Chang Gung Memorial Hospital, Chang Gung University College Fofollow Medicine, this and Kaohsiung, additional T aiwanworks at: https://www.tjo.org.tw/tjo Part of the Orthodontics and Orthodontology Commons See next page for additional authors Recommended Citation Tsai, Chi-Yu; Lin, Shiu-Shiung; Lee, Yi-Hao; Sun, Li-Tyng; Chang, Yu-Jen; and Wu, Te-Ju (2017) "Non-surgical Treatment of an Adult Class III Malocclusion Patient with Facial Asymmetry by Unilateral Mandibular Arch Distalization," Taiwanese Journal of Orthodontics: Vol. 29 : Iss. 2 , Article 4. DOI: 10.30036/TJO.201706_29(2).0004 Available at: https://www.tjo.org.tw/tjo/vol29/iss2/4 This Case Report is brought to you for free and open access by Taiwanese Journal of Orthodontics. It has been accepted for inclusion -

An Overview on Interproximal Enamel Reduction Review
DENTISTRY ISSN 2377-1623 http://dx.doi.org/10.17140/DOJ-1-104 Open Journal Review An Overview on Interproximal Enamel *Corresponding author Reduction Yanqi Yang Assistant Professor in Orthodontics Faculty of Dentistry, the University of Deborah Chee#, Chong Ren# and Yanqi Yang* Hong Kong, 2/F, Prince Philip Dental Hospital, 34 Hospital Road, Sai Ying #equally contributed Pun, Hong Kong, China Tel. +852-28590252 Orthodontics, Faculty of Dentistry, the University of Hong Kong, 34 Hospital Road, Hong Kong Fax: +852-25593803 SAR, China E-mail: [email protected] Volume 1 : Issue 1 ABSTRACT Article Ref. #: 1000DOJ1104 Ever since its first introduction seven decades ago, there has been continuous advance- ment of the concept and technique of Interproximal enamel reduction (IPR). It’s demonstrated Article History that with correct case selection and clinical performance, IPR is safe and effective for alleviat- Received: October 28th, 2014 ing crowding, improving dental and gingival aesthetics as well as facilitating post-treatment Accepted: December 5th, 2014 stability. The fulfilment of treatment outcomes depends on careful pre-treatment examination Published: December 8th, 2014 and planning, appropriate clinical procedures and effective post-treatment protection. This re- view aims to provide a general introduction to IPR in terms of its history background, risks and Citation benefits and clinical performance. Chee D, Ren C, Yang Y. An overview on interproximal enamel reduction. Dent Open J. 2014; 1(1): 14-18. doi: KEYWORDS: Interproximal enamel reduction; Orthodontic treatment; Crowding; Tooth re- 10.17140/DOJ-1-104 contouring. INTRODUCTION Interproximal enamel reduction (IPR) also described as “stripping”, “reproximation” and “slenderizing” has been applied in clinical orthodontics for almost seven decades.1,2 By removing part of the enamel tissue from the interproximal contact area, this technique has been proved to be effective in improving dental alignment, stability and aesthetics. -

Orthodontic Treatment of a Patient with Duchenne Muscular Dystrophy and Macroglossia: How Informed Consent Was Critical to Success
CASE REPORT Orthodontic treatment of a patient with Duchenne muscular dystrophy and macroglossia: How informed consent was critical to success James R. Miller Golden Valley and Minneapolis, Minn This article describes the complex orthodontic treatment of a 22-year-old patient with Duchenne muscular dys- trophy and macroglossia. His orthodontic treatment hinged on providing proper informed consent and manage- ment of the malocclusion with glossectomy, extractions, fixed appliances, and elastics. Challenges to traditional treatment are outlined, and compromises to both process and outcome are discussed from an informed consent point of view because of the serious risks involved. The treatment objectives were met, and the outcome was considered a success. (Am J Orthod Dentofacial Orthop 2013;144:890-8) he purpose of this article is to describe the ortho- past medical history was remarkable for Duchenne Tdontic treatment of a 22-year-old man with muscular dystrophy and an allergy to Augmentin. He Duchenne muscular dystrophy and macroglossia. did not have a tracheostomy tube. He was unable to He used a power wheelchair that he controlled with a voluntarily lift his arms and relied on caregivers for joystick, and some aspects of diagnosis and treatment oral hygiene. The clinical examination and initial photo- were adapted to address his needs and abilities. I report graphic montage (Fig 1) in full occlusion showed gener- here the treatment we provided, including the compro- alized excessive buccal crown torque with an anterior mises that were made and the problems that arose. I open bite of 8 to 10 mm and a posterior open bite of discuss the patient's treatment based on his wishes 0 to 12 mm. -

Movingnot Removing Enamel
VOLUME 01 / ISSUE 01 The Academy for Clear Aligner Therapy the AmericanJournal Academy of Cosmetic Orthodontics MOVING not removing ENAMEL. PEER-REVIEWED SOLUTIONS that will make Clear Aligner Treatment THAT MUCH EASIER. Like this Journal? start receiving your quarterly issue today! The official academy for Clear Aligner Therapy. Become a member TODAY! www.aacortho.com AACO Board Members Dr. David Galler: President the Dr. Mark Hodge: Vice President Dr. Perry Jones: Director of Education Dr. Jeffrey Galler: Editor AmericanJournal Academy of Cosmetic Orthodontics Dr. Len Tau: Director of Media Relations Dr. Bruce McFarlane: Orthodontist, Advisory Board Article is Peer Reviewed Article offers CE Credit at www.aacortho.com Dr. David Harrnick: Orthodontist, Advisory Board Dr. Sandi Bosin: Orthodontist, Editorial Board Case Reports Dr. Peter Rivolli: ClearCorrect Clinical Expert Dr. Yana Shampanksy: Invisalign Expert 2 Upper Lateral Incisor Crossbite with Dr. Lori Trost: MTM Clinical Expert Lower Premolar in Lingual Version by Dr. Cathy Sherry 4 Invisalign Correction of a Teenager’s Class 2 Division 1 Malocclusion by Dr. David J. Harnick 8 Upper Arch Spacing and Lower Editorial Arch Overcrowding I’ve been reading numerous by Dr. David Galler dental journals every Practice Development month for many years, 14 The Economics of Buying vs. but don’t remember ever Renting Your Next Office actually reading an editorial completely, from beginning by Jake Jacklich to end. 16 “Doctor, I’ve been your patient for I resolved that in this, my first 10 years; how come you never editorial for the Journal of the American mentioned orthodontics before?” Academy of Cosmetic Orthodontics, by Gary Kadi I would write an editorial that readers Retention would, in fact, read from the very first to the very last word. -

Orthodontic Treatment of Class Three Malocclusion Using Clear Aligners
Journal of Oral Biology and Craniofacial Research 9 (2019) 360–362 Contents lists available at ScienceDirect Journal of Oral Biology and Craniofacial Research journal homepage: www.elsevier.com/locate/jobcr Case study Orthodontic treatment of class three malocclusion using clear aligners: A case report T ∗ Edoardo Staderini , Simonetta Meuli, Patrizia Gallenzi Institute of Dentistry and Maxillofacial Surgery, Fondazione Policlinico Universitario A. Gemelli IRCCS, Università Cattolica del Sacro Cuore, Largo A, Gemelli N°1, Rome, RM, 00168, Italy ARTICLE INFO ABSTRACT Keywords: Class III malocclusion is a growth-related challenging condition for orthodontists. We present a case of a 11-year- Angle class III old girl with a skeletal class III malocclusion with bilateral cross bite, and a functional shift of the lower dental Clear aligner midline. A multiphase clear aligners' treatment was scheduled with the aim of removing all dental interferences Interceptive orthodontic treatment which involved an anterior displacement of the mandible. At one-year follow-up, clear aligners’ therapy resulted in skeletal and dental improvements. Clear aligners therapy represents a valid alternative to fixed appliance therapy in the early interception of class III malocclusion. The present manuscript was prepared following the CARE guidelines. 1. Introduction relation was noticed.4 At intraoral evaluation, the patient presented a late mixed dentition with a bilateral class III malocclusion, along with a Class III malocclusion is a challenging dentoalveolar growth defor- functional mandibular lateral deviation towards the patient's left side, mity, affecting between 5.5% and 19.4% of the population.1 Early without any sign or symptom of temporomandibular joint disorders. -
3D Airway Changes Using CBCT in Patients Following Mandibular Setback Surgery ± Maxillary Advancement
Received: 5 December 2018 | Accepted: 7 December 2018 DOI: 10.1111/ocr.12291 SUPPLEMENT ARTICLE 3D Airway changes using CBCT in patients following mandibular setback surgery ± maxillary advancement Andrew G. Havron1 | Sharon Aronovich2 | Anita V. Shelgikar3 | H. Ludia Kim4 | R. Scott Conley5 1Department of Orthodontics and Pediatric Dentistry, University of Michigan, Ann Structured Abstract Arbor, Michigan Introduction: The aim of this study was to determine the 3D airway changes that 2 Department of Oral and Maxillofacial occur following mandibular setback surgery alone vs bimaxillary surgery in patients Surgery, University of Michigan, Ann Arbor, Michigan with similar skeletal start forms. 3Department of Neurology, University of Setting and Sample Population: The University of Michigan School of Dentistry and Michigan, Ann Arbor, Michigan Medical Center. A total of 85 patients undergoing mandibular setback with or with- 4Private Practice, Ann Arbor, Michigan out simultaneous maxillary advancement. 5Department of Orthodontics, University at Buffalo, Buffalo, New York Materials and Methods: A retrospective evaluation of pre- and post- surgical CBCT scans for patients undergoing mandibular setback surgery alone (14) vs bimaxillary Correspondence R. Scott Conley, University at Buffalo School surgery (71) was performed. Cross- sectional evaluation at standardized locations, of Dental Medicine, Buffalo, NY. minimum cross section and volumetric analysis were performed (Dolphin Imaging & Email: [email protected] Management Solutions). Results: Patients who underwent mandibular setback surgery alone showed a statis- tically significant average increase of 47.5 mm2 in minimum axial area. Patients who underwent bimaxillary surgery showed a statistically significant increase in airway volume, minimum axial area, location of minimum axial area, and axial area at the re- tropalatal and retroglossal regions. -

Journal of Cosmetic Dentistry
Journal of Cosmetic Dentistry Rubber Dam First Calin Pop, DDS Analysis with Imaging & Photography Conservative Composite Bonding 2020 VOLUME 36 ISSUE 3 “We asked, they delivered!” Based on AACD members’ feedback, Ivoclar Vivadent developed a NEW Higher Viscocity Veneer Cement. Amanda Seay, DDS, FAACD INTRODUCING Variolink® Esthetic LC HV Higher viscosity light curing cement • Controlled seating GET YOUR FREE REFILL AT • Precise cleanup blog.ivoclarvivadent.us/free-variolink-sample • Ideal for veneers ivoclarvivadent.com For more information, call us at 1-800-533-6825 in the U.S., 1-800-263-8182 in Canada. © 2020 Ivoclar Vivadent, Inc. Ivoclar Vivadent and Variolink are registered trademarks of Ivoclar Vivadent, Inc. 13722_VE LC HV_JCD.indd 1 11/3/20 3:51 PM A PEER-REVIEWED PUBLICATION OF THE AMERICAN ACADEMY OF COSMETIC DENTISTRY EDITORIAL REVIEW BOARD Pinhas Adar, MDT, CDT, Atlanta, GA Irfan Ahmad, BDS, Middlesex, United Kingdom Somkiat Aimplee, DDS, MSc, AAACD, Bangkok, Thailand volume 36 issue 3 Gary Alex, DMD, AAACD, Huntington, NY Journal of Cosmetic Dentistry Edward P. Allen, DDS, PhD, Dallas, TX Chad J. Anderson, DMD, MS, Fresno, CA Elizabeth M. Bakeman, DDS, FAACD, Grand Rapids, MI Lee Ann Brady, DMD, Glendale, AZ Kevin M. Brown, DDS, AAACD, Bellevue, WA Ricardo M. Carvalho, DDS, PhD, Vancouver, BC, Canada EDITOR-IN-CHIEF Edward Lowe, DMD, AAACD Christian Coachman, DDS, CDT, Sáo Paulo, Brazil Vancouver, BC, Canada, [email protected] John C. Cranham, DDS, Chesapeake, VA EXECUTIVE DIRECTOR Barbara J. Kachelski, MBA, CAE, [email protected] Michael W. Davis, DDS, Santa Fe, NM Newton Fahl Jr., DDS, MS, Curitiba-PR, Brazil CHIEF MARKETING OFFICER Mike DiFrisco, CAE, [email protected] Jonathan L.