Soft Tissue Surgeries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Unit Price Base Price Service Type Procedure
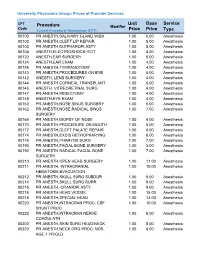
University Physicians Group: Prices of Provider Services CPT Unit Base Service Procedure Modifier Code ype Current Procedural Terminology (CPT) Price Price T 00100 PR ANESTH,SALIVARY GLAND W/BX 1.00 5.00 Anesthesia 00102 PR ANESTH,CLEFT LIP REPAIR 1.00 6.00 Anesthesia 00103 PR ANESTH,BLEPHAROPLASTY 1.00 5.00 Anesthesia 00104 ANESTH,ELECTROSHOCK/ ECT 1.00 4.00 Anesthesia 00120 ANESTH,EAR SURGERY 1.00 5.00 Anesthesia 00124 ANESTH,EAR EXAM 1.00 4.00 Anesthesia 00126 PR ANESTH,TYMPANOTOMY 1.00 4.00 Anesthesia 00140 PR ANESTH,PROCEDURES ON EYE 1.00 5.00 Anesthesia 00142 ANESTH, LENS SURGERY 1.00 4.00 Anesthesia 00144 PR ANESTH,CORNEAL TRANSPLANT 1.00 6.00 Anesthesia 00145 ANESTH, VITREORETINAL SURG 1.00 6.00 Anesthesia 00147 PR ANESTH,IRIDECTOMY 1.00 4.00 Anesthesia 00148 ANESTH,EYE EXAM 1.00 4.00 Anesthesia 00160 PR ANESTH,NOSE,SINUS SURGERY 1.00 5.00 Anesthesia 00162 PR ANESTH,NOSE,RADICAL SINUS 1.00 7.00 Anesthesia SURGERY 00164 PR ANESTH,BIOPSY OF NOSE 1.00 4.00 Anesthesia 00170 PR ANESTH,PROCEDURE ON MOUTH 1.00 5.00 Anesthesia 00172 PR ANESTH,CLEFT PALATE REPAIR 1.00 6.00 Anesthesia 00174 PR ANESTH,EXCIS RETROPHARYNG 1.00 6.00 Anesthesia 00176 PR ANESTH,PHARYNX SURG 1.00 7.00 Anesthesia 00190 PR ANESTH,FACIAL BONE SURGERY 1.00 5.00 Anesthesia 00192 PR ANESTH,RADICAL FACIAL BONE 1.00 7.00 Anesthesia SURGERY 00210 PR ANESTH,OPEN HEAD SURGERY 1.00 11.00 Anesthesia 00211 PR ANESTH, INTRACRANIAL 1.00 10.00 Anesthesia HEMATOMA EVACUATION 00212 PR ANESTH,SKULL SURG SUBDUR 1.00 5.00 Anesthesia 00214 PR ANESTH,SKULL SURG BURR 1.00 9.00 Anesthesia -

Code Procedure Cpt Price University Physicians Group
UNIVERSITY PHYSICIANS GROUP (UPG) PRICES OF PROVIDER SERVICES CODE PROCEDURE MOD CPT PRICE 0001A IMM ADMN SARSCOV2 30MCG/0.3ML DIL RECON 1ST DOSE 0001A $40.00 0002A IMM ADMN SARSCOV2 30MCG/0.3ML DIL RECON 2ND DOSE 0002A $40.00 0011A IMM ADMN SARSCOV2 100 MCG/0.5 ML 1ST DOSE 0011A $40.00 0012A IMM ADMN SARSCOV2 100 MCG/0.5 ML 2ND DOSE 0012A $40.00 0021A IMM ADMN SARSCOV2 5X1010 VP/0.5 ML 1ST DOSE 0021A $40.00 0022A IMM ADMN SARSCOV2 5X1010 VP/0.5 ML 2ND DOSE 0022A $40.00 0031A IMM ADMN SARSCOV2 AD26 5X10^10 VP/0.5 ML 1 DOSE 0031A $40.00 0042T CEREBRAL PERFUS ANALYSIS, CT W/CONTRAST 0042T $954.00 0054T BONE SURGERY USING COMPUTER ASSIST, FLURO GUIDED 0054T $640.00 0055T BONE SURGERY USING COMPUTER ASSIST, CT/ MRI GUIDED 0055T $1,188.00 0071T U/S LEIOMYOMATA ABLATE <200 CC 0071T $2,500.00 0075T 0075T PR TCAT PLMT XTRC VRT CRTD STENT RS&I PRQ 1ST VSL 26 26 $2,208.00 0126T CAROTID INT-MEDIA THICKNESS EVAL FOR ATHERSCLER 0126T $55.00 0159T 0159T COMPUTER AIDED BREAST MRI 26 26 $314.00 PR RECTAL TUMOR EXCISION, TRANSANAL ENDOSCOPIC 0184T MICROSURGICAL, FULL THICK 0184T $2,315.00 0191T PR ANT SEGMENT INSERTION DRAINAGE W/O RESERVOIR INT 0191T $2,396.00 01967 ANESTH, NEURAXIAL LABOR, PLAN VAG DEL 01967 $2,500.00 01996 PR DAILY MGMT,EPIDUR/SUBARACH CONT DRUG ADM 01996 $285.00 PR PERQ SAC AGMNTJ UNI W/WO BALO/MCHNL DEV 1/> 0200T NDL 0200T $5,106.00 PR PERQ SAC AGMNTJ BI W/WO BALO/MCHNL DEV 2/> 0201T NDLS 0201T $9,446.00 PR INJECT PLATELET RICH PLASMA W/IMG 0232T HARVEST/PREPARATOIN 0232T $1,509.00 0234T PR TRANSLUMINAL PERIPHERAL ATHERECTOMY, RENAL -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

FLEXOR TENOTOMY: a Simplified Technique
CHAPTER 1 FLEXOR TENOTOMY: A Simplified Technique Mickey D. Stapp, DPM Craig Camasta, DPM INTRODUCTION The key to choosing this procedure is that the digital deformity must be flexible or semi-rigid at the interpha - Tenotomies have been performed in foot and ankle langeal joint level and no contracture or a reducible surgeries for many years. Traditionally, open tenotomies deformity at the metatarsophalangeal joint level. This were performed alone, in significant tendon contractures procedure cannot serve as an alternative for an arthrodesis without osseous involvement, or in combination with or arthroplasty of the digit or a full sequential release at the osseous surgery when osseous changes were also present. metatarsophalangeal joint. A percutaneous tenotomy for Many foot and ankle surgeons have understood the flexible digital deformities would be rarely indicated for importance of tenotomies in successful digital surgeries. 1-4 multiple adjacent digits. It is most often utilized on third McGowan may have been first to describe a minimally and fourth toes. invasive technique for tenotomies. 5 The lesion pattern, hyperkeratotic, preulcerative, or Surgeons searching for less invasive procedures to full ulcer, must be taken into consideration. The majority address tendon pathology began utilizing percutaneous of lesions best amenable to this procedure are lesions tenotomies for a multitude of various foot and ankle located at the distal aspect of the digit. This procedure deformities. The vast majority of these have been described provides a simplified technique to eliminate painful distal for clubfoot deformities. 6-8 Prior to the use of percutaneous clavi or recurring ulcerative lesions (Figure 1). tenotomies in clubfoot surgery, this technique was described for various Achilles tendonopathies. -

1 Annex 2. AHRQ ICD-9 Procedure Codes 0044 PROC-VESSEL
Annex 2. AHRQ ICD-9 Procedure Codes 0044 PROC-VESSEL BIFURCATION OCT06- 0201 LINEAR CRANIECTOMY 0050 IMPL CRT PACEMAKER SYS 0202 ELEVATE SKULL FX FRAGMNT 0051 IMPL CRT DEFIBRILLAT SYS 0203 SKULL FLAP FORMATION 0052 IMP/REP LEAD LF VEN SYS 0204 BONE GRAFT TO SKULL 0053 IMP/REP CRT PACEMAKR GEN 0205 SKULL PLATE INSERTION 0054 IMP/REP CRT DEFIB GENAT 0206 CRANIAL OSTEOPLASTY NEC 0056 INS/REP IMPL SENSOR LEAD OCT06- 0207 SKULL PLATE REMOVAL 0057 IMP/REP SUBCUE CARD DEV OCT06- 0211 SIMPLE SUTURE OF DURA 0061 PERC ANGIO PRECEREB VES (OCT 04) 0212 BRAIN MENINGE REPAIR NEC 0062 PERC ANGIO INTRACRAN VES (OCT 04) 0213 MENINGE VESSEL LIGATION 0066 PTCA OR CORONARY ATHER OCT05- 0214 CHOROID PLEXECTOMY 0070 REV HIP REPL-ACETAB/FEM OCT05- 022 VENTRICULOSTOMY 0071 REV HIP REPL-ACETAB COMP OCT05- 0231 VENTRICL SHUNT-HEAD/NECK 0072 REV HIP REPL-FEM COMP OCT05- 0232 VENTRI SHUNT-CIRCULA SYS 0073 REV HIP REPL-LINER/HEAD OCT05- 0233 VENTRICL SHUNT-THORAX 0074 HIP REPL SURF-METAL/POLY OCT05- 0234 VENTRICL SHUNT-ABDOMEN 0075 HIP REP SURF-METAL/METAL OCT05- 0235 VENTRI SHUNT-UNINARY SYS 0076 HIP REP SURF-CERMC/CERMC OCT05- 0239 OTHER VENTRICULAR SHUNT 0077 HIP REPL SURF-CERMC/POLY OCT06- 0242 REPLACE VENTRICLE SHUNT 0080 REV KNEE REPLACEMT-TOTAL OCT05- 0243 REMOVE VENTRICLE SHUNT 0081 REV KNEE REPL-TIBIA COMP OCT05- 0291 LYSIS CORTICAL ADHESION 0082 REV KNEE REPL-FEMUR COMP OCT05- 0292 BRAIN REPAIR 0083 REV KNEE REPLACE-PATELLA OCT05- 0293 IMPLANT BRAIN STIMULATOR 0084 REV KNEE REPL-TIBIA LIN OCT05- 0294 INSERT/REPLAC SKULL TONG 0085 RESRF HIPTOTAL-ACET/FEM -

Ipo) List for Cy 2021 (N=266)
TABLE 31: PROPOSED MUSCULOSKELETAL-RELATED SERVICE REMOVALS FROM THE INPATIENT ONLY (IPO) LIST FOR CY 2021 (N=266) CY CY 2020 Long Descriptor Related Proposed Proposed 2020 Services CY 2021 CY 2021 CPT OPPS OPPS APC Code Status Assignment Indicator 0095T Removal of total disc arthroplasty 22856 N/A (artificial disc), anterior approach, each additional interspace, cervical (list separately in addition to code for primary procedure) 0098T Revision including replacement 22858 N/A of total disc arthroplasty (artificial disc), anterior approach, each additional interspace, cervical (list separately in addition to code for primary procedure) 0163T Total disc arthroplasty (artificial 22858 N/A disc), anterior approach, including discectomy to prepare interspace (other than for decompression), each additional interspace, lumbar (list separately in addition to code for primary procedure) 0164T Removal of total disc 22856 N/A arthroplasty, (artificial disc), anterior approach, each additional interspace, lumbar (list separately in addition to code for primary procedure) 0165T Revision including replacement 22858 N/A of total disc arthroplasty (artificial disc), anterior approach, each additional interspace, lumbar (list separately in addition to code for primary procedure) 0202T Posterior vertebral joint(s) 63030 J1 5115 arthroplasty (for example, facet joint[s] replacement), including facetectomy, laminectomy, foraminotomy, and vertebral column fixation, injection of bone cement, when performed, including fluoroscopy, single level, lumbar spine -

Approved Surgical Procedures
UNION MEDICAL BENEFITS SOCIETY LTD APPROVED SURGICAL PROCEDURES The following list of surgical procedures should be read in conjunction with your policy document. If you are intending to have one of the listed procedures, please call our surgical team on 0800 600 666 so we can guide you through the prior approval process. If a surgical procedure is not listed below, it will not be covered unless UniMed decides, in its sole discretion, to offer cover. CARDIAC GENERAL • Pericardiotomy Breast • Pericardiocentesis • Breast Cyst Aspiration or Needle Biopsy • Drainage of Pericaridal Effusion • Breast Biopsy • Coronary Artery Bypass (using vein or artery) • Core Biopsy of Breast • Open Repair of Atrial Septal Defect (ASD) • Excision Accessary Breast Tissue • Valvuloplasty • Mastectomy • Aortic/ Mitral Valve Replacement via Sternotomy • Sentinel Node Biopsy with/without Axillary Dissection • Pulmonary Valve Replacement via Sternotomy • Breast Microdochotomy • Tricuspid Valve Replacement via Sternotomy • Balloon Valvuloplasty – Mitral/ Aortic Reconstruction Post Mastectomy • Pacemaker Surgery – Initial Implantation (Excluding the Cost • Breast/ Nipple Reconstruction of the Pacemaker) • Nipple Areolar Tattoo • Removal of Sternal Wire • Maze Arrhythmia Surgery Gastrointestinal • Removal & Rewiring of Sternal Wire • Anal Sphincterotomy • Maze Arrhythmia Surgery (Standalone procedure) • Simple Repair of Anal Fistula – Special approval only • Maze Procedure – Thoracoscopic • Anal Fistula Repair with Mucosal Advancement Flap • Bentall’s Procedure (includes -

NOMESCO Classification of Surgical Procedures
NOMESCO Classification of Surgical Procedures NOMESCO Classification of Surgical Procedures 87:2009 Nordic Medico-Statistical Committee (NOMESCO) NOMESCO Classification of Surgical Procedures (NCSP), version 1.14 Organization in charge of NCSP maintenance and updating: Nordic Centre for Classifications in Health Care WHO Collaborating Centre for the Family of International Classifications in the Nordic Countries Norwegian Directorate of Health PO Box 700 St. Olavs plass 0130 Oslo, Norway Phone: +47 24 16 31 50 Fax: +47 24 16 30 16 E-mail: [email protected] Website: www.nordclass.org Centre staff responsible for NCSP maintenance and updating: Arnt Ole Ree, Centre Head Glen Thorsen, Trine Fresvig, Expert Advisers on NCSP Nordic Reference Group for Classification Matters: Denmark: Søren Bang, Ole B. Larsen, Solvejg Bang, Danish National Board of Health Finland: Jorma Komulainen, Matti Mäkelä, National Institute for Health and Welfare Iceland: Lilja Sigrun Jonsdottir, Directorate of Health, Statistics Iceland Norway: Øystein Hebnes, Trine Fresvig, Glen Thorsen, KITH, Norwegian Centre for Informatics in Health and Social Care Sweden: Lars Berg, Gunnar Henriksson, Olafr Steinum, Annika Näslund, National Board of Health and Welfare Nordic Centre: Arnt Ole Ree, Lars Age Johansson, Olafr Steinum, Glen Thorsen, Trine Fresvig © Nordic Medico-Statistical Committee (NOMESCO) 2009 Islands Brygge 67, DK-2300 Copenhagen Ø Phone: +45 72 22 76 25 Fax: +45 32 95 54 70 E-mail: [email protected] Cover by: Sistersbrandts Designstue, Copenhagen Printed by: AN:sats - Tryk & Design a-s, Copenhagen 2008 ISBN 978-87-89702-69-8 PREFACE Preface to NOMESCO Classification of Surgical Procedures Version 1.14 The Nordic Medico-Statistical Committee (NOMESCO) published the first printed edition of the NOMESCO Classification of Surgical Procedures (NCSP) in 1996. -

Procedure Codes Payable As an Inpatient Service When Delivered In
INDIANA HEALTH COVER A G E PROGRAMS PROVIDER CO D E S E T S Procedure codes payable as an inpatient service when delivered in an inpatient setting for stays of less than 24 hours for DOS on or after July 1, 2014 Procedure Description Code 11005 Debridement of skin, subcutaneous tissue, muscle and fascia for necrotizing soft tissue infection; abdominal wall, with or without fascial closure 11008 Removal of prosthetic material or mesh, abdominal wall for infection (eg, for chronic or recurrent mesh infection or necrotizing soft tissue infection) (list separately in addition to code for primary procedure) 19361 Breast reconstruction with latissimus dorsi flap, without prosthetic implant 21343 Open treatment of depressed frontal sinus fracture 21422 Treatment of palatal or alveolar ridge fractures (Lefort I type); open treatment 22532 Arthrodesis, lateral extracavitary technique, including minimal diskectomy to prepare interspace (other than for decompression); thoracic 22558 Arthrodesis, anterior interbody technique; lumbar, with bone graft 22585 Arthrodesis, ant or antitrl, ea additional interspace (list sep in add to single lvl arthrodesis) 22842 Posterior segmental instrumentation (eg, pedicle fixation, dual rods with multiple hooks and sublaminar wires); 3 to 6 vertebral segments (list separately in addition to code for primary procedure) 27025 Ober-yount fasciotomy, combined with spica cast, pins in tibia, wedging the cast, etc; unilateral 27450 Osteotomy, femur, shaft or supracondylar, with fixation; unilateral 27472 Repair, nonunion -
Procedure Codes Section 5
NEW YORK STATE MEDICAID PROGRAM PHYSICIAN – PROCEDURE CODES SECTION 5 - SURGERY Physician – Procedure Codes, Section 5 - Surgery _____________________________________________________________________________ Table of Contents ANESTHESIA SECTION------------------------------------------------------------------------2 GENERAL INFORMATION AND RULES------------------------------------------------2 CALCULATION OF TOTAL ANESTHESIA VALUES --------------------------------4 SURGERY SECTION ----------------------------------------------------------------------------5 GENERAL INFORMATION AND RULES------------------------------------------------5 SURGERY SERVICES ------------------------------------------------------------------------ 11 GENERAL -------------------------------------------------------------------------------------- 11 INTERGUMENTARY SYSTEM ----------------------------------------------------------- 11 MUSCULOSKELETAL SYSTEM--------------------------------------------------------- 38 RESPIRATORY SYSTEM ---------------------------------------------------------------- 108 CARDIOVASCULAR SYSTEM --------------------------------------------------------- 123 HEMIC AND LYMPHATIC SYSTEMS ------------------------------------------------ 167 MEDIASTINUM AND DIAPHRAGM --------------------------------------------------- 170 DIGESTIVE SYSTEM---------------------------------------------------------------------- 171 URINARY SYSTEM ------------------------------------------------------------------------ 214 MALE GENITAL SYSTEM --------------------------------------------------------------- -

CPT Codes Requiring Prior Authorization
CPT Codes Requiring Prior Authorization NOTE: To validate coverage by site of service, please reference the appropriate Appendices below. Services not designated as a covered service in the applicable Appendix, based on the location and type of service, are not reimbursable in accordance with the Ohio Administrative Code rules, unless prior authorization is obtained. Prior authorization is always required for non-covered or non-grouper surgical codes (codes not listed in the Appendices designated for the site of service). DISCLAIMER: Prior Authorization is not required for office-based surgical procedures, except for those listed below: • Cosmetic, plastic, and reconstructive procedures • Experimental/investigational procedures • Services performed by podiatrists • Pain management procedures • Unlisted/miscellaneous procedures Site of Service Appendix Ohio Administrative Code (OAC) Physician Services Appendix DD 5160-1-60 Ambulatory Surgical Centers Appendix DD 5160-22-03 (These codes are noted in the “Current ASC Group” column of the Medicaid Fee Schedule, Appendix DD. Please reference ASC Facility Payment Rates for the ASC grouper assigned in Appendix DD.) Outpatient Hospital Surgical Services Appendix C 5160-2-21 Outpatient Hospital Clinic Services Appendix D 5160-2-21 Hospital Emergency Room Visits Appendix E 5160-2-21 Outpatient Hospital Ancillary Services Appendix F 5160-2-21 Outpatient Hospital Radiology Services Appendix G 5160-2-21 Outpatient Hospital Laboratory Services Appendix H 5160-2-21 As of Jan. 1, 2014 Code Service Description -

2013 Abstracts Revised 06�10�13 Sm
MID-AMERICA ORTHOPAEDIC ASSOCIATION 31 st Annual Meeting April 17-21, 2013 Omni Amelia Island Resort Amelia Island, FL Podium and Poster Abstracts NOTE: Disclosure information is listed at the end of this document. MAOA FIRST PLENARY SESSION April 18, 2013 1. Long-Term Outcomes of Modified Eden-Lange Tendon Transfer for Symptomatic Trapezius Paralysis from Spinal Accessory Nerve Injury Eric R. Wagner, M.D. Rochester, MN *Basseem T. Elhassan, M.D. Rochester, MN PURPOSE: The purpose of this study is to evaluate the outcome of multiple tendon transfers to the scapula to stabilize the scapulothoracic articulation in the treatment of symptomatic trapezius paralysis. METHODS: Thirteen patients, with average age of 25 years, had a history of trapezius paralysis secondary to spinal accessory nerve injury that failed to recover spontaneously or after nerve repair. The indications for surgery included shoulder pain and weakness and limited range of motion of the shoulder, specifically shoulder abduction. All patients underwent triple tendon transfer, including transfer of the levator scapulae with its bony insertion to the lateral aspect of the spine of the scapula, rhomboid minor with its bony insertion to the spine of the scapula just medial to the levator scapulae insertion, and rhomboid major tendinous insertion to the medial spine of the scapula and superomedial aspect of the infraspinatus fossa. All patients had a CT scan and ultrasound done at brace removal and beyond one year. RESULTS: At an average follow-up of 25 months (15-35), all patients had improvement of neck asymmetry, restoration of the scapula position compared to the opposite site, and no evidence of winging.