Ipo) List for Cy 2021 (N=266)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Femoral Shaft Fractures Andrew Chen, MD University of North Carolina
Femoral Shaft Fractures Andrew Chen, MD University of North Carolina Core Curriculum V5 Disclosure All figures belong to Andrew Chen, MD unless otherwise indicated Core Curriculum V5 Objectives • Review initial management of femoral shaft fractures and possible concomitant injuries • Discuss multiple options with intramedullary nailing • Antegrade/retrograde • Starting point • Reaming • Patient positioning • Understand commonly associated complications Core Curriculum V5 Femoral Shaft Fractures • Bimodal distribution • Young patients after high-energy trauma • Elderly patients after falls from standing secondary to osteopenia/osteoporosis • MVC, MCC, pedestrian struck, fall from height, and gunshot wounds most common mechanisms • Intramedullary nail as “gold standard” treatment, which has continued to evolve since introduction by Gerhard Küntscher around World War II Core Curriculum V5 Anatomy • Largest and strongest bone in body • Anterior bow with radius of curvature ~120 cm1 • Blood supply from primary nutrient vessel through linea aspera and small periosteal vessels • Deformity pattern dependent on attached musculature • Proximal fragment • Flexed (gluteus medius/minimus on greater trochanter) • Abducted (iliopsoas on lesser trochanter) • Distal fragment • Varus (adductors inserting on medial aspect distal femur) • Extension (gastrocnemius attaching on distal aspect of posterior femur) Courtesy of Rockwood and Green’s Fracture in Adults2 Core Curriculum V5 Femur Fracture Classification: AO/OTA • Bone Segment 32 • Type A • Simple • -

Microsurgery: Free Tissue Transfer and Replantation
MICROSURGERY: FREE TISSUE TRANSFER AND REPLANTATION John R Griffin MD and James F Thornton MD HISTORY In 1964 Nakayama and associates15 reported In the late 1890s and early 1900s surgeons began what is most likely the first clinical series of free- approximating blood vessels, both in laboratory ani- tissue microsurgical transfers. The authors brought mals and human patients, without the aid of magni- vascularized intestinal segments to the neck for cer- fication.1,2 In 1902 Alexis Carrel3 described the vical esophageal reconstruction in 21 patients. The technique of triangulation for blood vessel anasto- intestinal segments were attached by direct microvas- mosis and advocated end-to-side anastomosis for cular anastomoses in vessels 3–4mm diam. Sixteen blood vessels of disparate size. Nylen4 first used a patients had a functional esophagus on follow-up of monocular operating microscope for human ear- at least 1y. drum surgery in 1921. Soon after, his chief, Two separate articles in the mid-1960s described Holmgren, used a stereoscopic microscope for the successful experimental replantation of rabbit otolaryngologic procedures.5 ears and rhesus monkey digits.16,17 Komatsu and 18 In 1960 Jacobson and coworkers,6 working with Tamai used a surgical microscope to do the first laboratory animals, reported microsurgical anasto- successful replantation of a completely amputated moses with 100% patency in carotid arteries as digit in 1968. That same year Krizek and associ- 19 small as 1.4mm diameter. In 1965 Jacobson7 was ates reported the first successful series of experi- able to suture vessels 1mm diam with 100% patency mental free-flap transfers in a dog model. -

Rare Combination of Ipsilateral Acetabular Fracture-Dislocation and Pertrochanteric Fracture
A Case Report & Literature Review Rare Combination of Ipsilateral Acetabular Fracture-Dislocation and Pertrochanteric Fracture Kevin M. Kuhn, CDR, MC, USN, John A. Boudreau, MD, and J. Tracy Watson, MD oral fractures. Other case reports have described acetabular Abstract fracture-dislocations associated with femoral neck fractures.1-3 Acetabular fracture-dislocations are severe This case report describes an acetabular fracture-dislocation injuries that require urgent closed reduction associated with an ipsilateral pertrochanteric fracture and sub- of the hip and often require surgery to restore trochanteric extension. hip stability. Other authors have described We propose a staged treatment strategy consisting of early acetabular fracture-dislocations associated minimally invasive reduction of the hip and delayed reduction with femoral neck fractures, but to our knowl- and fixation of the fractures. This strategy may be useful in edge, this case report is the first to describe an managing a polytraumatized patient who may not be stable acetabular fracture-dislocation in association enough to undergo early definitive management, or a patient with an ipsilateral pertrochanteric fracture and who requires prolonged transfer to receive definitive care. subtrochanteric extension. The patient provided written informed consent for print The polytraumatized patient initially was not and electronic publication of this case report. stable enough for prolonged surgery. Through a 3-cm anterolateral hip incision, a 5-mmAJO Schanz Case Report screw was introduced percutaneously into the A 44-year-old man was involved in a head-on motor vehicle femoral head through the primary fracture site collision at highway speed. He was taken to a local hospital, under fluoroscopic guidance. -

The Use of Bone Age in Clinical Practice – Part 2
Mini Review HORMONE Horm Res Paediatr 2011;76:10–16 Received: March 25, 2011 RESEARCH IN DOI: 10.1159/000329374 Accepted: May 16, 2011 PÆDIATRIC S Published online: June 21, 2011 The Use of Bone Age in Clinical Practice – Part 2 a d f e b David D. Martin Jan M. Wit Ze’ev Hochberg Rick R. van Rijn Oliver Fricke g h j c George Werther Noël Cameron Thomas Hertel Stefan A. Wudy i k a a Gary Butler Hans Henrik Thodberg Gerhard Binder Michael B. Ranke a b Pediatric Endocrinology and Diabetology, University Children’s Hospital, Tübingen , Children’s Hospital, c University of Cologne, Cologne , and Paediatric Endocrinology and Diabetology, Justus Liebig University, Giessen , d e Germany; Department of Pediatrics, Leiden University Medical Center, Leiden , and Department of Radiology, f Emma Children’s Hospital/Academic Medical Center Amsterdam, Amsterdam , The Netherlands; Meyer Children’s g Hospital, Rambam Medical Center, Haifa , Israel; Department of Endocrinology, Royal Children’s Hospital h Parkville, Parkville, Vic. , Australia; Centre for Global Health and Human Development, Loughborough University, i Loughborough , and Institute of Child Health, University College London and University College London Hospital, j k London , UK; H.C. Andersen Children’s Hospital, Odense University Hospital, Odense , and Visiana, Holte , Denmark Key Words ness and cortical thickness should always be evaluated in -Skeletal maturity ؒ Bone age ؒ Tall stature ؒ relation to a child’s height and BA, especially around puber Precocious puberty ؒ Congenital adrenal hyperplasia ؒ ty. The use of skeletal maturity, assessed on a radiograph Bone mineral density alone to estimate chronological age for immigration author- ities or criminal courts is not recommended. -

Treatment of Common Hip Fractures: Evidence Report/Technology
This report is based on research conducted by the Minnesota Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. HHSA 290 2007 10064 1). The findings and conclusions in this document are those of the authors, who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help clinicians, employers, policymakers, and others make informed decisions about the provision of health care services. This report is intended as a reference and not as a substitute for clinical judgment. This report may be used, in whole or in part, as the basis for the development of clinical practice guidelines and other quality enhancement tools, or as a basis for reimbursement and coverage policies. AHRQ or U.S. Department of Health and Human Services endorsement of such derivative products may not be stated or implied. Evidence Report/Technology Assessment Number 184 Treatment of Common Hip Fractures Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. HHSA 290 2007 10064 1 Prepared by: Minnesota Evidence-based Practice Center, Minneapolis, Minnesota Investigators Mary Butler, Ph.D., M.B.A. Mary Forte, D.C. Robert L. Kane, M.D. Siddharth Joglekar, M.D. Susan J. Duval, Ph.D. Marc Swiontkowski, M.D. -

Femoral Shaft Fracture Fixation and Chest Injury After Polytrauma
This is an enhanced PDF from The Journal of Bone and Joint Surgery The PDF of the article you requested follows this cover page. Femoral Shaft Fracture Fixation and Chest Injury After Polytrauma Lawrence B. Bone and Peter Giannoudis J Bone Joint Surg Am. 2011;93:311-317. doi:10.2106/JBJS.J.00334 This information is current as of January 25, 2011 Reprints and Permissions Click here to order reprints or request permission to use material from this article, or locate the article citation on jbjs.org and click on the [Reprints and Permissions] link. Publisher Information The Journal of Bone and Joint Surgery 20 Pickering Street, Needham, MA 02492-3157 www.jbjs.org 311 COPYRIGHT Ó 2011 BY THE JOURNAL OF BONE AND JOINT SURGERY,INCORPORATED Current Concepts Review Femoral Shaft Fracture Fixation and Chest Injury After Polytrauma By Lawrence B. Bone, MD, and Peter Giannoudis, MD, FRCS Thirty years ago, the standard of care for the multiply injured tients with multiple injuries, defined as an ISS of ‡18, and patient with fractures was placement of the fractured limb in a patients with essentially an isolated femoral fracture and an splint or skeletal traction, until the patient was considered stable ISS of <18. Pulmonary complications consisting of ARDS, enough to undergo surgery for fracture fixation1. This led to a pulmonary dysfunction, fat emboli, pulmonary emboli, and number of complications2, such as adult respiratory distress pneumonia were present in 38% (fourteen) of thirty-seven syndrome (ARDS), infection, pneumonia, malunion, non- patients in the late fixation/multiple injuries group and 4% union, and death, particularly when the patient had a high (two) of forty-six in the early fixation/multiple injuries group; Injury Severity Score (ISS)3. -

Viewed at a Minimum Follow-Up of 2 Years (Maximum of 3 Years and 9 Months)
J Orthopaed Traumatol (2012) 13 (Suppl 1):S57–S89 DOI 10.1007/s10195-012-0210-2 12 NOVEMBER 2012 In-Depth Oral Presentations and Oral Communications IN-DEPTH ORAL PRESENTATIONS achieve a stable synthesis and an early mobilization of the MP and IP joints. However, if a malunion is present, it has to be corrected sur- gically as soon as possible. AT05–HAND AND WRIST Radio-distal epiphysis fractures: treatment with angular stability Treatment of malunion of the proximal phalangeal fractures plate of latest generation of the hand R. Di Virgilio*, E. Coppari, E. Condarelli, M. Rendine V. Potenza*, S. Bisicchia, R. Caterini, A. Fichera, P. Farsetti, E. Ippolito (Rome, IT) Universita` di Roma Tor Vergata (Rome, IT) Introduction Distal radius fractures are the most common fractures of the upper limb and coincide with 17 % of all fractures treated in Introduction It is difficult to treat fractures of the phalanges of the emergency rooms. The incidence of these fractures is greater in hand because they can cause complications such as deformity and patients aged 6 to 10 years, and in those between 60 and 70 years. joint limitation with a reduction in the grasping function. The most In older patients the incidence is higher in females. In the articular frequent complications are malunion of the fracture and joint limi- fractures, displaced, dislocated and highly unstable is indicated tation. The greatest incidence of complications can be found in open internal fixation (ORIF) to restore the congruity of the joint transverse fractures of the base of the proximal phalanx, in articular surface, to restore the correct length of the radius, its inclination fractures, comminuted fractures, and in those associated with lesions and palmar tilt. -
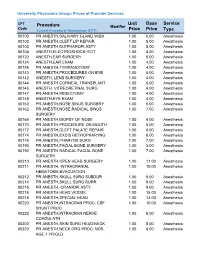
Unit Price Base Price Service Type Procedure
University Physicians Group: Prices of Provider Services CPT Unit Base Service Procedure Modifier Code ype Current Procedural Terminology (CPT) Price Price T 00100 PR ANESTH,SALIVARY GLAND W/BX 1.00 5.00 Anesthesia 00102 PR ANESTH,CLEFT LIP REPAIR 1.00 6.00 Anesthesia 00103 PR ANESTH,BLEPHAROPLASTY 1.00 5.00 Anesthesia 00104 ANESTH,ELECTROSHOCK/ ECT 1.00 4.00 Anesthesia 00120 ANESTH,EAR SURGERY 1.00 5.00 Anesthesia 00124 ANESTH,EAR EXAM 1.00 4.00 Anesthesia 00126 PR ANESTH,TYMPANOTOMY 1.00 4.00 Anesthesia 00140 PR ANESTH,PROCEDURES ON EYE 1.00 5.00 Anesthesia 00142 ANESTH, LENS SURGERY 1.00 4.00 Anesthesia 00144 PR ANESTH,CORNEAL TRANSPLANT 1.00 6.00 Anesthesia 00145 ANESTH, VITREORETINAL SURG 1.00 6.00 Anesthesia 00147 PR ANESTH,IRIDECTOMY 1.00 4.00 Anesthesia 00148 ANESTH,EYE EXAM 1.00 4.00 Anesthesia 00160 PR ANESTH,NOSE,SINUS SURGERY 1.00 5.00 Anesthesia 00162 PR ANESTH,NOSE,RADICAL SINUS 1.00 7.00 Anesthesia SURGERY 00164 PR ANESTH,BIOPSY OF NOSE 1.00 4.00 Anesthesia 00170 PR ANESTH,PROCEDURE ON MOUTH 1.00 5.00 Anesthesia 00172 PR ANESTH,CLEFT PALATE REPAIR 1.00 6.00 Anesthesia 00174 PR ANESTH,EXCIS RETROPHARYNG 1.00 6.00 Anesthesia 00176 PR ANESTH,PHARYNX SURG 1.00 7.00 Anesthesia 00190 PR ANESTH,FACIAL BONE SURGERY 1.00 5.00 Anesthesia 00192 PR ANESTH,RADICAL FACIAL BONE 1.00 7.00 Anesthesia SURGERY 00210 PR ANESTH,OPEN HEAD SURGERY 1.00 11.00 Anesthesia 00211 PR ANESTH, INTRACRANIAL 1.00 10.00 Anesthesia HEMATOMA EVACUATION 00212 PR ANESTH,SKULL SURG SUBDUR 1.00 5.00 Anesthesia 00214 PR ANESTH,SKULL SURG BURR 1.00 9.00 Anesthesia -
Knee Surgery-Arthroscopic and Open Procedures Version 1.0 Effective February 14, 2020
CLINICAL GUIDELINES CMM-312: Knee Surgery-Arthroscopic and Open Procedures Version 1.0 Effective February 14, 2020 Clinical guidelines for medical necessity review of Comprehensive Musculoskeletal Management Services. © 2019 eviCore healthcare. All rights reserved. Comprehensive Musculoskeletal Management Guidelines V1.0 CMM-312: Knee Surgery-Arthroscopic and Open Procedures CMM-312.1: Definitions 3 CMM-312.2: General Guidelines 5 CMM-312.3: Indications and Non-Indications 5 CMM-312.4: Experimental, Investigational, or Unproven 15 CMM-312.5: Procedure (CPT®) Codes 16 CMM-312.6: Procedure (HCPCS) Codes 19 CMM-312.7: References 20 ______________________________________________________________________________________________________ ©2020 eviCore healthcare. All Rights Reserved. Page 2 of 25 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Comprehensive Musculoskeletal Management Guidelines V1.0 CMM -312.1: Definitions The Modified Outerbridge Classification is a system that has been developed for judging articular cartilage injury to the knee. This system allows delineation of varying areas of chondral pathology, based on the qualitative appearance of the cartilage surface, and can assist in identifying those injuries that are suitable for repair techniques. The characterization of cartilage in this system is as follows: Grade I – Softening with swelling Grade II – Fragmentation and fissuring less than one square centimeter (1 cm2) Grade III – Fragmentation and fissuring greater than one square centimeter -

Pediatric Ankle Fractures
CHAPTER 26 PEDIATRIC ANKLE FRACTURES Sofi e Pinney, DPM, MS INTRODUCTION stronger than both the physis and bone. As a result, there is a greater capacity for plastic deformation and less chance of The purpose of this review is to examine the current intra-articular fractures, joint dislocation, and ligamentous literature on pediatric ankle fractures. I will discuss the disruptions. However, ligamentous injury may be more anatomic considerations of a pediatric patient, how to common than originally believed (1). A case-control study evaluate and manage these fractures, and when to surgically by Zonfrillo et al found an association between an increased repair them. Surgical techniques and complications will be risk of athletic injury in obese children, and concluded a briefl y reviewed. higher body mass index risk factor for ankle sprains (4). Ankle fractures are the third most common fractures in Secondary ossifi cation centers are located in the children, after the fi nger and distal radial physeal fracture. epiphysis. The distal tibial ossifi cation center appears at 6-24 Approximately 20-30% of all pediatric fractures are ankle months of age and closes asymmetrically over an 18-month fractures. Most ankle fractures occur at 8-15 years old. The period fi rst central, then medial and posterior, with the peak injury age is 11-12 years, and is relatively uncommon anterolateral portion closing last at 15 and 17 years of age for under the age 5. This injury is more common in boys. females and males, respectively. The distal fi bula ossifi cation The most common cause of pediatric ankle fractures is a center appears at 9-24 months of age and closes 1-2 years rotational force, and is often seen in sports injuries associated after the distal tibial. -

Commercial Musculoskeletal Codes
Updated January 2018 Commercial Musculoskeletal Codes Investigational or Non-Covered Spine Surgery Pain Management Joint Surgery Codes associated with an Arthrogram CPT Description Commercial Notes Partial excision of posterior vertebral component (eg, spinous 22100 process, lamina or facet) for intrinsic bony lesion, single vertebral segment; cervical 22101 Partial excision of posterior vertebral component (eg, spinous process, lamina or facet) for intrinsic bony lesion, single vertebral segment; thoracic 22102 Partial excision of posterior vertebral component (eg, spinous process, lamina or facet) for intrinsic bony lesion, single vertebral segment; lumbar Partial excision of posterior vertebral component (eg, spinous process, 22103 lamina or facet) for intrinsic bony lesion, single vertebral segment; each additional segment (List separately in addition to code for primary procedure) Partial excision of vertebral body, for intrinsic bony lesion, without 22110 decompression of spinal cord or nerve root(s), single vertebral segment;cervical Partial excision of vertebral body, for intrinsic bony lesion, without 22112 decompression of spinal cord or nerve root(s), single vertebral segment; thoracic Partial excision of vertebral body, for intrinsic bony lesion, without 22114 decompression of spinal cord or nerve root(s), single vertebral segment; lumbar each additional vertebral segment (list separately in addition to code 22116 for primary procedure) Osteotomy of spine, posterior or posterolateral approach, 3 columns, 22206 1 vertebral -
Pulmonary Dysfunction in Patients with Femoral Shaft Fracture Treated with Intramedullary Nailing by BRENT L
COPYRIGHT © 2001 BY THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED Pulmonary Dysfunction in Patients with Femoral Shaft Fracture Treated with Intramedullary Nailing BY BRENT L. NORRIS, MD, W. CHRISTOPHER PATTON, MD, JOSEPH N. RUDD JR., BSN, PHD, COLLEEN M. SCHMITT, MD, MHS, AND JEFFREY A. KLINE, MD Investigation performed at the University of Tennessee College of Medicine, Chattanooga, Tennessee, and the Carolinas Medical Center, Charlotte, North Carolina Background: This study was undertaken to determine whether alveolar dead space increases during intramedul- lary nailing of femoral shaft fractures and whether alveolar dead space predicts postoperative pulmonary dysfunc- tion in patients undergoing intramedullary nailing of a femoral shaft fracture. Methods: All patients with a femoral shaft fracture were prospectively enrolled in the study unless there was evi- dence of acute myocardial infarction, shock, or heart failure. Arterial blood gases were measured at three consec- utive time-periods after induction of general anesthesia: before intramedullary nailing and ten and thirty minutes after intramedullary nailing. The end-tidal carbon-dioxide level, minute ventilation, positive end-expiratory pres- sure, and percent of inspired and expired inhalation agent were recorded simultaneously with the blood-gas mea- surement. Postoperatively, all subjects were monitored for evidence of pulmonary dysfunction, defined as the need for mechanical ventilation or supplemental oxygen (at a fraction of inspired oxygen of >40%) in the presence of clinical signs of a respiratory rate of >20 breaths/min or the use of accessory muscles of respiration. Results: Seventy-four patients with a total of eighty femoral shaft fractures completed the study. Fifty fractures (62.5%) underwent nailing after reaming, and thirty fractures (37.5%) underwent nailing with minimal or no ream- ing.