University of Dundee Refining the Primrose Syndrome Phenotype
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Orphanet Report Series Rare Diseases Collection
Marche des Maladies Rares – Alliance Maladies Rares Orphanet Report Series Rare Diseases collection DecemberOctober 2013 2009 List of rare diseases and synonyms Listed in alphabetical order www.orpha.net 20102206 Rare diseases listed in alphabetical order ORPHA ORPHA ORPHA Disease name Disease name Disease name Number Number Number 289157 1-alpha-hydroxylase deficiency 309127 3-hydroxyacyl-CoA dehydrogenase 228384 5q14.3 microdeletion syndrome deficiency 293948 1p21.3 microdeletion syndrome 314655 5q31.3 microdeletion syndrome 939 3-hydroxyisobutyric aciduria 1606 1p36 deletion syndrome 228415 5q35 microduplication syndrome 2616 3M syndrome 250989 1q21.1 microdeletion syndrome 96125 6p subtelomeric deletion syndrome 2616 3-M syndrome 250994 1q21.1 microduplication syndrome 251046 6p22 microdeletion syndrome 293843 3MC syndrome 250999 1q41q42 microdeletion syndrome 96125 6p25 microdeletion syndrome 6 3-methylcrotonylglycinuria 250999 1q41-q42 microdeletion syndrome 99135 6-phosphogluconate dehydrogenase 67046 3-methylglutaconic aciduria type 1 deficiency 238769 1q44 microdeletion syndrome 111 3-methylglutaconic aciduria type 2 13 6-pyruvoyl-tetrahydropterin synthase 976 2,8 dihydroxyadenine urolithiasis deficiency 67047 3-methylglutaconic aciduria type 3 869 2A syndrome 75857 6q terminal deletion 67048 3-methylglutaconic aciduria type 4 79154 2-aminoadipic 2-oxoadipic aciduria 171829 6q16 deletion syndrome 66634 3-methylglutaconic aciduria type 5 19 2-hydroxyglutaric acidemia 251056 6q25 microdeletion syndrome 352328 3-methylglutaconic -

Neonatal Diabetes and MODY Information Sheet 6-14-19
Next Generation Sequencing Panels for Neonatal Diabetes Mellitus (NDM) and Maturity-Onset Diabetes of the Young (MODY) Monogenic diabetes mellitus includes a heterogeneous group of diabetes types that are caused by mutations in single genes. It is estimated that the monogenic forms of diabetes could represent as much as 1–2% of all cases of diabetes mellitus 1. The main phenotypes suggestive of an underlying monogenic cause include neonatal diabetes mellitus (NDM), maturity-onset diabetes of the young (MODY) and very rare diabetes-associated syndromes. Neonatal Diabetes Mellitus (NDM) is diabetes diagnosed within the first 6 months of life and can be characterized as either permanent (PNDM), requiring lifelong treatment, or transient (TNDM), which typically resolves by 18 months of age. NDM is rare with an incidence of approximately 1:1,000,000-260,000 live births. Maturity-onset diabetes of the young (MODY) is more common than NDM and usually occurs in children or adolescents but may be mild and not detected until adulthood. It is predicted that MODY accounts for approximately 1-2% of all Diabetes cases with an incidence of approximately 100 cases per million in the UK population. Approximately thirty genes that are highly expressed in the pancreatic beta-cell have been identified in these monogenic subtypes of diabetes, and many other genes have been implicated in syndromes that often include diabetes. Several etiological mechanisms of beta-cell dysfunction are involved including reduced beta-cell number, failure of glucose sensing and increased destruction of the beta-cell, which result in inadequate insulin secretion despite chronic hyperglycemia 2-4. -
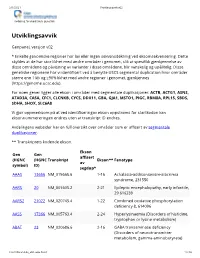
Utviklingsavvik V02
2/1/2021 Utviklingsavvik v02 Avdeling for medisinsk genetikk Utviklingsavvik Genpanel, versjon v02 * Enkelte genomiske regioner har lav eller ingen sekvensdekning ved eksomsekvensering. Dette skyldes at de har stor likhet med andre områder i genomet, slik at spesifikk gjenkjennelse av disse områdene og påvisning av varianter i disse områdene, blir vanskelig og upålitelig. Disse genetiske regionene har vi identifisert ved å benytte USCS segmental duplication hvor områder større enn 1 kb og ≥90% likhet med andre regioner i genomet, gjenkjennes (https://genome.ucsc.edu). For noen gener ligger alle ekson i områder med segmentale duplikasjoner: ACTB, ACTG1, ASNS, ATAD3A, CA5A, CFC1, CLCNKB, CYCS, DDX11, GBA, GJA1, MSTO1, PIGC, RBM8A, RPL15, SBDS, SDHA, SHOX, SLC6A8 Vi gjør oppmerksom på at ved identifiseringav ekson oppstrøms for startkodon kan eksonnummereringen endres uten at transkript ID endres. Avdelingens websider har en full oversikt over områder som er affisert av segmentale duplikasjoner. ** Transkriptets kodende ekson. Ekson Gen Gen affisert (HGNC (HGNC Transkript Ekson** Fenotype av symbol) ID) segdup* AAAS 13666 NM_015665.6 1-16 Achalasia-addisonianism-alacrimia syndrome, 231550 AARS 20 NM_001605.2 2-21 Epileptic encephalopathy, early infantile, 29 616339 AARS2 21022 NM_020745.4 1-22 Combined oxidative phosphorylation deficiency 8, 614096 AASS 17366 NM_005763.4 2-24 Hyperlysinaemia (Disorders of histidine, tryptophan or lysine metabolism) ABAT 23 NM_020686.6 2-16 GABA transaminase deficiency (Disorders of neurotransmitter metabolism, gamma-aminobutyrate) -

Mendeliome Panel Versie V3 (4362 Genen) Centrum Voor Medische Genetica Gent
H9.1-OP2-B24: Genpanel Mendeliome, in voege op 15/09/2020 Mendeliome panel versie V3 (4362 genen) Centrum voor Medische Genetica Gent Associated phenotype, OMIM phenotype ID, phenotype Gene OMIM gene ID mapping key and inheritance pattern {Alzheimer disease, susceptibility to}, 104300 (3), Autosomal A2M 103950 dominant A2ML1 610627 {Otitis media, susceptibility to}, 166760 (3), Autosomal dominant [Blood group, P1Pk system, p phenotype], 111400 (3); NOR A4GALT 607922 polyagglutination syndrome, 111400 (3); [Blood group, P1Pk system, P(2) phenotype], 111400 (3) Achalasia-addisonianism-alacrimia syndrome, 231550 (3), AAAS 605378 Autosomal recessive Keratoderma, palmoplantar, punctate type IA, 148600 (3), AAGAB 614888 Autosomal dominant Epileptic encephalopathy, early infantile, 29, 616339 (3), AARS1 601065 Autosomal recessive; Charcot-Marie-Tooth disease, axonal, type (AARS) 2N, 613287 (3), Autosomal dominant Combined oxidative phosphorylation deficiency 8, 614096 (3), AARS2 612035 Autosomal recessive; Leukoencephalopathy, progressive, with ovarian failure, 615889 (3), Autosomal recessive AASS 605113 Hyperlysinemia, 238700 (3), Autosomal recessive ABAT 137150 GABA-transaminase deficiency, 613163 (3), Autosomal recessive HDL deficiency, familial, 1, 604091 (3); Tangier disease, 205400 ABCA1 600046 (3), Autosomal recessive Ichthyosis, congenital, autosomal recessive 4B (harlequin), ABCA12 607800 242500 (3), Autosomal recessive; Ichthyosis, congenital, autosomal recessive 4A, 601277 (3), Autosomal recessive Intellectual developmental disorder -
13/2019 Wissenschaftliche Publikationen
BEILAGE BEILAGE FORSCHUNGSMAGAZIN NR. 13/2019 Wissenschaftliche Publikationen Publikationsliste 2018 der Medizinischen und Chirurgischen Kliniken, der Abteilungen für Klinische Chemie und Biochemie, Intensivmedizin und Neonatologie, Anästhesie und Bilddiagnostik am Universitäts-Kinderspital Zürich. Artikel in wissenschaftlichen Zeitschriften Aebi-Popp, K, Wandeler, G, Salazar-Vizcaya, Akdis, D, Saguner, A M, Medeiros-Domingo, A, Albisetti, Manuela, Schlosser, Arno, Brueck- L, Metzner, K, Stöckle, M, Cavassini, M, Schaller, A, Balmer, C, Steffel, J, Brunckhorst, mann, Martina, Gropper, Savion, Glund, Ste- Hoffmann, M, Lüthi, A, Suter, F, Bernasconi, C, Duru, F (2018): Multiple clinical profiles of phan, Tartakovsky, Igor, Brandão, Leonardo R, E, Fehr, Jan, Furrer, H, Rauch, A. Swiss HIV families with the short QT syndrome. Europace Reilly, Paul A (2018): Rationale and design of a Cohort Study (2018): Rapid decline of anti- 20 (FI1), f113-f121 phase III safety trial of idarucizumab in children hepatitis C virus (HCV) antibodies following receiving dabigatran etexilate for venous Akeret, Kevin, Bellut, David, Huppertz, Hans- early treatment of incident HCV infections in thromboembolism. Research and Practice in Jürgen, Ramantani, Georgia, König, Kris- HIV-infected men who have sex with men. HIV Thrombosis and Haemostasis 2 (1), 69-76 tina, Serra, Carlo, Regli, Luca, Krayenbühl, Medicine 19 (6), 420-425 Niklaus (2018): Ultrasonographic features of Alfadhel, Majid, Nashabat, Marwan, Alrifai, Aebi-Popp, K, Bernasconi, E, Kahlert, C, Mar- focal -

Psykisk Utviklingshemming
Psykisk utviklingshemming Genpanel, versjon v02 Endring fra v01: Fjernet BRCA2 Tabellen er sortert på gennavn (HGNC gensymbol) Navn på gen er iht. HGNC Kolonnen >x10 viser andel av genet som vi forventer blir lest med tilfredstillende kvalitet flere enn 10 ganger under sekvensering Gen Transkript >10x Fenotype (symbol) AAAS NM_015665.5 100% Achalasia-addisonianism-alacrimia syndrome OMIM AASS NM_005763.3 100% Hyperlysinemia OMIM Saccharopinuria OMIM ABCC9 NM_005691.3 100% Hypertrichotic osteochondrodysplasia OMIM ABCD1 NM_000033.3 76% Adrenoleukodystrophy OMIM ABCD4 NM_005050.3 100% Methylmalonic aciduria and homocystinuria, cblJ type OMIM ABHD5 NM_016006.4 100% Chanarin-Dorfman syndrome OMIM ACAD9 NM_014049.4 100% Mitochondrial complex I deficiency due to ACAD9 deficiency OMIM ACADM NM_000016.5 100% Acyl-CoA dehydrogenase, medium chain, deficiency of OMIM ACADS NM_000017.3 100% Acyl-CoA dehydrogenase, short-chain, deficiency of OMIM ACADVL NM_000018.3 100% VLCAD deficiency OMIM ACAT1 NM_000019.3 100% Alpha-methylacetoacetic aciduria OMIM ACO2 NM_001098.2 97% Infantile cerebellar-retinal degeneration OMIM ACOX1 NM_004035.6 100% Peroxisomal acyl-CoA oxidase deficiency OMIM ACSL4 NM_004458.2 99% Mental retardation, X-linked 63 OMIM Gen Transkript >10x Fenotype (symbol) ACTA2 NM_001613.2 100% Moyamoya disease 5 OMIM Multisystemic smooth muscle dysfunction syndrome OMIM ACTB NM_001101.3 100% ?Dystonia, juvenile-onset OMIM Baraitser-Winter syndrome 1 OMIM ACTG1 NM_001614.3 100% Baraitser-Winter syndrome 2 OMIM Deafness, autosomal dominant 20/26 OMIM -

ZIEGLER-DISSERTATION-2018.Pdf
DELINEATING THE MECHANISMS UNDERLYING RARE DISORDERS OF ECTOPIC CALCIFICATION TO REVEAL NOVEL THERAPEUTIC STRATEGIES by Shira G. Ziegler A dissertation submitted to Johns Hopkins University in conformity with the requirements for the degree of Doctor of Philosophy Baltimore, Maryland May, 2017 © 2017 Shira G. Ziegler All Rights Reserved ABSTRACT Biallelic mutations in ABCC6 cause pseudoxanthoma elasticum (PXE), a disease characterized by calcification in the skin, eyes, and blood vessels. While the function of ABCC6 and pathogenesis of PXE remains unclear, the mechanisms of related ectopic calcification disorders are better understood. Generalized arterial calcification of infancy (GACI) is caused by biallelic mutations in ENPP1, which encodes an enzyme that converts ATP to AMP and pyrophosphate (PPi), a major inhibitor of tissue calcification. AMP is further degraded to adenosine and inorganic phosphate by CD73, encoded by NT5E. We recently discovered that biallelic mutations in NT5E cause calcification of joints and arteries. We reasoned that a test for genetic interaction in mouse models of ectopic calcification might inform the pathogenesis of PXE. Enpp1-/- and Abcc6-/- mice showed fibrous capsule calcification of the vibrissae (an early marker of ectopic calcification) at 15 weeks of age, while Nt5e-/- mice calcified after one year. Abcc6-/- mice with one mutated Enpp1 or two defective Nt5e alleles showed accentuated calcification with strong statistical evidence for synergy. Additionally, ABCC6, ENPP1, and CD73 exhibited regulatory interactions; human fibroblasts with biallelic ABCC6 mutations had increased ENPP1 and decreased CD73 activity. Taken together, these data suggest that ABCC6 participates with ENPP1 and CD73 in ATP metabolism. Under osteogenic culture conditions, ABCC6 mutant cells calcified, suggesting a provoked cell- autonomous defect. -

Supplemental Figures and Tables Table S1. Summary of the Trio And
Supplementary material J Med Genet Supplemental figures and tables Table S1. Summary of the trio and single proband-based exome sequencing experiment. Sequencing Mean Percent Candidate Total NS/SS/I Family Individual output sequencing target de novo variantsa variantsa (in Gb) Depth (median) ≥ 10X SNV Trio 1 P1 dijex132 3,49 101.13 93.9 47848 14369 1 Mother dijex133 3,18 92.05 94.0 48178 14498 - Father dijex134 3,19 92.29 94.0 46912 14019 - Trio 2 P2 dijex135 3,23 93.38 94.0 48097 14526 1 Mother dijex136 3,63 105.11 94.4 48258 14480 - Father dijex137 3,32 96.19 94.0 47934 14657 - Trio 3 P3 dijex138 3,19 92.38 93.5 48365 14504 2 Mother dijex139 3 86.75 93.8 48229 14400 - Father dijex140 3,43 99.31 94.1 48035 14540 - Trio 4 P4 dijex141 3,42 98.89 94.5 47107 14126 2 Mother dijex142 3,69 106.78 94.4 47583 14365 - Father dijex143 3,38 97.81 94.3 48296 14667 - Trio 5 P5 dijex144 3,02 87.48 93.8 47648 14425 3 Mother dijex145 3,16 91.37 93.9 47284 14275 - Father dijex146 3,3 95.66 93.9 47964 14589 - Trio 6 P6 dijex147 3,51 101.74 94.1 48192 14568 3 Mother dijex148 3,15 91.20 93.8 48211 14638 - Father dijex149 3,11 90.12 93.8 47109 14178 - Trio 7 P7 dijex150 3,23 93.64 94.4 47648 14393 2 Mother dijex151 3,66 105.85 94.6 48040 14633 - Father dijex152 3,06 88.55 94.1 47950 14557 - Trio 8 P8 dijex153 3,18 91.99 94.0 48028 14633 4 Mother dijex154 3,42 99.05 94.0 48065 14472 - Father dijex155 3,43 99.40 94.0 48475 14635 - Trio 9 P9 dijex156 3,41 98.83 94.3 48682 14759 2 Mother dijex157 3,21 92.90 94.0 47604 14276 - Father dijex158 3,18 92.14 93.7 47682 -

American Osteopathic College of Dermatology Journal of the American Osteopathic College of Dermatology
Journal of the American Osteopathic College of Dermatology Journal of the American Osteopathic College of Dermatology 2009-2010 AOCD Officers President: Leslie Kramer, DO, FAOCD President-Elect: Bradley Glick, DO, FAOCD First Vice-President: James Towry, DO, FAOCD Second Vice-President: Karen Neubauer, DO, FAOCD Third Vice-President: David Grice, DO, FAOCD Secretary-Treasurer: Jere Mammino, DO, FAOCD Immediate Past President: Marc Epstein, DO, FAOCD Trustees: Celeste Angel, DO, FAOCD Alpesh Desai, DO, FAOCD Mark Kuriata, DO, FAOCD Editors Rick Lin, DO, FAOCD Jay S. Gottlieb, DO Andrew Racette, DO, FAOCD Jon Keeling, DO Suzanne Rozenberg, DO, FAOCD Editorial Review Board Kevin Belasco, DO Rich Bernert, M.D. Sponsors: Iqbal Bukhari, MD Global Pathology Laboratory JAOCD Ryan Carlson, DO Medicis Founding Sponsor Igor Chaplik, DO JAOCD Founding Sponsor Michael Conroy, M.D. Galderma Brad Glick, DO, FAOCD Ranbaxy Melinda Greenfield, DO Andrew J Hanly, MD David Horowitz, DO, FAOCD JAOCD Matt Leavitt, DO, FAOCD Founding Sponsor Mark Lebwohl, MD AOCD • 1501 E. Illinois • Kirksville, MO 63501 Rick Lin, DO 800-449-2623 • FAX: 660-627-2623 www.aocd.org Megan Machuzak, D.O. Jere Mammino, DO, FAOCD COPYRIGHT AND PERMISSION: written permission must be obtained from the Journal of the American Osteopathic College of Dermatology John Minni, DO for copying or reprinting text of more than half page, tables or figures. Navid Nami, DO Permissions are normally granted contingent upon similar permission from the author(s), inclusion of acknowledgement of the original source, Shaheen Oshtory, DO and a payment of $15 per page, table or figure of reproduced material. Permission fees are waived for authors wishing to reproduce their own John Perrotto, DO articles. -

Identification of Novel Genetic Causes of Monogenic Intellectual Disability Francesca Mattioli
Identification of novel genetic causes of monogenic intellectual disability Francesca Mattioli To cite this version: Francesca Mattioli. Identification of novel genetic causes of monogenic intellectual disability. Neuro- biology. Université de Strasbourg, 2018. English. NNT : 2018STRAJ035. tel-01963143 HAL Id: tel-01963143 https://tel.archives-ouvertes.fr/tel-01963143 Submitted on 21 Dec 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. UNIVERSITÉ DE STRASBOURG ÉCOLE DOCTORALE DES SCIENCES DE LA VIE ET DE LA SANTE Institut de Génétique et Biologie Moléculaire et Cellulaire THÈSE présentée par : Francesca MATTIOLI soutenue le : 26 Juin 2018 pour obtenir le grade de : Docteur de l’université de Strasbourg Discipline/ Spécialité : Aspects Moléculaires et Cellulaires de la Biologie Identification of Novel Genetic Causes of Monogenic Intellectual Disability THÈSE co‐dirigée par : M MANDEL Jean-Louis Pr, Collège de France, IGBMC, Strasbourg Mme PITON Amélie MCU‐PH, Université de Strasbourg, IGBMC, Strasbourg RAPPORTEURS : Mme RENIERI Alessandra Pr, Università di Siena M REYMOND Alexandre Pr, Center for Integrative Genomics, Lausanne AUTRES MEMBRES DU JURY : M SERAPHIN Bertrand DR CNRS, IGBMC, Strasbourg Mme ZWEIER Christiane Pr, Institute of Human Genetics, Erlangen 1 ACKNOWLEDGMENTS I would like to thank Alessandra Renieri, Alexandre Reymond, Bertrand Seraphin and Christiane Zweier for accepting to be part of the jury, for evaluating my work and for having found time in your busy schedule to come and take part at my PhD defence. -

For Peer Review 20 Research Priority Program Radiz (Rare Disease Initiative Zurich), Fondazione Bambino Gesù (Vite 21 22 Coraggiose) and Fondazione Umberto Veronesi
Human Mutation Clinical and functional characterization of two novel ZBTB20 mutations causing Primrose syndrome Journal: Human Mutation Manuscript ForID Draft Peer Review Wiley - Manuscript type: Brief Report Date Submitted by the Author: n/a Complete List of Authors: Stellacci, Emilia; Istituto Superiore di Sanità, Oncologia e Medicina Molecolare Steindl, Katharina; Institute of Medical Genetics, University of Zurich Joset, Pascal; Institute of Medical Genetics, University of Zurich Mercurio, Laura; Istituto Superiore di Sanità, Oncologia e Medicina Molecolare Anselmi, Massimiliano; Università di Roma 'Tor Vergata', Dipartimento di Scienze e Tecnologie Chimiche Cecchetti, Serena; Istituto Superiore di Sanità, Servizio grandi strumentazioni e core facilities Gogoll, Laura; Institute of Medical Genetics, University of Zurich Zweier, Markus; Institute of Medical Genetics, University of Zurich Hackenberg, Annette; University Children's Hospital Zürich, Division of Pediatric Neurology Bocchinfuso, Gianfranco; Università di Roma 'Tor Vergata', Dipartimento di Scienze e Tecnologie Chimiche Stella, Lorenzo; Universita' "Tor Vergata", Dipartimento di Scienze e Tecnologie Chimiche Tartaglia, Marco; Bambino Gesù Children’s Hospital, IRCCS, Division of Genetic Disorders and Rare Diseases Rauch, Anita; University of Zurich, Institute of Medical Genetics Primrose syndrome, <i>ZBTB20</i>, 3q13.31 microdeletion syndrome, Key Words: mutation spectrum, functional analyses John Wiley & Sons, Inc. Page 1 of 22 Human Mutation Stellacci, Steindl, et al. Pag. -

OMIM Mendelian Gene List V2.0
Gene Disease A2M ALZHEIMER DISEASE; AD [AD] NOR polyagglutination syndrome 111400 (3) | [Blood group P1Pk system P(2) phenotype] 111400 (3) | [Blood group P1Pk system p A4GALT phenotype] 111400 (3) AAAS ACHALASIA-ADDISONIANISM-ALACRIMA SYNDROME; AAAS [AR] AAGAB PALMOPLANTAR KERATODERMA. PUNCTATE TYPE IA; PPKP1A [AD] AARS1 CHARCOT-MARIE-TOOTH DISEASE. AXONAL. TYPE 2N; CMT2N [AD] | EPILEPTIC ENCEPHALOPATHY. EARLY INFANTILE. 29; EIEE29 [AR] LEUKOENCEPHALOPATHY. PROGRESSIVE. WITH OVARIAN FAILURE; LKENP [AR] | COMBINED OXIDATIVE PHOSPHORYLATION AARS2 DEFICIENCY 8; COXPD8 [AR] AASS HYPERLYSINEMIA. TYPE I [AR] ABAT GABA-TRANSAMINASE DEFICIENCY [AR] ABCA1 TANGIER DISEASE; TGD [AR] ICHTHYOSIS. CONGENITAL. AUTOSOMAL RECESSIVE 4B; ARCI4B [AR] | ICHTHYOSIS. CONGENITAL. AUTOSOMAL RECESSIVE 4A; ARCI4A ABCA12 [AR] ABCA3 SURFACTANT METABOLISM DYSFUNCTION. PULMONARY. 3; SMDP3 [AR] MACULAR DEGENERATION. AGE-RELATED. 2; ARMD2 [AD] | STARGARDT DISEASE 1; STGD1 [AR] | RETINITIS PIGMENTOSA 19; RP19 ABCA4 [AR] ABCB11 CHOLESTASIS. BENIGN RECURRENT INTRAHEPATIC. 2; BRIC2 [AR] | CHOLESTASIS. PROGRESSIVE FAMILIAL INTRAHEPATIC. 2; PFIC2 [AR] GALLBLADDER DISEASE 1; GBD1 [AD] | CHOLESTASIS. INTRAHEPATIC. OF PREGNANCY 3; ICP3 [AD] | CHOLESTASIS. PROGRESSIVE ABCB4 FAMILIAL INTRAHEPATIC. 3; PFIC3 [AR] MICROPHTHALMIA. ISOLATED. WITH COLOBOMA 7; MCOPCB7 [AD] | DYSCHROMATOSIS UNIVERSALIS HEREDITARIA 3; DUH3 [AD] | ABCB6 PSEUDOHYPERKALEMIA. FAMILIAL. 2. DUE TO RED CELL LEAK; PSHK2 [AD] ABCB7 ANEMIA. SIDEROBLASTIC. AND SPINOCEREBELLAR ATAXIA; ASAT [XLR] ABCC2 DUBIN-JOHNSON SYNDROME; DJS [AR] ARTERIAL CALCIFICATION. GENERALIZED. OF INFANCY. 2; GACI2 [AR] | PSEUDOXANTHOMA ELASTICUM. FORME FRUSTE [AD] | ABCC6 PSEUDOXANTHOMA ELASTICUM; PXE [AR] DIABETES MELLITUS. PERMANENT NEONATAL; PNDM [AD] | HYPERINSULINEMIC HYPOGLYCEMIA. FAMILIAL. 1; HHF1 [AD] | DIABETES ABCC8 MELLITUS. NONINSULIN-DEPENDENT; NIDDM [AD] | HYPOGLYCEMIA. LEUCINE-INDUCED; LIH [AD] ABCC9 CANTU SYNDROME [AD] | ATRIAL FIBRILLATION. FAMILIAL. 12; ATFB12 [AD] | CARDIOMYOPATHY. DILATED.