Title of Presentation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WINTER Warmers the PERFECT WINTER RECIPE COLLECTION
WINTER Warmers THE PERFECT WINTER RECIPE COLLECTION What better time to chow down on hearty, soul-warming comfort food than winter? This Winter Warmers cookbook is the best collection of winter recipes around. It has soups, stews, casseroles and many more recipes to help get you through the winter blues with a satisfied stomach. TABLE OF CONTENTS Randall’s White Bean and Turkey Chili ..........................................................................................................................2 Slow Cooker White Beans with Smoked Turkey .............................................................................................................3 Great Northern Beans and Ham with Cornbread ...........................................................................................................3 Tortilla Soup with Chicken and Beans .............................................................................................................................4 Green Chili Pork Stew with Pinto Beans .........................................................................................................................5 Pinto Bean Chili Casserole ...............................................................................................................................................6 Spicy Shrimp and Corn White Bean Chowder .................................................................................................................7 Corned Beef and Bean Soup ...........................................................................................................................................8 -

Basic Beanery
344 appendix Basic Beanery name(s) origin & CharaCteristiCs soaking & Cooking Adzuki Himalayan native, now grown Soaked, Conventional Stovetop: 40 (aduki, azuki, red Cowpea, throughout Asia. Especially loved in minutes. unSoaked, Conventional Stovetop: red oriental) Japan. Small, nearly round red bean 1¼ hours. Soaked, pressure Cooker: 5–7 with a thread of white along part of minutes. unSoaked, pressure Cooker: the seam. Slightly sweet, starchy. 15–20 minutes. Lower in oligosaccharides. Anasazi New World native (present-day Soak? Yes. Conventional Stovetop: 2–2¹⁄² (Cave bean and new mexiCo junction of Arizona, New Mexico, hours. pressure Cooker: 15–18 minutes appaloosa—though it Colorado, Utah). White speckled with at full pressure; let pressure release isn’t one) burgundy to rust-brown. Slightly gradually. Slow-Cooker: 1¹⁄² hours on sweet, a little mealy. Lower in high, then 6 hours on low. oligosaccharides. Appaloosa New World native. Slightly elongated, Soak? Yes. Conventional Stovetop: 2–2¹⁄² (dapple gray, curved, one end white, the other end hours. pressure Cooker: 15–18 minutes; gray nightfall) mottled with black and brown. Holds let pressure release gradually. Slow- its shape well; slightly herbaceous- Cooker: 1¹⁄² hours on high, then 6–7 piney in flavor, a little mealy. Lower in hours on low. oligosaccharides. Black-eyed pea West African native, now grown and Soak? Optional. Soaked, Conventional (blaCk-eyes, lobia, loved worldwide. An ivory-white Stovetop: 20–30 minutes. unSoaked, Chawali) cowpea with a black “eye” across Conventional Stovetop: 45–55 minutes. the indentation. Distinctive ashy, Soaked, pressure Cooker: 5–7 minutes. mineral-y taste, starchy texture. unSoaked, pressure Cooker: 9–11 minutes. -

DINNER MENU HUMMUS YOUR WAY DELUXE PLATTERS Served with Three Pitas Deluxe Platers Served with Hummus, Baba Ganough, Tahini Salad, Israeli Salad, Two Pitas
ALLAN’S FALAFEL DINNER MENU HUMMUS YOUR WAY DELUXE PLATTERS Served with three pitas Deluxe platers served with hummus, baba ganough, tahini salad, Israeli salad, two pitas. a choice of rice, red cabbage or fries. Classic Hummus: $6.95 Galit Hummus: $8.95 Allan's Famous Falafel Deluxe Platter: $18 Classic hummus topped with pickles, zatar, paprika, and olive. Our famous ground chickpeas, combined with spices, then formed into small balls. Hummus with Falafel: $9.95 Classic hummus served with falafel. Chicken Cutlet Delux Platter: $20.95 Seasoned chicken breast with onions and peppers, Hummus with Shawarma: $10.95 cooked on the grill. Layers of lamb and turkey, slowly roasted on a vertical grill, sliced thinly, served with classic hummus. Chicken Kebab Delux Platter: $21.95 Chicken cubes on a skewer, cooked on a charcoal grill. Hummus with Chicken Cutlet: $10 Seasoned chicken breast with onions and peppers, Kufta Kebab Delux Platter: $21.95 cooked on a grill, served with classic hummus. Minced ground beef and lamb, seasoned with spices, onion, parsley. APPETIZERS Turkey Shawarma Deluxe Platter: $22.95 Falafel (4 Balls): $3.50 Layers of lamb and turkey, slowly roasted on a vertical Chickpeas ground with parsley, cilantro, spices, formed into roasting grill, served in thin slices. balls and deep fried. - Mixed Grill Deluxe Platter: $26.95 Chicken, shawarma and kufta kebab. Stuffed Grape Leaves: 4 pieces: $5 8 pieces: $8.50 Rice, vegetables, spices, rolled in grape leaves. PLATE ENTREES Tzatziki Dip: small: $5.50 med: $7.50 Plates are served with green salad, hummus, tahini salad, Yogurt, cucumber, olive oil, fresh herbs. -

Livret De Recettes
RESTAURATION SCOLAIRE EXPÉRIMENTATION DU MENU VÉGÉTARIEN LIVRET DE RECETTES CONSEIL NATIONAL DE LA RESTAURATION COLLECTIVE OCTOBRE 2020 LIVRET DE RECETTES – CONSEIL NATIONAL DE LA RESTAURATION COLLECTIVE 1 2 LIVRET DE RECETTES – CONSEIL NATIONAL DE LA RESTAURATION COLLECTIVE Préambule Dans le cadre du Groupe de Travail sur la Nutrition sous l’égide du Conseil National de la Restauration Collective (CNRC), le sous-groupe « recettes et menus » s’est constitué afin d’apporter aux acteurs de la restauration, un outil pratique pour faciliter la mise en œuvre de l’article n° 24 de la Loi EGALIM qui vient compléter « le Guide - Expérimentation du menu végétarien en restauration scolaire ». Guide - Expérimentation du menu végétarien (PDF, 1.97 Mo) https://agriculture.gouv.fr/telecharger/116169?token=88db1e987b4ae08d473c36ba66b9e- da400f70974f564a4bb2d45d5751a08063b Les membres de ce sous-groupe, provenant d’horizons divers se sont réunis à plusieurs reprises afin de concevoir ce document d’informations générales sur les aliments de la cui- sine végétarienne et de proposer une douzaine de recettes réalisables en restauration collec- tive. Les recettes choisies mettent toutes à l’honneur les légumes secs : lentilles, haricots, pois chiches et pois cassés. Nous tenons à remercier Hélène Garcia – gestionnaire des actions de restauration/Conseil départemental de Haute Garonne et Maryline Tosi – Diététicienne à la CDE – Paris 11 qui nous ont aidés dans la rédaction des recettes en vérifiant notamment tous les process et en nous faisant partager leurs -

Ramadan-Kitchen-Survival-2019.Pdf
RAMADAN KAREEM Ramadan is the month of fasting, charity, good deeds, prayer and intense worship for Muslims around the world. It is that time of the year where days seem endless and nights fly by. Ramadan is a season to reflect, control yourself and feel the hardships that many face. Although Ramadan is not intended to be centered around food, it ends up that way. But for us, home cooks, it is always rewarding to see people, especially kids, enjoy our food after a long day of fasting. In this guide, my goal is to help you cook ahead, meal prep and freezer cook for the month so you can enjoy all the spirituality coming your way. FREEZER FRIENDLY RECIPES Your freezer is your best friend during Ramadan. Use your freezer to get ahead of the game. Freezer friendly meals can save time and ease your days especially during weeknights. You'll be surprised at how many things you can freeze. From main, pastry, drinks to desserts and even Suhur meals. Make sure you freeze food in freezer friendly bags or containers. Also do not forget to label food before freezing. Sometimes when food has been frozen it is hard to tell what is in there, trust me I've been there. Here is a list of recipes that you can freeze. DRINKS Follow recipes for drinks as written, add sugar or not it is up to you. Divide liquid among containers according to your family's consumption, label and freeze. When ready to use, just thaw in fridge overnight or even on the countertop during the day. -
Soups & Stews Cookbook
SOUPS & STEWS COOKBOOK *RECIPE LIST ONLY* ©Food Fare https://deborahotoole.com/FoodFare/ Please Note: This free document includes only a listing of all recipes contained in the Soups & Stews Cookbook. SOUPS & STEWS COOKBOOK RECIPE LIST Food Fare COMPLETE RECIPE INDEX Aash Rechte (Iranian Winter Noodle Soup) Adas Bsbaanegh (Lebanese Lentil & Spinach Soup) Albondigas (Mexican Meatball Soup) Almond Soup Artichoke & Mussel Bisque Artichoke Soup Artsoppa (Swedish Yellow Pea Soup) Avgolemono (Greek Egg-Lemon Soup) Bapalo (Omani Fish Soup) Bean & Bacon Soup Bizar a'Shuwa (Omani Spice Mix for Shurba) Blabarssoppa (Swedish Blueberry Soup) Broccoli & Mushroom Chowder Butternut-Squash Soup Cawl (Welsh Soup) Cawl Bara Lawr (Welsh Laver Soup) Cawl Mamgu (Welsh Leek Soup) Chicken & Vegetable Pasta Soup Chicken Broth Chicken Soup Chicken Soup with Kreplach (Jewish Chicken Soup with Dumplings) Chorba bil Matisha (Algerian Tomato Soup) Chrzan (Polish Beef & Horseradish Soup) Clam Chowder with Toasted Oyster Crackers Coffee Soup (Basque Sopa Kafea) Corn Chowder Cream of Celery Soup Cream of Fiddlehead Soup (Canada) Cream of Tomato Soup Creamy Asparagus Soup Creamy Cauliflower Soup Czerwony Barszcz (Polish Beet Soup; Borsch) Dashi (Japanese Kelp Stock) Dumpling Mushroom Soup Fah-Fah (Soupe Djiboutienne) Fasolada (Greek Bean Soup) Fisk och Paprikasoppa (Swedish Fish & Bell Pepper Soup) Frijoles en Charra (Mexican Bean Soup) Garlic-Potato Soup (Vegetarian) Garlic Soup Gazpacho (Spanish Cold Tomato & Vegetable Soup) 2 SOUPS & STEWS COOKBOOK RECIPE LIST Food -

The Importance of Dry Beans in Your Diet August 2005
The Importance of Dry Beans in Your Diet August 2005 The purpose of this lesson is to: Learn more about the nutritional value of dried beans Learn ways to stretch food dollars with dried beans Learn ways to incorporate dried beans, peas, and legumes in family meals Walworth County Association for Home and Community Education Jenny M. Wehmeier Family Living Educator UW-Extension, Walworth County 1 What is a dry bean? Dry beans are produced in pods and belong to the family of plants called legumes. A legume is a plant that produces seeds in a pod (fruit). The physical shape of the seed helps distinguish beans from peas and lentils. Usually, beans are kidney-shaped or oval, peas are round, and lentils are flat disks. Most dry beans grown in this country belong to the species Phaseolus vulgaris, or common bean. The term "dry beans" refers to beans that are dry-packaged in sealed bags and sacks or rehydrated and pre-cooked in cans. Dry beans include popular beans like pinto, navy, kidney (dark and light red), and black beans. Green beans, string beans or soybeans are not considered dry beans. What is the history of the dry bean? Beans have been a staple food for thousands of years. Beans were first domesticated over 7,000 years ago in Peru and southern Mexico. Both centers of domestication have a wide array of colors. In fact, in Mexico, the Indians developed white beans, black beans, and all other colors and color patterns. In the Andes, the same is true, but very lively and bright colors were developed. -
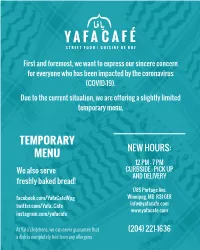
Limited Menu Copy
STREET FOOD | CUISINE DE RUE First and foremost, we want to express our sincere concern for everyone who has been impacted by the coronavirus (COVID-19). Due to the current situation, we are offering a slightly limited temporary menu. TEMPORARY NEW HOURS: MENU 12 PM – 7 PM We also serve CURBSIDE - PICK UP AND DELIVERY freshly baked bread! 1785 Portage Ave. facebook.com/YafaCafeWpg Winnipeg, MB R3J 0E8 twitter.com/Yafa_Cafe [email protected] www.yafacafe.com instagram.com/yafacafe At Yafa’s kitchens, we can never guarantee that (204) 221-1636 a dish is completely free from any allergens اﻟﻤﻘﺒﻼت HOT APPETIZERS اﻟﺴﺎﺧﻨﺔ .All dips are served with one fresh pita bread ﻓﻮل ﻣﺼﺮي ﻣﺪﻣﺲ Foule Mudammas Dip $5 v National Egyptian dish that was made 5,000 years ago and was eaten by the Pharaohs of seasoned mashed fava beans with cumin, garlic, lemon, olive oil. Foule is the Arabic word of fava beans. Vegan option available. ﻗﺪﺳﻴﻪ Qudsiyeh Dip $5 Hummus mixed foule, lemon and olive oil. Prepared the Jerusalemite way. ﺷﻜﺸﻮﻛﻪ Shakshouka $10 v Tunisian dish of sweet smoky tomato, garlic, onions, red peppers, breaking eggs. ﺣﻤﺺ ﺷﺎورﻣﺎ Hummus Shawarma $10 Chickpeas purée with sesame paste, lemon juice and olive oil topped with slices of beef Shawarma, and roasted almonds. ﺑﻮﺗﻴﻦ ﺷﺎورﻣﺎ Poutine Shawarma $13 A remix twist of Canadian Poutine. Soaked in Yafa Gravy and topped with curd cheese, chicken or beef shawarma with vibrant toppings of tahineh and garlic sauce. اﻟﻤﻘﺒﻼت اﻟﺒﺎردة COLD APPETIZERS ﺣﻤﺺ Hummus Dip $5 Chickpeas, lemon, tahini paste (sesame seed), olive oil. -

One Dish Meals.Pdf
contents soups 1 stews 41 braises 81 pastas and baked dishes 109 sautés and stir-fries 139 167 contents light fare index 208 | introduction What is a one dish meal? our first reaction to the title of this book may that we needed to define what we mean by a one dish meal very well be to imagine a large soup pot, sitting on a stove carefully, because we didn’t want to leave anything out. y and bubbling away. We began thinking about some tradi- Cooks have more than one need, and a more complex cu- tional options: stews, braises, hearty soups, and layered pasta linary personality than some books give them credit for. This dishes like lasagna. book accommodates a trusty pot roast that you leave alone in We also took a look around at what everyone else was say- a gentle oven as well as a fiery curry from Thailand that cooks ing about one dish meals and we found a lot of different names in less time than the nightly news. You’ll find dishes that cook for this style of cooking: for hours and dishes that are not “cooked” at all but are simply • Fix it and forget it built, composed, or assembled. As we worked on this book, • Cook once a week (or once a month) we smashed some one dish “myths.” • Meals that make themselves Myth #1: One dish meals are only for cold weather. • Slow cooking • Peasant cooking One dish meals can be served anytime of the year, in any kind • Wash-day cooking of weather. -

CHEZ FRANÇOIS Restaurant Volume 25 Issue 1
Spring 2012 CHEZ FRANÇOIS Restaurant Volume 25 Issue 1 555 Main Street, Vermilion, Ohio 44089 • www.Chezfrancois.com • A publication for friends and guests of Chez François. Dear Friend of Chez François, Thank you for your patronage this past year. We feel blessed to have you as our guest and we look forward to continued success this coming year. Fair, fair...what is all this talk about fairness? Few things are ever truly fair. It seems those who complain about fairness are the ones that don’t really do anything. They never learn that you have to work hard in life, yet feel entitled to many rights they never earned.When in fact, the only right they have in America is the right of Life, Liberty and the pursuit of Happiness. From early childhood we were taught that if you believe in an idea and work hard to execute and have faith in that idea, then you will be successful. It is easy to have an idea, but quite another to commit the time and effort on a daily basis. Inevitably, there will be negative influences along the way and those who will try to criticize, but diligence and persistence guide one through these times. Criticism is fine, as long as it’s constructive and one learns and improves from it, which is what we’ve done for the past 25 years...always striving for improvement in the pursuit of excellence. So if others are more successful than we are, bear in mind it is likely the result of a great deal of time and devotion towards a solid concept and often of great sacrifice too. -

Recipe: Hummus
Hummus Lebanon | Easy | 10 min | 6 servings | Side Dish Tasty Mediterraneo’s Hummus recipe is savoury, creamy and smooth. A healthy vegan and gluten free appetizer rich in fibre and protein. It is perfect served with bread and/or fresh raw vegetables (carrots, peppers…) to dip in. Tools and equipment ~ mortar and pestle ~ food processor Directions Method: 1 If you are using dried chickpeas, to cook them: soak the dried chickpeas in warm water for 12 hours with ⅓ teaspoon of baking soda (ideally leave them soaking overnight). Rinse them well and drain. Bring water to a Ingredients boil in a cooking pot and when the water is boiling add the chickpeas and leave them cooking over low heat for approximately 2 hours until tender. Remove them from the heat, drain and leave them to cool. Reserve the cooking water. If you have forgotten to soak them overnight or you do not have the time to cook them as explained, you • 500g (2 ½ cup) chickpeas, • juice of 2 lemons could use canned organic chickpeas in water (but make sure to rinse them well and drain). cooked (reserve part of the • 3 tablespoon extra-virgin olive 2 Puree the cooked chickpeas in a food processor adding approximately 50ml (3 tablespoons) of the cooking liquid. cooking liquid and a few whole oil for the garnish chickpeas) • 1 bunch parsley 3 Mix the peeled and crushed garlic cloves, the salt and the cumin in a mortar and pestle until you get a paste. Add • 2 garlic cloves, peeled and the tahini and the lemon juice. -

Lynn Take out Menu 2 Sided 05-21
Saturdays & Sundays ful (fūl) $8.75 v fava bean cooked overnight with aromatic spiceswith tomato, cucumber, parsley, onion + pickled egg +$1 our menu is inspired by the bold, labne shakshuka * $9.75 v poached eggs with garlicky labne, mint, SWEETS fresh flavors found in the street foods drizzled with spicy olive oil, zouk, armenian labne bar $5.75 of the Eastern Mediterranean salad, black olives, pickled turnip + sujuk (armenian sausage) $1.50 banana + almond v +lamb meatball $3.50 banana, almond, pinenuts, cinnamon, honey shakshuka * $9.75 v crushed fresh tomatoes, onion with our spices, blueberry + power seeds vNGF blueberries, chia, pumpkin, sunflower topped with black olive, cilantro, poached egg seeds, walnuts, grape molasses + sujuk (armenian sausage) $1.50 +lamb meatball $3.50 mango + chocolate v NGF mango, pistachios, chocolate pearls, kenefe $9.75 v NGF fresh mint, honey crushed filo dough with anoush’ella cheese wrapped with fresh fruit granola v NGF m’anoush with sesame seeds, orange blossom syrup seasonal fresh fruit, our granola, grape molasses mezze for two $28 v shakshuka, ful, za’atar manoush, hummus m’anoush $7.50 anous’ella omellete $7.50 gluten-free bread +$2.50 two eggs, anoush’ella cheese, tomatoes, cucumber, mint, black olives, green onion, pickled turnip, za’atar nutella chocolate vNGF strawberry, banana, cinnamon, honey, granola anoush’ella smores v NGF nutella with graham crackers, marshmallows anoush’ella peanut butter 35 West Newton St. 1205 Market Street Time Out Market v vegetarian NGF not gluten-free with seasonal berries South End - Boston Lynnfield MA Fenway , MA • Please note that we are not a gluten or nut free facility.