Surveillance for European Bat Lyssavirus in Swiss Bats
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Geneva and Region - GVA.CH
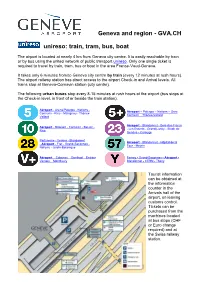
Geneva and region - GVA.CH unireso: train, tram, bus, boat The airport is located at nearly 4 km from Geneva city centre. It is easily reachable by train or by bus using the united network of public transport unireso. Only one single ticket is required to travel by train, tram, bus or boat in the area France-Vaud-Geneva. It takes only 6 minutes from/to Geneva city centre by train (every 12 minutes at rush hours). The airport railway station has direct access to the airport Check-in and Arrival levels. All trains stop at Geneva-Cornavin station (city centre). The following urban buses stop every 8-15 minutes at rush hours at the airport (bus stops at the Check-in level, in front of or beside the train station). Aéroport - Aréna/Palexpo - Nations - Aéroport – Palexpo – Nations – Gare Cornavin - Rive - Malagnou - Thônex- Cornavin – Thônex-Vallard Vallard Aéroport - Blandonnet - Bois-des-Frères Aéroport - Balexert - Cornavin - Bel-Air - - Les Esserts - Grand-Lancy - Stade de Rive Genève - Carouge Parfumerie - Vernier - Blandonnet Aéroport - Blandonnet - Hôpital de la - Aéroport - Fret - Grand-Saconnex - Tour - Meyrin Nations - Jardin-Botanique Aéroport – Colovrex – Genthod – Entrée- Ferney - Grand-Saconnex - Aéroport - Versoix – Montfleury Blandonnet - CERN - Thoiry Tourist information can be obtained at the information counter in the Arrivals hall of the airport, on leaving customs control. Tickets can be purchased from the machines located at bus stops (CHF or Euro change required) and at the Swiss railway station. Travel free on public transport during your stay in Geneva You can pick up a free ticket for public transport from the machine in the baggage collection area at the Arrival level. -

Swiss Schools and Lifestyle Guide
Swiss SCHOOL & LIFESTYLE GUIDE A guide to the educational system in Switzerland and the best locations to live, created in partnership with Carfax Consultants. Welcome letter Switzerland remains one of the world’s most revered and sought after locations and it is no surprise as we explore on page 6; the country is consistently rated strongly for its high standards of living, excellent education, quality of life, a robust and stable economy and favourably low levels of tax, crime and poverty. Private individuals who are drawn by this safe and dependable environment regularly approach Knight Frank to seek our recommendations and guidance from over 12 years working across this market. The Knight Frank Swiss Schools and Lifestyle Guide was developed alongside Carfax Consultants and the collective knowledge from our network of over 13 offices spread strategically throughout the country to provide a comprehensive overview of the top private schools, plus a guide to some of the various lifestyle options available and information on how to purchase. The guide considers both clients seeking permanent residence (see pages 4 & 5) as well as those who desire a holiday home or just to invest in Swiss real estate as a non-resident (see page 12). The Benefits of a Swiss Education (see page 14) offers a unique insight by Carfax Consultants for those not so familiar with the variety of options on offer. The experience that Carfax can provide to help clients place their children within the right school is paramount to a successful relocation. We hope you find the information useful and if you have any questions, or wish to find out more about how our team can help you find your dream home, with great educational options close by, please get in touch. -

Cham'art Organise Une Exposition Au Grand
Lundi 17 mai 2021 Sommaire Bellevue Tribune Journal des communes Un vieux chêne casse 2 d’Anières, Bellevue, Choulex, Anières Recyclez vos vélos! 3 Cologny, Corsier, Genthod, Cologny Hermance, Meinier, Des Unes au musée 4 Pregny-Chambésy Rives-Lac Editeur: La Tribune de Genève SA. Rédactrice responsable: Stéphanie Jousson. Prochaine parution: [email protected] Tél. 022 733 40 31 Lundi 7 juin Pregny-Chambésy accueille cette année Le covoiturage semble la deuxième étape du Tour du Canton de Genève avoir de l’avenir à Meinier On va courir pendant un l’édition 2021. La Commune de au 20 juin. Les participants pour- également prévu une catégorie qui Une nouvelle association seuls à aller faire leurs courses, mois sur les chemins Pregny-Chambésy a décidé de ront télécharger une application s’adresse aux marcheurs. est née dans notre village. deux amis y aillent ensemble. de la commune. maintenir son engagement en qui leur permettra durant un mois Attention au nombre de Les coûts de consommation de accueillant la deuxième étape, – en respectant les dates du tour – places limitées. Si l’événement C’est l’histoire de trois voisins, la voiture sont évalués et gérés bé- La course du Tour du Canton de comme prévu en 2020. de réaliser cette course pédestre ac- sportif devait être annulé due à d’amis, qui réalisent ne pas névolement par une comptable. Genève ayant été annulée l’an- tive sur notre canton depuis vingt- la situation sanitaire, les frais avoir besoin de leur voiture ré- Un pécule est aussi mis de côté née dernière pour des raisons Inscriptions six ans. -

LA MARCHE DU CAD Dimanche 29 Septembre 2019
CAO 9 ACCÈS Actions Seniors TPG : Route de la Chapelle 22 Bachet-de-Pesay Dimanche 29 LA MARCHE 1212 Grand-Lancy lignes 12, 18, 23, 42, 43, 46, 62 et D septembre 2019 DU CAO 022 420 42 80 Préventorium, ligne 43 CAD ACTIONS SENIORS cadra hospicegeneral.ch www.cad-ge.ch Merci de privilégier les transports publics 1 Horaires : 8h30- 17h30 LA MARCHE DU CAD Dimanche 29 septembre 2019 Q) Dès 8h30 :Marches > .Q) c 12h00 :Arrivée au CAO avec la fanfare du Château Q) (9 Q) -o 12h20 : Partie officielle c .8 12h30 :Saucisse et salades offertes aux marcheurs c rn u â) Q) .,.-::J :0 ::J " •Q) 0:: ~ Q) -o c <1! ::J 0 V) ~ u Q) k-~~~ ~~--~----~ ~ PLAINPHIVANT Ki~ ü /loio ,olo io/ om in ltltiu el! (j) t ~ -"l ()_ E Q) >< Q) ::-w âge -:<i,c --A- C) _g _ ~ ~~~~~~ C) C) "' o- - ~ C) N Mieux vivre ~ 0 CJ Hospice général L.:Airedesseniors Commission des Aînés Club des aînés Conseil des Anciens 0 Perly Aire laville Carouge <( 1 deTroinex' ® ensemble à Genève , 9. CAROUGE 12. ACACIAS DEPARTS Départ 9 : 11hOO Départ 12 : 1OhOO Du rée de la marche: 1 hOO Du rée de la marche: 2h00 min. POUR S'INSCRIRE Inscriptions :022 420 42 80 Inscriptions: 022 304 04 02 CAO et Club des Aînés, Carouge Seniors d'ici et d'ailleurs- Croix-Rouge Les inscriptions se font directement auprès des associations partenaires entre le 2 et le 20 septembre 2019. Parmi les propositions ci-contre, choisissez votre Genevoise lieu de départ et appelez directement le numéro indiqué pour avoir les informa 10. -

Chêne En Mouvement Riés
Agenda des 3-Chêne inclus! Fondé en 1915 Février 2020 • n° 543 Sommaire Avis 2 Dossier 4 Actualités 14 Informations officielles 17 Vie associative 50 Sports & Loisirs 52 Pêle-mêle 55 Chêne-Bougeries La Commune fête cette année les 50 ans d'Editart, avec une exposition au Nouveau Vallon. Ce sera l'occasion pour le public chênois de décou- vrir ou de redécouvrir l'activité extraordi- naire déployée par ses fondateurs, Orlando et Dolores Blanco qui vous feront vivre à travers les œuvres et les textes exposés, les moments de grâce qu'ils ont connus avec les plus grands maîtres et poètes du XXe siècle. Voir en p. 23 Chêne-Bourg La saison culturelle s'affi che dans les pages communales avec plus d'une dizaine de spectacles va- Chêne en mouvement riés. Humour, musique, cinéma, En ce début d'année 2020, le Léman Express est sur toutes les lèvres. Son arrivée à Chêne-Bourg a été sa- danse, théâtre, etc., des artistes de tout horizon vous donnent rendez- luée par les habitants et les Autorités. On peut également voir circuler le tram 17 dans les rues chênoises vous sur la scène du Point favre avec pour et certaines lignes de bus ont été modifi ées. Se pose alors la question des titres de transport : quel billet seul but de vous divertir. Vous n'aurez que l'embarras du choix ! Voir en pp. 34-35 prendre pour quel trajet ? Existe-t-il une application qui facilite votre mobilité ? Dans notre dossier du mois, Laura Etienne a mené l'enquête et vous donne toutes les réponses que les Chênois sont en mesure Thônex de se poser pour leurs déplacements quotidiens en transports publics. -

Map of Fare Zone
Fares Public transport for Geneva Map of Fare Zone as of Dec. 15 2019 Évian-les-Bains Plan tarifaire 300 L1 Thonon-les-Bains Légende Legend Toward Lausanne LignesTrain lines ferroviaires Lac Léman Perrignier Coppet LignesBus and de tram bus etlines tram Chens-sur-Léman LignesTransalis Transalis lines L1 L2 L3 L4 RE Gex Tannay LignesLacustre navettes shuttle lacustre lines Hermance-Village Customs Veigy-Foncenex, Les Cabrettes Bons-en-Chablais Divonne-les-Bains Mies PassageZone crossing de zone Chavannes-des-Bois Hermance Veigy-Foncenex ZoneLéman Léman Pass Pass zones Veigy- Veigy-Village Bois-Chatton Versoix Zoneunireso 10 zoneunireso 10 Pont-Céard Douane 200 Machilly Collex-Bossy Versoix Anières Customs Gy 250 Customs Bossy Genthod Creux-de-Genthod Anières-Douane Corsier Meinier Jussy St-Genis-Pouilly Ferney-Douane Genthod-Bellevue Bellevue Customs Grand-Saconnex-Douane Collonge-Bellerive Ferney-Bois Candide Les Tuileries Customs Le Grand-Saconnex Mategnin Chambésy Choulex Meyrin-Gravière Pregny- Chambésy 10 Genève-Aéroport Genève-Sécheron Vésenaz Presinge Customs Meyrin L1 Saint-Genis-Porte de France L2 Vandœuvre Meyrin L3 CERN 10 De-Chateaubriand Puplinge Thoiry Vernier L4 RE Ville-la-Grand Vernier Gare de Genève Pâquis Port-Noir Zimeysa Chêne-Bourg Annemasse Satigny Ambilly Eaux-Vives Chêne-Bougeries Genève Annemasse Satigny Gaillard- Molard Chêne-Bourg Customs Libération L1 L2 L3 L4 RE Etrembières Le Rhône 10 Genève-Eaux-Vives Moillesulaz 240 Russin Genève-Champel Gaillard 210 Lancy-Pont-Rouge Thônex Russin Dardagny Onex Challex -

Compte Rendu 2019
RÉPUBLIQUE ET CANTON DE GENÈVE GENTHOD COMPTE RENDU DE L’ADMINISTRATION MUNICIPALE | 2019 Une invitation à prendre place un moment et apprécier d’être au cœur du village MESSAGE DU MAIRE 2 ADMINISTRATION | GESTION DU PERSONNEL | AMÉNAGEMENT DU TERRITOIRE ET MOBILITÉ | ÉTAT CIVIL | CIMETIÈRE | FINANCES BÂTIMENTS 6 AFFAIRES SOCIALES ET NATURALISATIONS | CULTURE, SPORTS ET LOISIRS | SCOLAIRE 10 SÉCURITÉ PUBLIQUE | GÉNIE CIVIL | ENVIRONNEMENT 12 SÉANCES DU CONSEIL MUNICIPAL 15 BILAN DES COMMISSIONS SUR L’ANNÉE 2019 27 ET PENDANT CE TEMPS À GENTHOD 36 BILAN DES SOCIÉTÉS COMMUNALES 37 BILAN DES GROUPEMENTS COMMUNAUX 48 RAPPORT FINANCIER 2019 51 ÉLÉMENTS STATISTIQUES 58 RENSEIGNEMENTS UTILES 60 GENTHOD PRATIQUE 63 RECOMMANDATIONS 66 PLAN DE LA COMMUNE 68 AUTORITÉS MUNICIPALES 70 RÉPUBLIQUE ET CANTON DE GENÈVE GENTHOD COMPTE RENDU DE L’ADMINISTRATION MUNICIPALE | 2019 MESSAGE DU MAIRE Chères citoyennes, chers citoyens, Mesdames, Messieurs, Conformément à la loi cantonale du 18 avril 1984 sur l’administration des communes, plus connue sous l’abréviation “la LAC”, nous vous présentons le rapport administratif et financier couvrant la période du 1er janvier au 31 décembre 2019. L’année 2019 fut, malgré quelques nuages passagers, une année passionnante et riche en événements. Il est réjouissant que le nombre d’habitants de la commune et des élèves qui fréquentent notre école se soit de nouveau accru après de longues années de stag- nation. Un renouvellement au moins modéré est essentiel pour une commune comme la nôtre; le monde de demain appartient aux enfants d’aujourd’hui. Voici les événements les plus marquants, dont certains seront abordés plus loin: > la nouvelle ligne TPG; > le succès dans les urnes de l’initiative “pour un pilotage démocratique de l’aéroport”; > l’introduction officielle du Léman Express avec sa cadence soutenue et son effet limité sur la densification des constructions de notre commune; > le rapport musclé de la Cour des Comptes; > l’échéance des droits de superficie au bord du lac; > le changement de propriétaire du restaurant Le Lacustre. -

Here's the Least Expensive Place to Live
Investment Solutions & Products Swiss Economics Here’s the least expensive place to live Financial residential attractiveness| May 2021 Financial residential attractiveness RDI indicator 2021 Results for your household What's left after subtracting all mandatory Life in the city centers is expensive, but there are Here’s the least expensive place for you to live charges and fixed costs? often more attractive municipalities close by Page 9 Page 29 Page 46 Masthead Publisher: Credit Suisse AG, Investment Solutions & Products Dr. Nannette Hechler-Fayd'herbe Head of Global Economics & Research +41 44 333 17 06 nannette.hechler-fayd'[email protected] Dr. Sara Carnazzi Weber Head of Policy & Thematic Economics +41 44 333 58 82 [email protected] Editorial deadline May 4, 2021 Orders Electronic copies via credit-suisse.com/rdi Copyright The publication may be quoted provided the source is identified. Copyright © 2021 Credit Suisse Group AG and/or affiliate companies. All rights reserved. Source references Credit Suisse unless specified Authors Dr. Jan Schüpbach +41 44 333 77 36 [email protected] Emilie Gachet +41 44 332 09 74 [email protected] Pascal Zumbühl +41 44 334 90 48 [email protected] Dr. Sara Carnazzi Weber +41 44 333 58 82 [email protected] Contributions Fabian Diergardt Thomas Mendelin Marcin Jablonski Swiss Economics | Financial residential attractiveness 2021 2 Editorial Dear readers, For many people, choosing where to live is one of the most important decisions in life. In addition to geographical location and infrastructure, the availability of appropriate housing, emotional criteria and personal networks, financial factors also play a key role. -

WELCOME to GENEVA Practical Guide to Living in Geneva Anglais
WELCOME TO GENEVA PRACTICAL GUIDE TO LIVING IN GENEVA ANGLAIS REPUBLIQUE ET CANTON DE GENEVE Geneva : 45 communes al Aire-la-Ville co Gy am Anières cp Hermance an Avully cq Jussy ao Avusy cr Laconnex ap Bardonnex cs Ville de Lancy aq Bellevue ct Meinier ar Bernex dk Meyrin as Ville de Carouge dl Onex at Cartigny dm Perly Certoux bk Céligny dn Plan-les-Ouates bl Chancy do Pregny Chambesy bm Chêne-Bougeries dp Presinge bn Chêne-Bourg dq Puplinge bo Choulex dr Russin bp Collex-Bossy ds Satigny bq Collonge-Bellerive dt Soral br Cologny ek Thônex bs Confi gnon el Troinex bt Corsier em Vandoeuvres ck Dardagny en Vernier cl Genève eo Versoix cm Genthod ep Veyrier cn Grand-Saconnex IF YOU HAVE DIFFICULTY READING THESE TEXTS, A LARGE FORMAT (A4) VERSION IS AVAILABLE ON : www.ge.ch/integration/publications OR BY CONTACTING THE OFFICE FOR INTEGRATION OF FOREIGNERS, al RUE PIERRE FATIO 15 (4th FLOOR) 1204 GENEVA TEL. 022 546 74 99 FAX. 022 546 74 90 www.ge.ch/integration [email protected] 2 WELCOME TO GENEVA - MESSAGE On behalf of the Council of State of the Canton of Geneva and the Association of Geneva Communes (ACG) we wish you a very warm welcome. Geneva has been a place of asylum and refuge for victims of religious persecution since the 16th century and has always been conscious of the richness of its multicultural society and convinced that it is one of its major strengths which favours exchange, dialogue and creativity. In order to promote this cultural richness, symbolised by the presence of 194 nationalities in Geneva, the canton and the communes deploy a great effort to encourage integration, intercultural dialogue and respect for minorities. -

Le Bicyclologue D'anières Nous Rend Parfois Visite
Lundi 22 mars 2021 Sommaire Hermance Tribune Journal des communes Retraite bien méritée 2 d’Anières, Bellevue, Choulex, Bellevue Les enfants s’activent 3 Cologny, Corsier, Genthod, Corsier Hermance, Meinier, Transition assurée 4 Pregny-Chambésy Rives-Lac Editeur: La Tribune de Genève SA. Rédactrice responsable: Stéphanie Jousson. Prochaine parution: [email protected] Tél. 022 733 40 31 Lundi 26 avril Nouveau titre pour notre jeune rameuse La soirée publique 2021 de hermançoise, une belle récompense Pregny-Chambésy aura lieu le 25 mars Sophia Meakin est Elle sera différente mais se tiques. La soirée se poursuivait au- conviés le jeudi 25 mars à 19 h, à championne suisse! veut toujours proche des tour d’un buffet et les discussions assister depuis chez eux à la soi- habitants! continuaient. rée publique, qui sera transmise Après un hiver très difficile, un Cette année, il n’en sera pas de en web streaming sur la chaîne long Covid l’ayant obligée à rester Habituellement, les habitants de même. Il est à noter que l’Exécu- YouTube communale. un mois sans entraînement, et Pregny-Chambésy se retrouvaient tif de Pregny-Chambésy aurait pu Pour celles et ceux qui ne sau- après deux mois de réadaptation, dans la salle communale pour as- annuler la soirée publique, raient pas comment faire, rien de Sofia Meakin, notre championne sister à leur soirée publique. comme cela avait été le cas en plus simple. hermançoise et médaillée d’or en Sophia Meakin. JEAN-MICHEL BILLY Après la présentation par les 2020, de par la situation sani- Un peu avant 19 h, connec- 2019 avec sa coéquipière Éline membres de l’Exécutif de leur di- taire. -
Innovation in Public Transportation
TPG and Innovation for a Smart Region Anne Hornung-Soukup Chair of the Board of Directors Transports publics genevois (tpg) Day of Cities, UNECE - April 9th, 2019 History of TPG Geneva Mass Transit Milestones and Eras 19th Century – Innovation 1833 First omnibus launched 1862 First horse-drawn tramway line Line 12: historic, oldest still operating in Europe 1878 First steam-powered tram 1896 First electric tram 20th Century – Wars and Cars 1920 Peak of Geneva tram lines Place de Neuve, 1894 1977 Takeover by the State of Geneva 21st Century – Renewed Growth State of the company today Facts and figures 217 million passengers/year 700’000/day during work week 28 million km covered More than 70’000 km/day or twice circumference of earth 63 lines 1959 employees (12% woman) of whom almost 1200 drivers 440 vehicles (50% electric) 237 buses, 92 trolleybuses, 111 trams 7 days per week, 23 hours per day Source: annual report 2017 Client experience Overall satisfaction with public transport – Geneva first in Europe Source: BEST Survey 2017 HSBC 2017 Expat Study: Geneva-based expats consider local public transport reliable and convenient Sustainable cities reduce congestion Most efficient way = Encourage mass transit Geneva Canton Population: 501,748 (2018) 576,000 to 625,000 (2040) Commuters from France to Geneva/day: 109,972 Percent commuters from France in cars: More than 90% 70 people on the left, 70 people on the right Sustainable mobility for smart cities Tpg is actively developing innovative products/systems Sustainable development Virtual reality Automatisation TOSA flash-charging bus Drivers training Driverless vehicles Digital transformation Application programming Multimodality Comm tpgPay Interface – tpg Lab ZenGo Tetra radio In addition to ongoing innovation Three Major Events on December 15th, 2019 1. -

List of Participants
UNECE Regional Preparatory Meeting for Rio+20 SALLE XVIII Palais des Nations, Geneva 1–2 December 2011 List of participants as of 8 December 2011 (Please, make corrections, as appropriate, and send them to [email protected]. Thank you.) 1 UNECE Regional Preparatory Meeting for UNCSD - Rio+20 Start Date: 01 Dec 2011 End Date: 02 Dec 2011 List of participants (as of 8 December 2011) Number of Persons: 416 GOVERNMENTAL DELEGATIONS .....................................................................................................3 GOVERNMENTAL DELEGATIONS - UN MEMBER STATES OUTSIDE THE ECE ................22 EUROPEAN UNION .............................................................................................................................22 UN ORGANIZATIONS AND SPECIALIZED AGENCIES............................................................23 INTERGOVERNMENTAL ORGANIZATIONS ................................................................................33 REGIONAL ENVIRONMENTAL CENTERS ....................................................................................34 MAJOR GROUPS ..................................................................................................................................35 Business & Industry ......................................................................................................................35 Children & Youth ............................................................................................................................38 Farmers ..............................................................................................................................................38