Durham E-Theses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
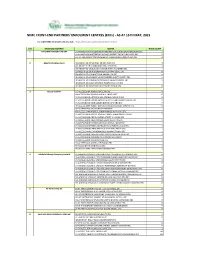
NIMC FRONT-END PARTNERS' ENROLMENT CENTRES (Ercs) - AS at 15TH MAY, 2021
NIMC FRONT-END PARTNERS' ENROLMENT CENTRES (ERCs) - AS AT 15TH MAY, 2021 For other NIMC enrolment centres, visit: https://nimc.gov.ng/nimc-enrolment-centres/ S/N FRONTEND PARTNER CENTER NODE COUNT 1 AA & MM MASTER FLAG ENT LA-AA AND MM MATSERFLAG AGBABIAKA STR ILOGBO EREMI BADAGRY ERC 1 LA-AA AND MM MATSERFLAG AGUMO MARKET OKOAFO BADAGRY ERC 0 OG-AA AND MM MATSERFLAG BAALE COMPOUND KOFEDOTI LGA ERC 0 2 Abuchi Ed.Ogbuju & Co AB-ABUCHI-ED ST MICHAEL RD ABA ABIA ERC 2 AN-ABUCHI-ED BUILDING MATERIAL OGIDI ERC 2 AN-ABUCHI-ED OGBUJU ZIK AVENUE AWKA ANAMBRA ERC 1 EB-ABUCHI-ED ENUGU BABAKALIKI EXP WAY ISIEKE ERC 0 EN-ABUCHI-ED UDUMA TOWN ANINRI LGA ERC 0 IM-ABUCHI-ED MBAKWE SQUARE ISIOKPO IDEATO NORTH ERC 1 IM-ABUCHI-ED UGBA AFOR OBOHIA RD AHIAZU MBAISE ERC 1 IM-ABUCHI-ED UGBA AMAIFEKE TOWN ORLU LGA ERC 1 IM-ABUCHI-ED UMUNEKE NGOR NGOR OKPALA ERC 0 3 Access Bank Plc DT-ACCESS BANK WARRI SAPELE RD ERC 0 EN-ACCESS BANK GARDEN AVENUE ENUGU ERC 0 FC-ACCESS BANK ADETOKUNBO ADEMOLA WUSE II ERC 0 FC-ACCESS BANK LADOKE AKINTOLA BOULEVARD GARKI II ABUJA ERC 1 FC-ACCESS BANK MOHAMMED BUHARI WAY CBD ERC 0 IM-ACCESS BANK WAAST AVENUE IKENEGBU LAYOUT OWERRI ERC 0 KD-ACCESS BANK KACHIA RD KADUNA ERC 1 KN-ACCESS BANK MURTALA MOHAMMED WAY KANO ERC 1 LA-ACCESS BANK ACCESS TOWERS PRINCE ALABA ONIRU STR ERC 1 LA-ACCESS BANK ADEOLA ODEKU STREET VI LAGOS ERC 1 LA-ACCESS BANK ADETOKUNBO ADEMOLA STR VI ERC 1 LA-ACCESS BANK IKOTUN JUNCTION IKOTUN LAGOS ERC 1 LA-ACCESS BANK ITIRE LAWANSON RD SURULERE LAGOS ERC 1 LA-ACCESS BANK LAGOS ABEOKUTA EXP WAY AGEGE ERC 1 LA-ACCESS -
P E E L C H R Is T Ian It Y , Is L a M , an D O R Isa R E Lig Io N
PEEL | CHRISTIANITY, ISLAM, AND ORISA RELIGION Luminos is the open access monograph publishing program from UC Press. Luminos provides a framework for preserving and rein- vigorating monograph publishing for the future and increases the reach and visibility of important scholarly work. Titles published in the UC Press Luminos model are published with the same high standards for selection, peer review, production, and marketing as those in our traditional program. www.luminosoa.org Christianity, Islam, and Orisa Religion THE ANTHROPOLOGY OF CHRISTIANITY Edited by Joel Robbins 1. Christian Moderns: Freedom and Fetish in the Mission Encounter, by Webb Keane 2. A Problem of Presence: Beyond Scripture in an African Church, by Matthew Engelke 3. Reason to Believe: Cultural Agency in Latin American Evangelicalism, by David Smilde 4. Chanting Down the New Jerusalem: Calypso, Christianity, and Capitalism in the Caribbean, by Francio Guadeloupe 5. In God’s Image: The Metaculture of Fijian Christianity, by Matt Tomlinson 6. Converting Words: Maya in the Age of the Cross, by William F. Hanks 7. City of God: Christian Citizenship in Postwar Guatemala, by Kevin O’Neill 8. Death in a Church of Life: Moral Passion during Botswana’s Time of AIDS, by Frederick Klaits 9. Eastern Christians in Anthropological Perspective, edited by Chris Hann and Hermann Goltz 10. Studying Global Pentecostalism: Theories and Methods, by Allan Anderson, Michael Bergunder, Andre Droogers, and Cornelis van der Laan 11. Holy Hustlers, Schism, and Prophecy: Apostolic Reformation in Botswana, by Richard Werbner 12. Moral Ambition: Mobilization and Social Outreach in Evangelical Megachurches, by Omri Elisha 13. Spirits of Protestantism: Medicine, Healing, and Liberal Christianity, by Pamela E. -

Boko Haram Beyond the Headlines: Analyses of Africa’S Enduring Insurgency
Boko Haram Beyond the Headlines: Analyses of Africa’s Enduring Insurgency Editor: Jacob Zenn Boko Haram Beyond the Headlines: Analyses of Africa’s Enduring Insurgency Jacob Zenn (Editor) Abdulbasit Kassim Elizabeth Pearson Atta Barkindo Idayat Hassan Zacharias Pieri Omar Mahmoud Combating Terrorism Center at West Point United States Military Academy www.ctc.usma.edu The views expressed in this report are the authors’ and do not necessarily reflect those of the Combating Terrorism Center, United States Military Academy, Department of Defense, or U.S. Government. May 2018 Cover Photo: A group of Boko Haram fighters line up in this still taken from a propaganda video dated March 31, 2016. COMBATING TERRORISM CENTER ACKNOWLEDGMENTS Director The editor thanks colleagues at the Combating Terrorism Center at West Point (CTC), all of whom supported this endeavor by proposing the idea to carry out a LTC Bryan Price, Ph.D. report on Boko Haram and working with the editor and contributors to see the Deputy Director project to its rightful end. In this regard, I thank especially Brian Dodwell, Dan- iel Milton, Jason Warner, Kristina Hummel, and Larisa Baste, who all directly Brian Dodwell collaborated on the report. I also thank the two peer reviewers, Brandon Kend- hammer and Matthew Page, for their input and valuable feedback without which Research Director we could not have completed this project up to such a high standard. There were Dr. Daniel Milton numerous other leaders and experts at the CTC who assisted with this project behind-the-scenes, and I thank them, too. Distinguished Chair Most importantly, we would like to dedicate this volume to all those whose lives LTG (Ret) Dell Dailey have been afected by conflict and to those who have devoted their lives to seeking Class of 1987 Senior Fellow peace and justice. -

Maiduguri: City Scoping Study
MAIDUGURI: CITY SCOPING STUDY By Marissa Bell and Katja Starc Card (IRC) June 2021 MAIDUGURI: CITY SCOPING STUDY 2 Maiduguri is the largest city in north east Nigeria and the capital of Borno State, which suffers from endemic poverty, and capacity and legitimacy gaps in terms of its governance. The state has been severely affected by the Boko Haram insurgency and the resulting insecurity has led to economic stagnation in Maiduguri. The city has borne the largest burden of support to those displaced by the conflict. The population influx has exacerbated vulnerabilities that existed in the city before the security and displacement crisis, including weak capacities of local governments, poor service provision and high youth unemployment. The Boko Haram insurgency appears to be attempting to fill this gap in governance and service delivery. By exploiting high levels of youth unemployment Boko Haram is strengthening its grip around Maiduguri and perpetuating instability. Maiduguri also faces severe environmental challenges as it is located in the Lake Chad region, where the effects of climate change increasingly manifesting through drought and desertification. Limited access to water and poor water quality is a serious issue in Maiduguri’s vulnerable neighborhoods. A paucity of drains and clogging leads to annual flooding in the wet season. As the population of Maiduguri has grown, many poor households have been forced to take housing in flood-prone areas along drainages due to increased rent prices in other parts of the city. URBAN CONTEXT Maiduguri is the oldest town in north eastern Nigeria and has long served as a commercial centre with links to Niger, Cameroon and Chad and to nomadic communities in the Sahara. -

Kanembu-Kaniri Relationship
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Hochschulschriftenserver - Universität Frankfurt am Main Berichte des Sonderforschungsbereichs 268, Band 8, Frankfurt a.M. 1996: 37-47 KANEMBU-KANURI RELATIONSHIP: A PROPOSAL1 Shettima Umara Bulakarima Abstract The paper takes recourse to oral tradition and linguistics to ascertain the assertion that the present-day Kanuri and Kanembu speech forms emerged from the same parent language. In determining the parent language, the descriptions of the various components (i.e. clans and ethnic groups) of Kanuri and Kanembu are given as a first basis and the relation of each dialect of Kanuri and Kanembu to the other (i.e. dialect contiguity) is demonstrated as a second basis. Taking into consideration the sociolinguistic background of both Kanuri and Kanembu, the brief history of their divergence, the strong contention of the Borno Ulama and the dialect contiguity of the data presented, the paper concludes that Kanuri and Kanembu are initially one and the same language with ancient classical Kanembu being the parent language. Kanembu-Kanuri relationship: a proposal Introduction The close genetic relationship of a group of languages referred to as Saharan, was recognised about one and a half centuries ago. This was evident in BARTH (1965), NACHTIGAL (1987), LUKAS (1951), TUCKER and BRYAN (1956), GREENBERG (1966) and CYFFER (1981, 1990, 1991). Based on the genetic classification model of LUKAS (1951), GREENBERG (1966), PETRACEK (1966, 1978 and 1979) and CYFFER (1981 and 1990), the Saharan languages can be modelled as fig. 1 below. 1 I am grateful to the following colleagues for their academic criticisms/contributions which brought the paper to its present stage: A. -
Inequality and Development in Nigeria Inequality and Development in Nigeria
INEQUALITY AND DEVELOPMENT IN NIGERIA INEQUALITY AND DEVELOPMENT IN NIGERIA Edited by Henry Bienen and V. P. Diejomaoh HOLMES & MEIER PUBLISHERS, INC' NEWv YORK 0 LONDON First published in the United States of America 1981 by Holmes & Meier Publishers, Inc. 30 Irving Place New York, N.Y. 10003 Great Britain: Holmes & Meier Publishers, Ltd. 131 Trafalgar Road Greenwich, London SE 10 9TX Copyright 0 1981 by Holmes & Meier Publishers, Inc. ALL RIGIITS RESERVIED LIBRARY OF CONGRESS CATALOGING IN PUBLICATION DATA Political economy of income distribution in Nigeria. Selections. Inequality and development in Nigeria. "'Chapters... selected from The Political economy of income distribution in Nigeria."-Pref. Includes index. I. Income distribution-Nigeria-Addresses, essays, lectures. 2. Nigeria- Economic conditions- Addresses. essays, lectures. 3. Nigeria-Social conditions- Addresses, essays, lectures. I. Bienen. Henry. II. Die jomaoh. Victor P., 1940- III. Title. IV. Series. HC1055.Z91516 1981 339.2'09669 81-4145 LIBRARY OF CONGRESS CATALOGING IN PUBLICATION DATA ISBN 0-8419-0710-2 AACR2 MANUFACTURED IN THE UNITED STATES OF AMERICA Contents Page Preface vii I. Introduction 2. Development in Nigeria: An Overview 17 Douglas Riummer 3. The Structure of Income Inequality in Nigeria: A Macro Analysis 77 V. P. Diejomaoli and E. C. Anusion wu 4. The Politics of Income Distribution: Institutions, Class, and Ethnicity 115 Henri' Bienen 5. Spatial Aspects of Urbanization and Effects on the Distribution of Income in Nigeria 161 Bola A veni 6. Aspects of Income Distribution in the Nigerian Urban Sector 193 Olufemi Fajana 7. Income Distribution in the Rural Sector 237 0. 0. Ladipo and A. -

An Analysis of What Works and What Doesn't
Radicalisation and Deradicalisation in Nigeria: An Analysis of What Works and What Doesn’t Nasir Abubakar Daniya i Radicalisation and Deradicalisation in Nigeria: An Analysis of What Works and What Doesn’t. Nasir Abubakar Daniya Student Number: 13052246 A Thesis Submitted in Fulfilment of Requirements for award of: Professional Doctorate Degree in Policing Security and Community Safety London Metropolitan University Faculty of Social Science and Humanities March 2021 Thesis word count: 104, 482 ii Abstract Since Nigeria’s independence from Britain in 1960, the country has made some progress while also facing some significant socio-economic challenges. Despite being one of the largest producers of oil in the world, in 2018 and 2019, the Brooking Institution and World Poverty Clock respectively ranked Nigeria amongst top three countries with extreme poverty in the World. Muslims from the north and Christians from the south dominate the country; each part has its peculiar problem. There have been series of agitations by the militants from the south to break the country due to unfair treatments by the Nigerian government. They produced multiple violent groups that killed people and destroyed properties and oil facilities. In the North, an insurgent group called Boko Haram emerges in 2009; they advocated for the establishment of an Islamic state that started with warning that, western education is prohibited. Reports say the group caused death of around 100,000 and displaced over 2 million people. As such, Niger Delta Militancy and Boko Haram Insurgency have been major challenges being faced by Nigeria for about a decade. To address such challenges, the Nigerian government introduced separate counterinsurgency interventions called Presidential Amnesty Program (PAP) and Operation Safe Corridor (OSC) in 2009 and 2016 respectively, which are both aimed at curtailing Militancy and Insurgency respectively. -

Unclaimed-Dividend202047.Pdf
UNCLAIMED DIVIDENDS 1 (HRH OBA) GABRIEL OLATERU ADEWOYE 140 ABDULLAHI AHMED 279 ABIGAL ODUNAYO LUCAS 418 ABOSEDE ADETUTU ORESANYA 2 (NZE) SUNDAY PAUL EZIEFULA 141 ABDULLAHI ALIU ADAMU 280 ABIGALIE OKUNWA OKAFOR 419 ABOSEDE AFOLAKEMI IBIDAPO-OBE 3 A A J ENIOLA 142 ABDULLAHI AYINLA ABDULRAZAQ 281 ABIJO AYODEJI ADEKUNLE 420 ABOSEDE BENEDICTA ONAKOYA 4 A A OYEGBADE 143 ABDULLAHI BILAL FATSUMA 282 ABIJOH BALIKIS ADESOLA 421 ABOSEDE DUPE ODUMADE 5 A A SIJUADE 144 ABDULLAHI BUKAR 283 ABIKE OTUSANYA 422 ABOSEDE JEMILA IBRAHIM 6 A BASHIR IRON BABA 145 ABDULLAHI DAN ASABE MOHAMMED 284 ABIKELE GRACE 423 ABOSEDE OLAYEMI OJO 7 A. ADESIHMA FAJEMILEHIN 146 ABDULLAHI DIKKO KASSIM (ALH) 285 ABIMBADE ATANDA WOJUADE 424 ABOSEDE OLUBUNMI SALAU (MISS) 8 A. AKINOLA 147 ABDULLAHI ELEWUETU YAHAYA (ALHAJI) 286 ABIMBOLA ABENI BAMGBOYE 425 ABOSEDE OMOLARA AWONIYI (MRS) 9 A. OLADELE JACOB 148 ABDULLAHI GUNDA INUSA 287 ABIMBOLA ABOSEDE OGUNNIEKAN 426 ABOSEDE OMOTUNDE ABOABA 10 A. OYEFUNSO OYEWUNMI 149 ABDULLAHI HALITA MAIBASIRA 288 ABIMBOLA ALICE ALADE 427 ABOSI LIVINUS OGBUJI 11 A. RAHMAN BUSARI 150 ABDULLAHI HARUNA 289 ABIMBOLA AMUDALAT BALOGUN 428 ABRADAN INVESTMENTS LIMITED 12 A.A. UGOJI 151 ABDULLAHI IBRAHIM RAIYAHI 290 ABIMBOLA AREMU 429 ABRAHAM A OLADEHINDE 13 AAA STOCKBROKERS LTD 152 ABDULLAHI KAMATU 291 ABIMBOLA AUGUSTA 430 ABRAHAM ABAYOMI AJAYI 14 AARON CHIGOZIE IDIKA 153 ABDULLAHI KURAYE 292 ABIMBOLA EKUNDAYO ODUNSI (MISS) 431 ABRAHAM ABU OSHIAFI 15 AARON IBEGBUNA AKABIKE 154 ABDULLAHI MACHIKA OTHMAN 293 ABIMBOLA FALI SANUSI-LAWAL 432 ABRAHAM AJEWOLE ARE 16 AARON M AMAK DAMAK 155 ABDULLAHI MAILAFIYA ABUBAKAR 294 ABIMBOLA FAUSAT ADELEKAN 433 ABRAHAM AJIBOYE OJEDELE 17 AARON OBIAKOR 156 ABDULLAHI MOHAMMED 295 ABIMBOLA FEHINTOLA 434 ABRAHAM AKEJU OMOLE 18 AARON OLUFEMI 157 ABDULLAHI MOHAMMED ABDULLAHI 296 ABIMBOLA KEHINDE OLUWATOYIN 435 ABRAHAM AKINDELE TALABI 19 AARON U. -

Interrogating Godfathers
Journal of Sustainable Development in Africa (Volume 19, No.4, 2017) ISSN: 1520-5509 Clarion University of Pennsylvania, Clarion, Pennsylvania INTERROGATING GODFATHERS – ELECTORAL CORRUPTION NEXUS AS A CHALLENGE TO SUSTAINABLE DEVELOPMENT AND NATIONAL SECURITY IN FOURTH REPUBLIC NIGERIA 1Preye kuro Inokoba and 2Chibuzor Chile Nwobueze 1Department of Political Science, Niger Delta University, Bayelsa State, Nigeria 2Department Of History & Diplomatic Studies, Ignatius Ajuru University of Education, Port Harcourt ABSTRACT In all modern democracies, election is not only an instrument for selecting political officeholders but also a vital platform for ensuring government legitimacy, accountability and mobilization of the citizenry for political participation. However, elections in Nigeria since independence have been bedeviled by electoral corruption characterized by such vices as election rigging, snatching of electoral materials, result falsification, political intimidation and assassination before, during and after elections. This situation has often brought unpopular governments to power, with resultant legitimacy crisis, breakdown of law and order and general threat to security. The paper, in explaining the adverse effects of electoral fraud and violence on sustainable development and national security, identified political godfathers as the main orchestrators, masterminds and beneficiaries of electoral corruption in Nigeria. Through the application of the descriptive method of data analysis, the study investigates how godfathers, in a bid to achieve their inordinate political and pecuniary interests, flout all known electoral laws, subvert democratic institutions and governance and as a result threaten national development and security. The paper therefore concludes that, to effectively address the undemocratic practice of electoral corruption, which is a threat to sustainable development and national security, there is need for the strengthening of the legal framework and democratic structures in Nigeria. -

Legislative Control of the Executive in Nigeria Under the Second Republic
04, 03 01 AWO 593~ By AWOTOKUN, ADEKUNLE MESHACK B.A. (HONS) (ABU) M.Sc. (!BADAN) Thesis submitted to the Department of Public Administration Faculty of Administration in Partial fulfilment of the requirements for the degree of --~~·---------.---·-.......... , Progrnmme c:~ Petites Subventions ARRIVEE - · Enregistré sous lo no l ~ 1 ()ate :. Il fi&~t. JWi~ DOCTOR OF PHILOSOPHY (PUBLIC ADMIJISTRATION) Obafemi Awolowo University, CE\/ 1993 1le-Ife, Nigeria. 2 3 r • CODESRIA-LIBRARY 1991. CERTIFICATION 1 hereby certify that this thesis was prepared by AWOTOKUN, ADEKUNLE MESHACK under my supervision. __ _I }J /J1,, --- Date CODESRIA-LIBRARY ACKNOWLEDGEMENTS A work such as this could not have been completed without the support of numerous individuals and institutions. 1 therefore wish to place on record my indebtedness to them. First, 1 owe Professer Ladipo Adamolekun a debt of gratitude, as the persan who encouraged me to work on Legislative contrai of the Executive. He agreed to supervise the preparation of the thesis and he did until he retired from the University. Professor Adamolekun's wealth of academic experience ·has no doubt sharpened my outlciok and served as a source of inspiration to me. 1 am also very grateful to Professor Dele Olowu (the Acting Head of Department) under whose intellectual guidance I developed part of the proposai which culminated ·in the final production qf .this work. My pupilage under him i though short was memorable and inspiring. He has also gone through the entire draft and his comments and criticisms, no doubt have improved the quality of the thesis. Perhaps more than anyone else, the Almighty God has used my indefatigable superviser Dr. -
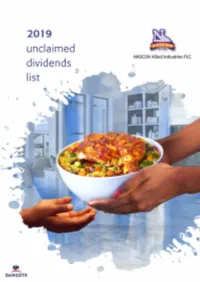
2019-Annual-Report-UNCLAIMED.Pdf
UNCLAIMED DIVIDENDS SN No. NAME SN No. NAME SN No. NAME 1 (HRH OBA) GABRIEL OLATERU ADEWOYE 96 ABDUL HAMID AZEEZAT OLUWANMI 191 ABDULLAHI MUHIBBA 2 (NZE) SUNDAY PAUL EZIEFULA 97 ABDUL JELILI ATANDA HADJI THOMPSON 192 ABDULLAHI OLANREWAJU ISIAQ 3 A A J ENIOLA 98 ABDUL LASISI MUSA 193 ABDULLAHI RAFIU ADESHINA 4 A A OYEGBADE 99 ABDUL MONSUR ROTIMI TOYIN 194 ABDULLAHI SABA 5 A A SIJUADE 100 ABDUL OLABOSIPO OGUNBANWO 195 ABDULLAHI SADILU MUYE 6 A BASHIR IRON BABA 101 ABDUL OTHMAN 196 ABDULLAHI SALAU (MALLAM) 7 A. ADESIHMA FAJEMILEHIN 102 ABDUL RAFIU AINA (ALHAJI) 197 ABDULLAHI SALE MUHAMMAD 8 A. AKINOLA 103 ABDUL RAFIU JIMOH 198 ABDULLAHI SALOME EGBUNU 9 A. OLADELE JACOB 104 ABDUL RAHAMAN ADEYEMI BELLO 199 ABDULLAHI SULE 10 A. OYEFUNSO OYEWUNMI 105 ABDUL RAHANMON MUYIDEEN 200 ABDULLAHI SUNDAY MUSA 11 A. RAHMAN BUSARI 106 ABDUL RAHEEM ISHOLA 201 ABDULLAHI TAMBARI KABIRU A.T. 12 A.A. UGOJI 107 ABDUL RAHEEM MORONFOLU 202 ABDULLAHI TANIMU 13 AA RANONIGERIA LIMITED 108 ABDUL RAHEIM OLADEJO 203 ABDULLAHI USMAN 14 AAA STOCKBROKERS LTD 109 ABDUL RASAQ RAJI 204 ABDULLAHI YARKOFOJI BADAMASI 15 AARON CHIGOZIE IDIKA 110 ABDUL RAZAQ OLUKAYODE ADETORO 205 ABDULLATEEF IYANDA ADUA 16 AARON IBEGBUNA AKABIKE 111 ABDUL RAZAQ OLUSOLA SAKA 206 ABDULLATEEF OLADEJO OPELOYERU 17 AARON M AMAK DAMAK 112 ABDUL TOLIB AIYEGBENI BELLO 207 ABDUL-MAJEED ABDUR-RAHEEM 18 AARON OBIAKOR 113 ABDUL WAHAB HAZZAN 208 ABDULMAJID ISAH 19 AARON OLUFEMI 114 ABDUL WAHEED AJIBADE 209 ABDUL-MALIK GARBA ADEBAYO 20 AARON U. AGU 115 ABDUL YEKINI KHADIJAT LARA 210 ABDULMALIK MAKAMA 21 AASA KOLA 116 ABDUL YEKINNI APENA (CHIEF) 211 ABDULMALIK USMAN 22 ABA FABS ONUCHE 117 ABDUL YEKINNI SHOBAYO 212 ABDULMALIKI OHUNENE AMINATU 23 ABABI Y OMOTOSHO 118 ABDULAHI ABDUSALAMI OLOMADA 213 ABDULMUMINI MOHAMMED 24 ABADA GOODLUCK AKACHUKWU A. -
Page 1 of 156
Page 1 of 156 Page 2 of 156 Page 3 of 156 Page 4 of 156 Page 5 of 156 Page 6 of 156 Page 7 of 156 TABLE OF CONTENTS NBA PRAYER 2 PRESIDENT 3 GENERAL SECRETARY 4 EXECUTIVES 5 NEC NOTICE 7 MINUTES OF DECEMBER NEC MEETING 8 5TH DECEMBER, 2019 PRESIDENT SPEEECH FINANCIAL REPORT 39 2019 (10%) BAR PRACTICE FEE REMITTANCE 64 TO NBA BRANCHES NBA 2019 AGC; PRESIDENT’S EXPLANATORY NOTE 69 NBA AGC 2019 FINANCIAL REPORT 71 NBA COMMITTEE REPORTS I. WOMEN’S FORUM 83 II. TECHNICAL COMMITTEE ON 100 CONFERENCE PLANNING III. SECTION ON PUBLIC INTEREST AND 139 DEVELOPMENT LAW REPORT IV. SECTION ON BUSSINESS LAW REPORT 141 V. SECTIONON ON LEGAL PRACTICE REPORT 147 VI. YOUNG LAWYERS’ FORUM 149 VII. LETTER OF COMMENDATION TO NBA BAR SERVICES DEPARTMENT Page 8 of 156 MINUTES OF THE NATIONAL EXECUTIVE COMMITTEE (NEC) MEETING OF THENIGERIAN BAR ASSOCIATION, HELD ON 5THDECEMBER, 2019 AT THE AUDITORIUM, NBA HOUSE NATIONAL SECRETARIAT ABUJA. 1.0. MEMBERS PRESENT: NATIONAL OFFICERS 1. PAUL USORO, SAN PRESIDENT 2. JONATHAN GUNU TAIDI, ESQ GENERAL SECRETARY 3. STANLEY CHIDOZIE IMO, ESQ 1ST VICE PRESIDENT 4. THEOPHILUS TERHILE IGBA , ESQ 3RD VICE PRESIDENT 5. BANKE OLAGBEGI-OLOBA, ESQ TREASURER 6. NNAMDI INNOCENT EZE, ESQ LEGAL ADVISER 7. JOSHUA ENEMALI USMAN, ESQ WELFARE SECRETARY 8. ELIAS EMEKA ANOSIKE, ESQ FINANCIAL SECRETARY 9. OLUKUNLE EDUN, ESQ PUBLICITY SECRETARY 10. EWENODE WILLIAM ONORIODE, ESQ 1ST ASST. SECRETARY 11. CHINYERE OBASI, ESQ 2ND ASST. SECRETARY 12. IRENE INIOBONG PEPPLE, ESQ ASST. FIN. SECRETARY 13. AKOREDE HABEEB LAWAL, ESQ ASST. PUB.