Recent Advances in Targeting the Prostacyclin Pathway in Pulmonary Arterial Hypertension
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
VTE) Cindy Ward, DNP, RN-BC, CMSRN, ACNS-BC
Chronic Complications of Venous Thromboembolism (VTE) Cindy Ward, DNP, RN-BC, CMSRN, ACNS-BC Roanoke, VA Disclosure • The speaker has no conflicts of interest to disclose. Carilion Roanoke Memorial Hospital • 3 time Magnet® designated • Flagship of Carilion Clinic, a 7 hospital system • Region’s only Level 1 Trauma Center • 703-bed academic medical center • System-wide, serves nearly 1 million patients across Virginia, West Virginia and North Carolina Objectives At the conclusion of this education activity, the learner will be able to: • recall VTE risk factors and prevention • describe post-thrombotic syndrome and chronic thromboembolic pulmonary hypertension (CTEPH) • identify nursing implications of caring for patients with post-thrombotic syndrome and CTEPH What is VTE? Pulmonary Embolus Deep Vein (PE) Thrombosis (DVT) Signs/Symptoms of DVT • Swelling • Erythema • Pain • Warmth1 Signs/Symptoms of PE 1 • Sudden onset of dyspnea • Tachycardia • Irregular heartbeat • Chest pain, worse with deep breath • Hemoptysis • Low blood pressure, light-headedness or syncope • 350,000 – 900,000 people per year are affected by VTE1, 2 • VTE is the leading cause of preventable hospital death in the US2 • VTE can occur without symptoms (silent)3 Quick Facts • Patients with DVT who are untreated have a 37% incidence of PE that is fatal4 • Combined mortality from PE (initial and recurrence) is 73%4 Quick Facts • 1 in 20 hospitalized patients will suffer a fatal PE if they have not received adequate VTE prophylaxis5 • For 25% of patients with PE, the first -

Cox Inhibitors and Thromboregulation
CLINICAL IMPLICATIONS OF BASIC RESEARCH Clinical Implications shown the importance of eicosanoids in preserving of Basic Research the dynamic balance among thrombosis, hemostasis, and the fluidity of blood. Recently, Cheng et al.1 presented compelling evi- dence that cell–cell interactions, principally between platelets and endothelial cells, that are mediated by ei- COX INHIBITORS cosanoids have a role in thrombosis. Using genetical- AND THROMBOREGULATION ly engineered mice that either overexpressed or lacked essential components of the eicosanoid pathway — ROM a historical perspective, there is perhaps no namely, receptors for prostacyclin (a platelet inhibitor Fmore interesting therapeutic saga than that of as- and vasodilator) or thromboxane A2 (a platelet agonist pirin, which began as a folk remedy, distilled from wil- and vasoconstrictor) — they found that the response low bark, and became a lifesaving preventive treatment of the intima of carotid vessels to mechanical injury is for ischemic cardiovascular disease. Aspirin primarily exuberant and leads to obstruction in mice lacking the inhibits the cyclooxygenase (COX)-dependent synthe- prostacyclin receptor. However, this response is muted sis of eicosanoids, which are the end products of me- in mice lacking the thromboxane A2 receptor or both tabolism of essential fatty acids and include prosta- receptors. In mice lacking the prostacyclin receptor cyclin and thromboxane A2. Numerous studies have (a defect that mimics the effects of COX-2–selective Endothelial cell Resting platelet Thromboxane A2 Soluble Stimulation CD39 Arachidonic acid Stimulated platelet COX inhibitor ATP and ADP Prostacyclin Nitric oxide AMP Carbon monoxide CD39 Resting platelet Figure 1. Effect on Platelet Reactivity of the Eicosanoids Thromboxane A2 and Prostacyclin, the Biologic Gases Nitric Oxide and Carbon Monoxide, and the Ectonucleotidase CD39. -

Endogenous Biosynthesis of Prostacyclin and Thromboxane and Platelet Function During Chronic Administration of Aspirin in Man
Endogenous biosynthesis of prostacyclin and thromboxane and platelet function during chronic administration of aspirin in man. G A FitzGerald, … , J A Lawson, A R Brash J Clin Invest. 1983;71(3):676-688. https://doi.org/10.1172/JCI110814. Research Article To assess the pharmacologic effects of aspirin on endogenous prostacyclin and thromboxane biosynthesis, 2,3-dinor-6- keto PGF1 alpha (PGI-M) and 2,3-dinor-thromboxane B2 (Tx-M) were measured in urine by mass spectrometry during continuing administration of aspirin. To define the relationship of aspirin intake to endogenous prostacyclin biosynthesis, sequential urines were initially collected in individuals prior to, during, and subsequent to administration of aspirin. Despite inter- and intra-individual variations, PGI-M excretion was significantly reduced by aspirin. However, full mass spectral identification confirmed continuing prostacyclin biosynthesis during aspirin therapy. Recovery of prostacyclin biosynthesis was incomplete 5 d after drug administration was discontinued. To relate aspirin intake to indices of thromboxane biosynthesis and platelet function, volunteers received 20 mg aspirin daily followed by 2,600 mg aspirin daily, each dose for 7 d in sequential weeks. Increasing aspirin dosage inhibited Tx-M excretion from 70 to 98% of pretreatment control values; platelet TxB2 formation from 4.9 to 0.5% and further inhibited platelet function. An extended study was performed to relate aspirin intake to both thromboxane and prostacyclin generation over a wide range of doses. Aspirin, in the range of 20 to 325 mg/d, resulted in a dose-dependent decline in both Tx-M and PGI-M excretion. At doses of 325-2,600 mg/d Tx-M excretion ranged from 5 to 3% of control values while PGI-M remained at 37-23% of control. -

Challenging the FDA Black Box Warning for High Aspirin Dose with Ticagrelor in Patients with Diabetes James J
PERSPECTIVES IN DIABETES Challenging the FDA Black Box Warning for High Aspirin Dose With Ticagrelor in Patients With Diabetes James J. DiNicolantonio and Victor L. Serebruany – Ticagrelor, a novel reversible antiplatelet agent, has a Food and ASA 300 325 mg (53.6%) in the U.S. compared with the Drug Administration (FDA) black box warning to avoid mainte- rest of the world (1.7%) was the only factor to explain nance doses of aspirin (ASA) .100 mg/daily. This restriction is (out of 37 variables explored) the regional interaction based on the hypothesis that ASA doses .100 mg somehow de- that ticagrelor was less effective and potentially more creased ticagrelor’s benefit in the Platelet Inhibition and Patient harmful than clopidogrel (2). However, this interaction Outcomes (PLATO) U.S. cohort. However, these data are highly was not significant, is highly postrandomized, comes postrandomized, come from a very small subgroup in PLATO from a very small subgroup of PLATO, and makes no (57% of patients in the U.S. site), and make no biological sense. biological sense (3). Moreover, the ticagrelor-ASA interaction was not significant by any multivariate Cox regression analyses. The Complete Re- sponse Review for ticagrelor indicates that for U.S. PLATO patients, an ASA dose .300 mg was not a significant interaction TICAGRELOR-ASA HYPOTHESIS for vascular outcomes. In the ticagrelor-ASA .300 mg cohort, all- The claimed ticagrelor-ASA interaction states that ticagrelor cause and vascular mortality were not significantly increased fi – P plus low-dose ASA is bene cial, whereas increasing doses (hazard ratio [HR] 1.27 [95% CI 0.84 1.93], = 0.262 and 1.39 of ASA in combination with ticagrelor produces adverse [0.87–2.2], P = 0.170), respectively. -

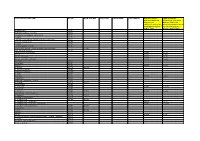
CDK4/6 Inhibitors in Breast Cancer Treatment: Potential Interactions with Drug, Gene and Pathophysiological Conditions
Review CDK4/6 Inhibitors in Breast Cancer Treatment: Potential Interactions with Drug, Gene and Pathophysiological Conditions Rossana Roncato 1,*,†, Jacopo Angelini 2,†, Arianna Pani 2,3,†, Erika Cecchin 1, Andrea Sartore-Bianchi 2,4, Salvatore Siena 2,4, Elena De Mattia 1, Francesco Scaglione 2,3,‡ and Giuseppe Toffoli 1,‡ 1 1 Experimental and Clinical Pharmacology Unit, Centro di Riferimento Oncologico (CRO), IRCCS, 33081 Aviano, Italy; [email protected] (E.C.); [email protected] (E.D.M.); [email protected] (G.T.) 2 Department of Oncology and Hemato-Oncology, Università degli Studi di Milano, 20122 Milan, Italy; [email protected] (J.A.); [email protected] (A.P.); [email protected] (A.S-B.); [email protected] (S.S.); [email protected] (F.S.) 3 Clinical Pharmacology Unit, ASST Grande Ospedale Metropolitano Niguarda, Piazza dell'Ospedale Maggiore 3, 20162 Milan, Italy 4 Department of Hematology and Oncology, Niguarda Cancer Center, Grande Ospedale Metropolitano Niguarda, 20162 Milan, Italy * Correspondence: [email protected]; Tel.:+390434659130 † These authors contributed equally. ‡ These authors share senior authorship. Int. J. Mol. Sci. 2020, 21, x; doi: www.mdpi.com/journal/ijms Int. J. Mol. Sci. 2020, 21, x 2 of 8 Table S1. Co-administered agents categorized according to their potential risk for Drug-Drug interaction (DDI) in combination with CDK4/6 inhibitors (CDKis). Colors suggest the risk of DDI with CDKis: green, low risk DDI; orange, moderate risk DDI; red, high risk DDI. ADME, absorption, distribution, metabolism, and excretion; GI, Gastrointestinal; TdP, Torsades de Pointes; NTI, narrow therapeutic index. * Cardiological toxicity should be considered especially for ribociclib due to the QT prolongation. -

GTH 2021 State of the Art—Cardiac Surgery: the Perioperative Management of Heparin-Induced Thrombocytopenia in Cardiac Surgery
Review Article 59 GTH 2021 State of the Art—Cardiac Surgery: The Perioperative Management of Heparin-Induced Thrombocytopenia in Cardiac Surgery Laura Ranta1 Emmanuelle Scala1 1 Department of Anesthesiology, Cardiothoracic and Vascular Address for correspondence Emmanuelle Scala, MD, Centre Anesthesia, Lausanne University Hospital (CHUV), Lausanne, Hospitalier Universitaire Vaudois, Rue du Bugnon 46, BH 05/300, 1011 Switzerland Lausanne, Suisse, Switzerland (e-mail: [email protected]). Hämostaseologie 2021;41:59–62. Abstract Heparin-induced thrombocytopenia (HIT) is a severe, immune-mediated, adverse drug Keywords reaction that paradoxically induces a prothrombotic state. Particularly in the setting of ► Heparin-induced cardiac surgery, where full anticoagulation is required during cardiopulmonary bypass, thrombocytopenia the management of HIT can be highly challenging, and requires a multidisciplinary ► cardiac surgery approach. In this short review, the different perioperative strategies to run cardiopul- ► state of the art monary bypass will be summarized. Introduction genicity of the antibodies and is diagnostic for HIT. The administration of heparin to a patient with circulating Heparin-induced thrombocytopenia (HIT) is a severe, im- pathogenic HITabs puts the patient at immediate risk of mune-mediated, adverse drug reaction that paradoxically severe thrombotic complications. induces a prothrombotic state.1,2 Particularly in the setting The time course of HIT can be divided into four distinct of cardiac surgery, where full anticoagulation is required phases.6 Acute HIT is characterized by thrombocytopenia during cardiopulmonary bypass (CPB), the management of and/or thrombosis, the presence of HITabs, and confirma- HIT can be highly challenging, and requires a multidisciplin- tion of their platelet activating capacity by a functional ary approach. -
List of Union Reference Dates A
Active substance name (INN) EU DLP BfArM / BAH DLP yearly PSUR 6-month-PSUR yearly PSUR bis DLP (List of Union PSUR Submission Reference Dates and Frequency (List of Union Frequency of Reference Dates and submission of Periodic Frequency of submission of Safety Update Reports, Periodic Safety Update 30 Nov. 2012) Reports, 30 Nov. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Inverse Agonism of SQ 29,548 and Ramatroban on Thromboxane A2 Receptor
Inverse Agonism of SQ 29,548 and Ramatroban on Thromboxane A2 Receptor Raja Chakraborty1,3, Rajinder P. Bhullar1, Shyamala Dakshinamurti2,3, John Hwa4, Prashen Chelikani1,2,3* 1 Department of Oral Biology, University of Manitoba, Winnipeg, Manitoba, Canada, 2 Departments of Pediatrics, Physiology, University of Manitoba, Winnipeg, Manitoba, Canada, 3 Biology of Breathing Group- Manitoba Institute of Child Health, Winnipeg, Manitoba, Canada, 4 Department of Internal Medicine (Cardiology), Cardiovascular Research Center, Yale University School of Medicine, New Haven, Connecticut, United States of America Abstract G protein-coupled receptors (GPCRs) show some level of basal activity even in the absence of an agonist, a phenomenon referred to as constitutive activity. Such constitutive activity in GPCRs is known to have important pathophysiological roles in human disease. The thromboxane A2 receptor (TP) is a GPCR that promotes thrombosis in response to binding of the prostanoid, thromboxane A2. TP dysfunction is widely implicated in pathophysiological conditions such as bleeding disorders, hypertension and cardiovascular disease. Recently, we reported the characterization of a few constitutively active mutants (CAMs) in TP, including a genetic variant A160T. Using these CAMs as reporters, we now test the inverse agonist properties of known antagonists of TP, SQ 29,548, Ramatroban, L-670596 and Diclofenac, in HEK293T cells. Interestingly, SQ 29,548 reduced the basal activity of both, WT-TP and the CAMs while Ramatroban was able to reduce the basal activity of only the CAMs. Diclofenac and L-670596 showed no statistically significant reduction in basal activity of WT-TP or CAMs. To investigate the role of these compounds on human platelet function, we tested their effects on human megakaryocyte based system for platelet activation. -

Effects of Selexipag and Its Active Metabolite in Contrasting The
Cutolo et al. Arthritis Research & Therapy (2018) 20:77 https://doi.org/10.1186/s13075-018-1577-0 RESEARCH ARTICLE Open Access Effects of selexipag and its active metabolite in contrasting the profibrotic myofibroblast activity in cultured scleroderma skin fibroblasts Maurizio Cutolo1*, Barbara Ruaro1, Paola Montagna1, Renata Brizzolara1, Emanuela Stratta2, Amelia Chiara Trombetta1, Stefano Scabini2, Pier Paolo Tavilla3, Aurora Parodi3, Claudio Corallo4, Nicola Giordano4, Sabrina Paolino1, Carmen Pizzorni1, Alberto Sulli1, Vanessa Smith5 and Stefano Soldano1 Abstract Background: Myofibroblasts contribute to fibrosis through the overproduction of extracellular matrix (ECM) proteins, primarily type I collagen (COL-1) and fibronectin (FN), a process which is mediated in systemic sclerosis (SSc) by the activation of fibrogenic intracellular signaling transduction molecules, including extracellular signal-regulated kinases 1 and 2 (Erk1/2) and protein kinase B (Akt). Selexipag is a prostacyclin receptor agonist synthesized for the treatment of pulmonary arterial hypertension. The study investigated the possibility for selexipag and its active metabolite (ACT-333679) to downregulate the profibrotic activity in primary cultures of SSc fibroblasts/myofibroblasts and the fibrogenic signaling molecules involved. Methods: Fibroblasts from skin biopsies obtained with Ethics Committee (EC) approval from patients with SSc, after giving signed informed consent, were cultured until the 3rd culture passage and then either maintained in normal growth medium (untreated cells) or independently treated with different concentrations of selexipag (from 30 μMto 0.3 μM) or ACT-333679 (from 10 μMto0.1μM) for 48 h. Protein and gene expressions of α-smooth muscle actin (α-SMA), fibroblast specific protein-1 (S100A4), COL-1, and FN were investigated by western blotting and quantitative real-time PCR. -

Clinical Trial Protocol: BPS-314D-MR-PAH-302
Clinical Trial Protocol: BPS-314d-MR-PAH-302 Study Title: A multicenter, double-blind, randomized, placebo-controlled, Phase 3 study to assess the efficacy and safety of oral BPS-314d-MR added-on to treprostinil, inhaled (Tyvaso®) in subjects with pulmonary arterial hypertension Study Number: BPS-314d- MR-PAH-302 Study Phase: 3 Product Name: Beraprost Sodium 314d Modified Release IND Number: 111,729 Indication: Treatment of Pulmonary Arterial Hypertension Investigators: Multicenter Sponsor: Lung Biotechnology Inc. Sponsor Contact: Medical Monitor: Date Original Protocol: 16 April 2013 Amendment 1: 17 December 2013 Amendment 2 15 October 2014 GCP Statement: This study will be conducted in compliance with the protocol, Good Clinical Practice (GCP) and applicable regulatory requirements. Confidentiality Statement The concepts and information contained herein are confidential and proprietary and shall not be disclosed in whole or part without the express written consent of Lung Biotechnology Inc. © 2014 Lung Biotechnology Inc. Beraprost Sodium 314d Modified Release Lung Biotechnology Inc. Clinical Trial Protocol: BPS-314-d-MR-PAH 302 15 October 2014 LIST OF CONTACTS Study Sponsor: Lung Biotechnology Inc. 1040 Spring Street Silver Spring, Maryland 20910 United States Phone: 301-608-9292 Fax: 301-589-0855 Sponsor Contact: Medical Monitor: SAE Reporting: CONFIDENTIAL Page 2 of 75 Beraprost Sodium 314d Modified Release Lung Biotechnology Inc. Clinical Trial Protocol: BPS-314-d-MR-PAH 302 15 October 2014 SYNOPSIS Sponsor: Lung Biotechnology Inc. -

Effect of Prostanoids on Human Platelet Function: an Overview
International Journal of Molecular Sciences Review Effect of Prostanoids on Human Platelet Function: An Overview Steffen Braune, Jan-Heiner Küpper and Friedrich Jung * Institute of Biotechnology, Molecular Cell Biology, Brandenburg University of Technology, 01968 Senftenberg, Germany; steff[email protected] (S.B.); [email protected] (J.-H.K.) * Correspondence: [email protected] Received: 23 October 2020; Accepted: 23 November 2020; Published: 27 November 2020 Abstract: Prostanoids are bioactive lipid mediators and take part in many physiological and pathophysiological processes in practically every organ, tissue and cell, including the vascular, renal, gastrointestinal and reproductive systems. In this review, we focus on their influence on platelets, which are key elements in thrombosis and hemostasis. The function of platelets is influenced by mediators in the blood and the vascular wall. Activated platelets aggregate and release bioactive substances, thereby activating further neighbored platelets, which finally can lead to the formation of thrombi. Prostanoids regulate the function of blood platelets by both activating or inhibiting and so are involved in hemostasis. Each prostanoid has a unique activity profile and, thus, a specific profile of action. This article reviews the effects of the following prostanoids: prostaglandin-D2 (PGD2), prostaglandin-E1, -E2 and E3 (PGE1, PGE2, PGE3), prostaglandin F2α (PGF2α), prostacyclin (PGI2) and thromboxane-A2 (TXA2) on platelet activation and aggregation via their respective receptors. Keywords: prostacyclin; thromboxane; prostaglandin; platelets 1. Introduction Hemostasis is a complex process that requires the interplay of multiple physiological pathways. Cellular and molecular mechanisms interact to stop bleedings of injured blood vessels or to seal denuded sub-endothelium with localized clot formation (Figure1).