REVISÃO / REVIEW but It Is Interesting to Review Some Aspects of the GERD Refractory Patients to the Proton Pump Inhibitors Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

List of New Drugs Approved in India from 1991 to 2000
LIST OF NEW DRUGS APPROVED IN INDIA FROM 1991 TO 2000 S. No Name of Drug Pharmacological action/ Date of Indication Approval 1 Ciprofloxacin 0.3% w/v Eye Indicated in the treatment of February-1991 Drops/Eye Ointment/Ear Drop external ocular infection of the eye. 2 Diclofenac Sodium 1gm Gel March-1991 3 i)Cefaclor Monohydrate Antibiotic- In respiratory April-1991 250mg/500mg Capsule. infections, ENT infection, UT ii)Cefaclor Monohydrate infections, Skin and skin 125mg/5ml & 250mg/5ml structure infections. Suspension. iii)Cefaclor Monohydrate 100mg/ml Drops. iv)Cefaclor 187mg/5ml Suspension (For paediatric use). 4 Sheep Pox Vaccine (For April-1991 Veterinary) 5 Omeprazole 10mg/20mg Short term treatment of April-1991 Enteric Coated Granules duodenal ulcer, gastric ulcer, Capsule reflux oesophagitis, management of Zollinger- Ellison syndrome. 6 i)Nefopam Hydrochloride Non narcotic analgesic- Acute April-1991 30mg Tablet. and chronic pain, including ii)Nefopam Hydrochloride post-operative pain, dental 20mg/ml Injection. pain, musculo-skeletal pain, acute traumatic pain and cancer pain. 7 Buparvaquone 5% w/v Indicated in the treatment of April-1991 Solution for Injection (For bovine theileriosis. Veterinary) 8 i)Kitotifen Fumerate 1mg Anti asthmatic drug- Indicated May-1991 Tablet in prophylactic treatment of ii)Kitotifen Fumerate Syrup bronchial asthma, symptomatic iii)Ketotifen Fumerate Nasal improvement of allergic Drops conditions including rhinitis and conjunctivitis. 9 i)Pefloxacin Mesylate Antibacterial- In the treatment May-1991 Dihydrate 400mg Film Coated of severe infection in adults Tablet caused by sensitive ii)Pefloxacin Mesylate microorganism (gram -ve Dihydrate 400mg/5ml Injection pathogens and staphylococci). iii)Pefloxacin Mesylate Dihydrate 400mg I.V Bottles of 100ml/200ml 10 Ofloxacin 100mg/50ml & Indicated in RTI, UTI, May-1991 200mg/100ml vial Infusion gynaecological infection, skin/soft lesion infection. -

The Role for Pre-Polymerized Sucralfate In
ISSN: 2692-5400 DOI: 10.33552/AJGH.2020.02.000531 Academic Journal of Gastroenterology & Hepatology Review Article Copyright © All rights are reserved by Ricky Wayne McCullough The Role for Pre-Polymerized Sucralfate in Management of Erosive and Non-Erosive Gastroesophageal Reflux Disease – High Potency Sucralfate-Mucin Barrier for Enteric Cytoprotection Ricky Wayne McCullough1,2* 1Translational Medicine Clinic and Research Center, USA 2Department of Internal Medicine and Emergency Medicine, Warren Alpert Brown University School of Medicine, USA *Corresponding author: Ricky Wayne McCullough, Translational Medicine Clinic and Received Date: April 13, 2020 Research Center, Storrs Connecticut, USA. Published Date: April 22, 2020 Abstract Pre-polymerized sucralfate, sometimes called high potency sucralfate or polymerized cross-linked sucralfate is a new sucralfate formulation recognizedClinical by outcomes the US FDAfrom in standard 2005. Positive sucralfate clinical do not data justify from a threerole in randomized the management controlled of erosive trials and using non-erosive pre-polymerized gastroesophageal sucralfate refluxfor GERD disease. and each of which cause classic mucosal reactions in the esophageal epithelium. These reactions are symptomatic but may or may not involve erosions. NERD was first reported in 2014 AGA’s Digestive Disease Week (DDW). Gastric refluxate contains protonic acid, dissolved bile acids and proteases Pre-polymerizedBeing non-systemic, sucralfate the utilizes entire biophysical clinical effect means of toany exclude sucralfate all three rests irritants in the fromsurface epithelial concentration mucosa. of sucralfate achieved. Pre-polymerized sucralfate, presented in 2014 DDW, and discussed here, achieves a surface concentration that is 800% greater than standard sucralfate on normal mucosal lining and 2,400% greater on inflamed or acid-injured mucosa, making it most certainly, a high potency sucralfate. -

Lansoprazole Delayed-Release Orally Disintegrating Tablets PI
HIGHLIGHTS OF PRESCRIBING INFORMATION • Patients receiving rilpivirine-containing products. (4, 7) Dual Therapy: Lansoprazole delayed-release orally disintegrating tablets/amoxicillin Administration with Water in an Oral Syringe 6.1 Clinical Trials Experience In clinical trials using combination therapy with lansoprazole plus amoxicillin and clarithromycin, women. Because animal reproduction studies are not always predictive of human response, this 8.6 Hepatic Impairment These highlights do not include all the information WARNINGS AND PRECAUTIONS Lansoprazole delayed-release orally disintegrating tablets in combination with amoxicillin as dual 1. Place a 15 mg tablet in oral syringe and draw up 4 mL of water, or place a 30 mg tablet Because clinical trials are conducted under widely varying conditions, adverse reaction rates and lansoprazole plus amoxicillin, no increased laboratory abnormalities particular to these drug drug should be used during pregnancy only if clearly needed [see Nonclinical Toxicology (13.2)]. In patients with various degrees of chronic hepatic impairment the exposure to lansoprazole was needed to use LANSOPRAZOLE DELAYED- • Gastric Malignancy: In adults, symptomatic therapy is indicated in adults for the treatment of patients with H. pylori infection and duodenal in oral syringe and draw up 10 mL of water. observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of combinations were observed. See full prescribing information for clarithromycin before using in pregnant women. increased compared to healthy subjects with normal hepatic function [see Clinical Pharmacology RELEASE ORALLY DISINTEGRATING TABLETS response with lansoprazole does not preclude ulcer disease (active or one year history of a duodenal ulcer) who are either allergic or intolerant 2. -
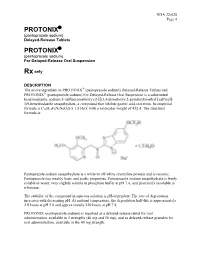
Protonix Protonix
NDA 22-020 Page 4 PROTONIX® (pantoprazole sodium) Delayed-Release Tablets PROTONIX® (pantoprazole sodium) For Delayed-Release Oral Suspension Rx only DESCRIPTION ® The active ingredient in PROTONIX (pantoprazole sodium) Delayed-Release Tablets and ® PROTONIX (pantoprazole sodium) For Delayed-Release Oral Suspension is a substituted benzimidazole, sodium 5-(difluoromethoxy)-2-[[(3,4-dimethoxy-2-pyridinyl)methyl] sulfinyl]- 1H-benzimidazole sesquihydrate, a compound that inhibits gastric acid secretion. Its empirical formula is C16H14F2N3NaO4S x 1.5 H2O, with a molecular weight of 432.4. The structural formula is: Pantoprazole sodium sesquihydrate is a white to off-white crystalline powder and is racemic. Pantoprazole has weakly basic and acidic properties. Pantoprazole sodium sesquihydrate is freely soluble in water, very slightly soluble in phosphate buffer at pH 7.4, and practically insoluble in n-hexane. The stability of the compound in aqueous solution is pH-dependent. The rate of degradation increases with decreasing pH. At ambient temperature, the degradation half-life is approximately 2.8 hours at pH 5.0 and approximately 220 hours at pH 7.8. PROTONIX (pantoprazole sodium) is supplied as a delayed-release tablet for oral administration, available in 2 strengths (40 mg and 20 mg); and as delayed-release granules for oral administration, available in the 40 mg strength. NDA 22-020 Page 5 Each PROTONIX (pantoprazole sodium) Delayed-Release tablet contains 45.1 mg or 22.6 mg of pantoprazole sodium sesquihydrate (equivalent to 40 mg or 20 mg pantoprazole, respectively) with the following inactive ingredients: calcium stearate, crospovidone, hypromellose, iron oxide, mannitol, methacrylic acid copolymer, polysorbate 80, povidone, propylene glycol, sodium carbonate, sodium lauryl sulfate, titanium dioxide, and triethyl citrate. -

Proton Pump Inhibitors
MEDICATION POLICY: Proton Pump Inhibitors Generic Name: Proton Pump Inhibitors Preferred: Esomeprazole (generic), Lansoprazole (generic), Omeprazole (generic), Therapeutic Class or Brand Name: Proton Pantoprazole (generic), and Rabeprazole Pump Inhibitors (generic) Applicable Drugs (if Therapeutic Class): Non-preferred: Aciphex® (rabeprazole), Esomeprazole (generic), Lansoprazole Dexilant® (dexlansoprazole), Nexium® (generic), Omeprazole (generic), Pantoprazole (esomeprazole), Not Medically Necessary: (generic), and Rabeprazole (generic). Omeprazole/Sodium Bicarbonate (generic), Aciphex® (rabeprazole), Dexilant® Zegerid® (omeprazole/sodium bicarbonate). (dexlansoprazole), Nexium® (esomeprazole), Prevacid® (lansoprazole), Prilosec® Date of Origin: 2/1/2013 (omeprazole), and Protonix® (pantoprazole). Date Last Reviewed / Revised: 12/23/2020 Omeprazole/Sodium Bicarbonate (generic), Zegerid® (omeprazole/sodium bicarbonate). Policy also applies to any other Proton Pump Inhibitors not listed. GPI Code: 4927002000, 4927002510, 4927004000, 4927006000, 4927007010, 4927007610, 4999600260 PRIOR AUTHORIZATION CRITERIA (May be considered medically necessary when criteria I and II are met) I. Documented diagnosis of one of the following A through G: A. Gastroesophageal reflux disease (GERD). B. Erosive esophagitis. C. Gastric ulcers. D. Risk reduction of NSAID-associated gastric ulcer. E. Duodenal ulcers. F. Eradication of H. pylori. G. Hypersecretory conditions II. Non-preferred PPIs require documented trials and failures of all generic PPIs. EXCLUSION -
2018 Annual Results Presentation
2018 Annual Results Presentation Sihuan Pharmaceutical Holdings Group Ltd. 四环医药控股集团有限公司 0 Disclaimer The sole purpose of this Presentation (the “Presentation”) is to assist the recipient in deciding whether it wishes to proceed with a further investigation of Sihuan Pharmaceutical Holdings Group Ltd. (the “Company”) and it is not intended to form the basis of any decision to purchase securities, interests or assets in or of the Company. This Presentation does not constitute or contain an offer or invitation or recommendation or solicitation for the sale or purchase of securities, interests or assets in or of the Company and neither this document nor anything contained herein shall form the basis of, or be relied upon in connection with, any contract or commitment whatsoever. Any decision to purchase or subscribe for securities in any offering must be made solely on the basis of the information contained in the prospectus or offering circular issued by the company in connection with such offerings. All the information in this Presentation has been provided by the Company and has not been independently verified. No representation or warranty, express or implied, is or will be made in or in relation to, and no responsibility or liability is or will be accepted by the Company or any of its subsidiaries as to the appropriateness, accuracy, completeness or reliability of, this Presentation or any other written or oral information made available to any interested party or its advisers and any liability therefore is hereby expressly disclaimed. And no reliance should be placed on the accuracy, fairness, completeness or correctness of the information contained in this Presentation. -

Carafate, Tablet
NEW ZEALAND DATA SHEET CARAFATE 1. Product Name Carafate, 1 g, tablet. 2. Qualitative and Quantitative Composition Each tablet contains 1 g sucralfate For the full list of excipients, see section 6.1. 3. Pharmaceutical Form Carafate is a white, uncoated capsule-shaped tablet. One side is plain, the other embossed with the word ‘CARAFATE’. Dimensions: 20 mm x 9 mm x 7mm 4. Clinical Particulars 4.1 Therapeutic indications Treatment of acute, non-malignant gastric ulcer and duodenal ulcer. Maintenance therapy to prevent the recurrence of duodenal ulcers. 4.2 Dose and method of administration Acute ulcerous conditions The recommended adult dose of Carafate for duodenal ulcer and gastric ulcer is 1 g tablet three times a day, one hour before meals and one 1 g tablet at bedtime or two 1 g tablets twice daily taken before breakfast and at bedtime (for up to 8 weeks). For relief of pain, antacids may be added to the treatment. However, they should not be taken within two hours before or after sucralfate intake. In duodenal ulcer, while healing with sucralfate often occurs within two to four weeks, treatment should be continued for up to 8 weeks unless healing has been demonstrated by x-ray and/or endoscopic examination. In the case of gastric ulcers an alternative treatment should be considered if no objective improvement is observed following 6 weeks of sucralfate therapy. Large gastric ulcers that show a progressive healing tendency may require the full 8 weeks of therapy. Maintenance treatment To reduce the risk of recurrence of duodenal ulcers, the recommended dose is one 1 g tablet before breakfast and one at bedtime (for up to 12 months). -

Patient Instructions for Colonoscopy and Upper GI Endoscopy
GASTROENTEROLOGY Patient Instructions for Colonoscopy and Upper GI Endoscopy This handout will help you get ready for your procedures. It has information about: Where to go for your procedures What are the procedures and why are they done Preparing ahead of time for your procedures Bowel preparation instructions Medication and diet instructions before your procedures What to expect during your procedures WHERE TO GO FOR YOUR COLONOSCOPY/UPPER ENDOSCOPY UVM Medical Center 111 Colchester Ave Endoscopy Outpatient Clinic West Pavilion, Level 4 Burlington, VT 05401 Check in at registration first: Level 3, Main Lobby WHAT IS A COLONOSCOPY? A colonoscopy is an examination of the colon (large intestine) using a specialized video camera called an endoscope. This instrument is inserted into the rectum and advanced up into your large intestine until it meets the small intestine. It shows images of the lining of the large intestine. Tissue samples (biopsies) may be taken during the test. This test can help diagnose and potentially treat: Early signs of cancer in the colon and rectum, specifically remove these abnormal growths called polyps Causes of unexplained changes in bowel habits Causes of inflamed tissue, abnormal growths, ulcers and bleeding WHAT IS AN UPPER ENDOSCOPY? Also known as: Esophagogastroduodenoscopy; EGD, Gastroscopy. An upper GI endoscopy is an examination of the upper gastrointestinal (GI) tract using a specialized video camera called an endoscope. This instrument is inserted down the throat and shows images of the lining -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG . -

PHRP March 2015
March 2015; Vol. 25(2):e2521518 doi: http://dx.doi.org/10.17061/phrp2521518 www.phrp.com.au Research Manual versus automated coding of free-text self-reported medication data in the 45 and Up Study: a validation study Danijela Gnjidica,b,i, Sallie-Anne Pearsona,c, Sarah N Hilmerb,d, Jim Basilakise, Andrea L Schaffera, Fiona M Blythb,f,g and Emily Banksg,h, on behalf of the High Risk Prescribing Investigators a Faculty of Pharmacy, University of Sydney, NSW, Australia b Sydney Medical School, University of Sydney, NSW, Australia c Sydney School of Public Health, University of Sydney, NSW, Australia d Royal North Shore Hospital and Kolling Institute of Medical Research, Sydney, NSW, Australia e School of Computing, Engineering and Mathematics, University of Western Sydney, NSW, Australia f Centre for Education and Research on Ageing (CERA), Concord Hospital, Sydney, NSW, Australia g The Sax Institute, Sydney, NSW, Australia h National Centre for Epidemiology and Population Health, Australian National University, Canberra, ACT i Corresponding author: [email protected] Article history Abstract Publication date: March 2015 Background: Increasingly, automated methods are being used to code free- Citation: Gnjidic D, Pearson S, Hilmer S, text medication data, but evidence on the validity of these methods is limited. Basilakis J, Schaffer AL, Blyth FM, Banks E. To examine the accuracy of automated coding of previously keyed Manual versus automated coding of free-text Aim: in free-text medication data compared with manual coding of original self-reported medication data in the 45 and Up Study: a validation study. Public Health handwritten free-text responses (the ‘gold standard’). -

Mini-Reviews and Perspectives
Mini-Reviews and Perspectives Persistent Reflux Symptoms in the Proton Pump Inhibitor Era: The Changing Face of Gastroesophageal Reflux Disease EVAN S. DELLON and NICHOLAS J. SHAHEEN Center for Esophageal Diseases and Swallowing and Center for Gastrointestinal Biology and Disease, Division of Gastroenterology and Hepatology, Department of Medicine, University of North Carolina School of Medicine, Chapel Hill, North Carolina iven the widespread use of potent acid suppressive Despite the common nature of incomplete control of Gtherapies and primary caregivers’ increasing com- GERD symptoms on PPI therapy, a universal definition fort with prescribing these medications at high doses, the for “PPI-refractory GERD” is lacking. Is a subject PPI patient population presenting to gastroenterologists for refractory after incomplete control at once daily dosing? symptoms of gastroesophageal reflux disease (GERD) has Should twice daily (BID) or other regimens be required changed. Whereas previous consultation often revolved before a subject is considered refractory? Previous work around the control of erosive disease and other mucosal demonstrates that a substantial number of subjects (as manifestations of GERD, and terminated with the prescrip- high as 32%) on daily PPI continue to demonstrate ab- tion of proton pump inhibitor (PPI) therapy, gastroenter- normal distal esophageal acid exposures, and that this ologists often now only enter the scene after failure of PPI proportion can be lowered to single digits by increasing therapy, for symptoms either resistant or only partially standard therapy to BID PPI.6,7 However, US Food and responsive to these medications. Because of the high pro- Drug Administration-approved dosing of these medica- portion of subjects with esophagitis who are healed with tions does not extend to BID therapy. -

Acid-Reducing Medications: Interactions with Harvoni and Epclusa
November 2016 | www.hepatitis.va.gov Acid-Reducing Medications: Interactions with Harvoni® and Epclusa® Sofosbuvir/Velpatasvir = Epclusa® Ledipasvir/Sofosbuvir = Harvoni® • Acid-reducing medications can decrease the effectiveness of Harvoni® and Epclusa® and could prevent successful cure. • Let your provider know if you are taking any acid-reducing medications—either prescribed to you or purchased over the counter. Types of Acid-Reducing What to Do if What to Do if Medications Taking Epclusa® Taking Harvoni® Antacids Separate taking the antacid and Separate taking the antacid and Epclusa® by 4 hours Harvoni® by 4 hours Combinations of aluminum, magnesium, and calcium. Brand names include: Alka-Seltzer® Maalox® Mylanta® Rolaids® TUMS® H2 Blockers Do not take more than the Do not take more than the recommended doses recommended doses Cimetidine (Tagamet®) Famotidine (Pepcid®) May take together with Epclusa® May take together with Harvoni® Nizatidine (Axid®) or 12 hours apart or 12 hours apart Ranitidine (Zantac®) Proton Pump Inhibitors (PPI) It is best to avoid PPIs during treat- It is best to avoid PPIs during ment with Epclusa®. If there are no treatment with Harvoni®. If there Esomeprazole (Nexium®) alternatives, follow these instructions: are no alternatives, follow these Lansoprazole (Prevacid®) instructions: Omeprazole (Prilosec®) Take Epclusa® with food Pantoprazole (Protonix®) Take the proton pump inhibitor 4 Take Harvoni® and the proton Rabeprazole (Aciphex®) hours after taking Epclusa® pump inhibitor at the same time in the morning after fasting overnight Do not take the proton pump (on an empty stomach) inhibitor at the same time as Epclusa® Do not take proton pump Do not take proton pump inhibitors inhibitors at more than the at more than the recommended dose recommended dose U.S.