View Subarachnoid Hemorrhage (SAH) Means There Is Bleeding Into the Fluid Space That Surrounds the Brain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Diagnosis of Subarachnoid Haemorrhage
Journal ofNeurology, Neurosurgery, and Psychiatry 1990;53:365-372 365 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.53.5.365 on 1 May 1990. Downloaded from OCCASIONAL REVIEW The diagnosis of subarachnoid haemorrhage M Vermeulen, J van Gijn Lumbar puncture (LP) has for a long time been of 55 patients with SAH who had LP, before the mainstay of diagnosis in patients who CT scanning and within 12 hours of the bleed. presented with symptoms or signs of subarach- Intracranial haematomas with brain shift was noid haemorrhage (SAH). At present, com- proven by operation or subsequent CT scan- puted tomography (CT) has replaced LP for ning in six of the seven patients, and it was this indication. In this review we shall outline suspected in the remaining patient who stop- the reasons for this change in diagnostic ped breathing at the end of the procedure.5 approach. In the first place, there are draw- Rebleeding may have occurred in some ofthese backs in starting with an LP. One of these is patients. that patients with SAH may harbour an We therefore agree with Hillman that it is intracerebral haematoma, even if they are fully advisable to perform a CT scan first in all conscious, and that withdrawal of cerebro- patients who present within 72 hours of a spinal fluid (CSF) may occasionally precipitate suspected SAH, even if this requires referral to brain shift and herniation. Another disadvan- another centre.4 tage of LP is the difficulty in distinguishing It could be argued that by first performing between a traumatic tap and true subarachnoid CT the diagnosis may be delayed and that this haemorrhage. -

Iatrogenic Spinal Subarachnoid Hematoma After Diagnostic Lumbar Puncture
https://doi.org/10.14245/kjs.2017.14.4.158 KJS Print ISSN 1738-2262 On-line ISSN 2093-6729 CASE REPORT Korean J Spine 14(4):158-161, 2017 www.e-kjs.org Iatrogenic Spinal Subarachnoid Hematoma after Diagnostic Lumbar Puncture Jung Hyun Park, Spinal subarachnoid hematoma (SSH) following diagnostic lumbar puncture is very rare. Generally, Jong Yeol Kim SSH is more likely to occur when the patient has coagulopathy or is undergoing anticoagulant therapy. Unlike the usual complications, such as headache, dizziness, and back pain at the Department of Neurosurgery, Kosin needle puncture site, SSH may result in permanent neurologic deficits if not properly treated University Gospel Hospital, Kosin within a short period of time. An otherwise healthy 43-year-old female with no predisposing University College of Medicine, factors presented with fever and headache. Diagnostic lumbar puncture was performed under Busan, Korea suspicion of acute meningitis. Lumbar magnetic resonance imaging was performed due to hypo- Corresponding Author: esthesia below the level of T10 that rapidly progressed after the lumbar puncture. SSH was Jong Yeol Kim diagnosed, and high-dose steroid therapy was started. Her neurological symptoms rapidly deterio- Department of Neurosurgery, rated after 12 hours despite the steroids, necessitating emergent decompressive laminectomy Kosin University Gospel Hospital, and hematoma removal. The patient’s condition improved after the surgery from a preoperative Kosin University College of Medicine, 262 Gamcheon-ro, Seo-gu, Busan motor score of 1/5 in the right leg and 4/5 in the left leg to brace-free ambulation (motor grade 49267, Korea 5/5) 3-month postoperative. -

What to Expect After Having a Subarachnoid Hemorrhage (SAH) Information for Patients and Families Table of Contents
What to expect after having a subarachnoid hemorrhage (SAH) Information for patients and families Table of contents What is a subarachnoid hemorrhage (SAH)? .......................................... 3 What are the signs that I may have had an SAH? .................................. 4 How did I get this aneurysm? ..................................................................... 4 Why do aneurysms need to be treated?.................................................... 4 What is an angiogram? .................................................................................. 5 How are aneurysms repaired? ..................................................................... 6 What are common complications after having an SAH? ..................... 8 What is vasospasm? ...................................................................................... 8 What is hydrocephalus? ............................................................................... 10 What is hyponatremia? ................................................................................ 12 What happens as I begin to get better? .................................................... 13 What can I expect after I leave the hospital? .......................................... 13 How will the SAH change my health? ........................................................ 14 Will the SAH cause any long-term effects? ............................................. 14 How will my emotions be affected? .......................................................... 15 When should -
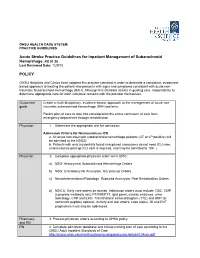
Acute Stroke Practice Guidelines for Inpatient Management of Subarachnoid Hemorrhage, PS 01.20 POLICY
OHSU HEALTH CARE SYSTEM PRACTICE GUIDELINES Acute Stroke Practice Guidelines for Inpatient Management of Subarachnoid Hemorrhage, PS 01.20 Last Reviewed Date: 1/29/10 POLICY OHSU Hospitals and Clinics have adopted this practice standard in order to delineate a consistent, evidenced- based approach to treating the patient who presents with signs and symptoms consistent with acute non- traumatic Subarachnoid Hemorrhage (SAH). Although this standard assists in guiding care, responsibility to determine appropriate care for each individual remains with the provider themselves. Outcomes/ Create a multi-disciplinary, evidence-based, approach to the management of acute non- goals traumatic subarachnoid hemorrhage (SAH) patients. Patient plan of care to take into consideration the entire continuum of care from emergency department through rehabilitation. Physician 1. Determine the appropriate unit for admission. Admission Criteria for Neurosciences ICU a. All acute non-traumatic subarachnoid hemorrhage patients (CT or LP positive) will be admitted to the NSICU. b. Patients with only incidentally found unruptured aneurysms do not need ICU care, unless routine post-op ICU care is required, and may be admitted to 10K. ( Physician 2. Complete appropriate physician order set in EPIC: a) NSG: Aneurysmal Subarachnoid Hemorrhage Orders. b) NSG: Craniotomy for Aneurysm: ICU post-op Orders. c) NeuroInterventional Radiology: Ruptured Aneurysm: Post Embolization Orders. d) NSICU: Daily care orders on rounds. Admission orders must include: CBC, CMP (complete metabolic set), PT/INR/PTT, lipid panel, cardiac enzymes, urine toxicology, CXR and EKG. Transthoracic echocardiogram (TTE) and BNP (B- natriuretic peptide) optional. Activity and diet orders, code status, GI and DVT prophylaxis must also be addressed. -

Simultaneous Cranial Subarachnoid Hemorrhage-Subdural Hematoma
Case Report/Olgu Sunumu İstanbul Med J 2021; 22(1): 81-3 DO I: 10.4274/imj.galenos.2020.73658 Simultaneous Cranial Subarachnoid Hemorrhage-Subdural Hematoma and Spinal Subarachnoid Hemorrhage Eşzamanlı Kraniyal Subaraknoid Kanama-Subdural Hematom ve Spinal Subaraknoid Kanama Hatice Kaplanoğlu1, Veysel Kaplanoğlu2, Aynur Turan1, Onur Karacif1 1University of Health Sciences Turkey, Dışkapı Yıldırım Beyazıt Training and Research Hospital, Clinic of Radiology, Ankara, Turkey 2University of Health Sciences Turkey, Keçiören Training and Research Hospital, Clinic of Radiology, Ankara, Turkey ABSTRACT ÖZ Patients with traumatic intracranial subarachnoid hemorrhage Çok nadiren, travmatik intrakraniyal subaraknoid hemorojisi (SAH) rarely develop spinal subarachnoid hemorrhage (SSAH) (SAH) olan hastalarda, doğrudan omurga yaralanması olmadan without direct spinal injury. We present the case of a 76-year- spinal subaraknoid kanama (SSAH) ortaya çıkabilir. Travmatik old male patient with traumatic intracranial SAH and subdural intrakraniyal SAH ve subdural hematomu olan 76 yaşındaki hematoma, back pain and weakness in the both lower erkek hastada, yoğun bakım takibi sırasında travmadan üç gün limbs radiating to the legs three days after the trauma. After sonra bacaklarına yayılan sırt ağrısı ve bilateral alt ekstremitede worsening of pain and numbness, the patient underwent a güçsüzlük ortaya çıktı. Ağrı ve uyuşmanın kötüleşmesi üzerine, lumbar magnetic resonance imaging 7 days after the trauma, travmadan 7 gün sonra hastaya lomber manyetik rezonans in which blood was seen in the spinal canal in the lumbosacral görüntüleme yapıldı. Lumbosakral bölgede intraspinal region. The bleeding was considered SSAH because of the kanama görüldü. Kanamanın sıvı seviyesi göstermesi liquid level. The patient underwent conservative treatment sebebiyle SSAH olarak değerlendirildi. Hasta kardiyak açıdan because the patient was found to be at high cardiac risk and yüksek riskli bulunduğu için ve nörolojik defisiti hafif olduğu the neurological deficit was mild. -

Subarachnoid Hemorrhage (SAH) (A Type of Hemorrhagic Stroke)
Subarachnoid Hemorrhage (SAH) (A type of Hemorrhagic Stroke) A Guide for Patients and Families in the Neurosurgery Intensive Care Unit Department of Neurosurgery Introduction A team of doctors and nurses at The University of Michigan Neurosurgery Intensive Care Unit (Neuro ICU) wrote this booklet for patients who have had a Subarachnoid Hemorrhage (SAH) and for the family members and friends who care about them. The purpose of this booklet is to give answers to questions about the illness and treatment of SAH and about what you can expect during your stay in the Neuro ICU. If you have any additional questions, please ask a Neurosurgery team member. Table of Contents: What is SAH?............................................................................4 What causes SAH?....................................................4 What are the risk factors for SAH?......................5 Treating SAH at the University of Michigan...................6 Reducing possible side-effects………………….8 Preventing a secondary stroke from cerebral vasospasm………………………………………… 8 What you need to know about your hospital stay…..10 How long will it last?.............................................10 The dangers of being bed bound.......................10 How can family and friends help patients achieve the best outcomes?...............................................................10 Your partnership with the Neuro ICU team................ 12 What is the best way to keep informed about a patient’s clinical status?........................................................12 -

Intracranial Hemorrhage
Intracranial Hemorrhage MARK MOSS, M.D. INTERVENTIONAL NEURORADIOLOGY WASHINGTON REGIONAL MEDICAL CENTER Definitions Stroke Clinical syndrome of rapid onset deficits of brain function lasting more than 24 hours or leading to death Transient Ischemic attack (TIA) Clinical syndrome of rapid onset deficits of brain function which resolves within 24 hours Epidemiology Stroke is the leading cause of adult disabilities 2nd leading cause of death worldwide 3rd leading cause of death in the U.S. 800,000 strokes per year resulting in 150,000 deaths Deaths are projected to increase exponentially in the next 30 years owing to the aging population The annual cost of stroke in the U.S. is estimated at $69 billion Stroke can be divided into hemorrhagic and ischemic origins 13% hemorrhagic 87% ischemic Intracranial Hemorrhage Collective term encompassing many different conditions characterized by the extravascular accumulation of blood within different intracranial spaces. OBJECTIVES: Define types of ICH Discuss best imaging modalities Subarachnoid hemorrhage / Aneurysms Roles of endovascular surgery Intracranial hemorrhage Outside the brain (Extra-axial) hemorrhage Subdural hematoma (SDH) Epidural hematoma (EDH) Subarachnoid hematoma (SAH) Intraventricular (IVH) Inside the brain (Intra-axial) hemorrhage Intraparenchymal hematoma (basal ganglia, lobar, pontine etc.) Your heads compartments Scalp Subgaleal Space Bone (calvarium) Dura Mater thick tough membrane Arachnoid flimsy transparent membrane Pia Mater tightly hugs the -

Primary Intracerebral and Subarachnoid Hemorrhage
PRIMARY INTRACEREBRAL AND SUBARACHNOID HEMORRHAGE AN APPROACH TO DIAGNOSIS AND THERAPY MARC FISHER * SUMMARY — The diagnosis of primary intracerebral hemorrhage (ICH) and subarachnoid hemorrhage (SAH) has become easier with the advent of modern imaging techniques. The incidence of ICH has declined, while SAH has remained relatively constant. The prognosis for both disorders remains dismal and the mortality rate is substantially higher than that observed with ischemic stroke. Early imaging with CT or MRI is important for rapid and accurate diagnosis. General medical management in a skilled nursing facility should be available for patients who are not moribund. Therapy for ICH is predominantly supportive and effective medical and surgical intervention remains elusive. For SAH, calcium channel blockers may reduce cerebral ischemic complications related to vasospasm, but effective medical therapy to prevent rebleeding has not been established. Early surgery after SAH should be considered in clinically stable patients. Many challenges remain regarding the prevention and treatment of both these cerebral hemorrhage subtypes. Hemorragia intracerebral primária e subaracnóidea: uma avaliação do diagnóstico e da terapêutica. RESUMO — O diagnóstico da hemorragia intracerebral primária (HIP), bem como o da hemorragia subaracnóidea (HSA), ficou mais fácil com o advento das modernas técnicas de imagem. A incidência da HIC tem declinado, ao passo que a da HSA tem permanecido relativamente constante. O prognóstico de ambas ainda é desanimador e a taxa de morta lidade substancialmente maior que a observada nas afecções isquêmicas. A indicação pre coce da TC ou da RNM do crânio é importante para um diagnóstico rápido e preciso. Pacientes que não estejam moribundos devem receber cuidados médicos gerais em instalações com equipes de enfermagem especializada. -

Emergencykt: Isolated Mild Traumatic Brain Injury
EmergencyKT: Isolated Mild Traumatic Brain Injury Table 1: Types of Hemorrhages Subarachnoid hemorrhage, subdural hematoma, epidural hematoma, intra- parenchymal hemorrhage, cerebral contusion Examples of Head CT findings suitable for Observation Protocol: 1. Convexity Subarachnoid Hemorrhage 2. Punctate Contusions (no more than 5) 3. Rim Subdural along Convexity Table 2: Inclusions and Exclusions from Protocol Inclusion Criteria: Adult patients who sustain an isolated head injury with a GCS 14 or 15 may be included in the ED mild TBI observation protocol. Patients may have a normal or abnormal head CT. Patients will be excluded from protocol if found to have any of the following features: 1. Any patient with INR >3.0 is excluded. Patients with an INR ≥1.5 may only have a hemorrhage listed in Table 4. Please see Table 4 for eligibility of patients on Coumadin. 2. Patient is on a factor Xa inhibitor or a direct thrombin inhibitor. 3. Objective new neurologic exam findings/deficits (e.g. aphasia, hemiparesis, weakness, etc.) 4. Intoxicated patients with negative head CT who need only to achieve sobriety prior to discharge 5. Patients who require intense nursing attention, direct line of sight and/or are restrained 6. Hemorrhages that require neurosurgical intervention or bleeds determined to be unsuitable for observation (please see Table 1) 7. Patients who are greater than 24 hours after their injury with new neurologic symptoms 8. Multiple traumatic injuries or any other severe traumatic injury 9. Patients with actively declining mental status 10. Vital sign abnormalities: BP>190/110 or <85/50; HR>120 or <45; O2<91% on RA 11. -

Traumatic Brain Injury and Intracranial Hemorrhage–Induced Cerebral Vasospasm:A Systematic Review
NEUROSURGICAL FOCUS Neurosurg Focus 43 (5):E14, 2017 Traumatic brain injury and intracranial hemorrhage–induced cerebral vasospasm: a systematic review Fawaz Al-Mufti, MD,1,2 Krishna Amuluru, MD,2 Abhinav Changa, BA,2 Megan Lander, BA,2 Neil Patel, BA,2 Ethan Wajswol, BS,2 Sarmad Al-Marsoummi, MBChB,5 Basim Alzubaidi, MD,1 I. Paul Singh, MD, MPH,2,4 Rolla Nuoman, MD,3 and Chirag Gandhi, MD2–4 1Department of Neurology, Rutgers Robert Wood Johnson Medical School, New Brunswick; Departments of 2Neurosurgery, 3Neurology, and 4Radiology, Rutgers University, New Jersey Medical School, Newark, New Jersey; and 5University of North Dakota, Grand Forks, North Dakota OBJECTIVE Little is known regarding the natural history of posttraumatic vasospasm. The authors review the patho- physiology of posttraumatic vasospasm (PTV), its associated risk factors, the efficacy of the technologies used to detect PTV, and the management/treatment options available today. METHODS The authors performed a systematic review in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines using the following databases: PubMed, Google Scholar, and CENTRAL (the Cochrane Central Register of Controlled Trials). Outcome variables extracted from each study included epidemiology, pathophysiology, time course, predictors of PTV and delayed cerebral ischemia (DCI), optimal means of surveillance and evaluation of PTV, application of multimodality monitoring, modern management and treatment op- tions, and patient outcomes after PTV. Study types were limited to retrospective chart reviews, database reviews, and prospective studies. RESULTS A total of 40 articles were included in the systematic review. In many cases of mild or moderate traumatic brain injury (TBI), imaging or ultrasonographic studies are not performed. -

Types of Brain Injury
Tipos de lesiones cerebrales Types of Brain Injury The bones of the skull are hard to protect the Los huesos del cráneo son duros para brain. When your head is hit or moved with proteger el cerebro. Cuando la cabeza se force, the brain is injured when it moves at a golpea o se mueve con fuerza, el cerebro se different speed than the skull. The brain or a lesiona cuando se mueve a una velocidad part of the brain can be bruised, stretched or diferente a la del cráneo. El cerebro o una torn to cause bleeding. parte de este puede sufrir un moretón, un A person may have one or several types of estiramiento o un desgarro que provoque brain injury. Recovering from a brain injury una hemorragia. can take a long time. Read on to learn about Una persona puede tener uno o varios tipos the different types of brain injury. de lesión cerebral. Recuperarse de una lesión cerebral puede llevar mucho tiempo. Siga leyendo para conocer los diferentes tipos de lesiones cerebrales. Concussion Conmoción cerebral A concussion is the most common type of La conmoción cerebral es el tipo más traumatic brain injury. It results from a fall or común de lesión cerebral traumática. Es hit to the head that causes the brain to twist el resultado de una caída o un golpe en la and turn inside the skull. cabeza que hace que el cerebro se tuerza y A concussion may cause bruising, bleeding gire dentro del cráneo. or swelling of the brain. A skull fracture may Una conmoción cerebral puede provocar occur along with a concussion. -

Migraine, White Matter Lesions and Subarachnoid Hemorrhage: Analysis Ofa Large Pedigree Migren, Ak Madde Ve Subaraknoid Kanama: Bir Aile Analizi
162 Case Report / Olgu Sunumu DOi: 10.4274inpa 47 5425 Migraine, White Matter Lesions and Subarachnoid Hemorrhage: Analysis ofa Large Pedigree Migren, Ak Madde ve Subaraknoid Kanama: Bir Aile Analizi Zeliha MATUR, Mürüwet POYRAZ*, Oya UYGUNER**, Hülya KAYSERiLi, Betül GÜVELi***, Betül BAYKAN lstanbul Üniversitesi lstanbul Fakültesi, Nöroloji Ana bilim lstanbul, Türkiye Hatun Merkezi, Nöroloji Bölümü, lstanbul, Türkiye ''lstanbul Üniversitesi lstanbul Fakültesi, Genetik Anabilim lstanbul, Türkiye Gureba Egitim ve Hastanesi, Nöroloji Klinigi, lstanbul, Türkiye ABSTRACT ÖZET Patients with migraine are at increased risk tor white matter hyperintensities Migrenli hastalarda manyetik rezonans görüntülemede IMRG) ak madde detected on magnetic resonance imaging (MAii. A 46-year-old woman had a tensitelerin saptanma 20 history of migraine with and without aura tor 20 years. Bilateral prominent ve migreni 12 ve FLAIR MRG hyperintense lesions were seen in centrum semiovale, posterior corona radia- sentrum semiovale, posterior korona radiata, trontal ak madde ve ta, frontal white matter and periventricular regions on her T2- and triküler bölgelerde hiperintens lezyonlar görüldü. On üç aile bireyinde öy- FLAIA-weighted cranial MRls. Thirteen members of her family, including her küsü ve benzer MAG lezyonlan migrenli oQlunda da görüldü. ilginç olarak üç son, hada history of migraine and similar brain MRI lesions. Furthermore, three aile bireyinde subaraknoid kanama (SAKI ve bir aile bireyinde intrakranyal anev- family members had a history of subarachnoid hemorrhage (SAH) and one rizma öyküsü mevcuttu. Önemi bilinmeyen ak madde olan migrenli has- member had intracranial aneurysm. Dur current knowledge on associations, olduQu durumlar, inceleme ve tedavileri bugünkü investigation plan and of patients with migraine with white matter bilgilerimiz Bu durumun ailesel SAK ile birlikteliQi ilk kez bu of unknown is limited.