Emergencykt: Isolated Mild Traumatic Brain Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Diagnosis of Subarachnoid Haemorrhage
Journal ofNeurology, Neurosurgery, and Psychiatry 1990;53:365-372 365 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.53.5.365 on 1 May 1990. Downloaded from OCCASIONAL REVIEW The diagnosis of subarachnoid haemorrhage M Vermeulen, J van Gijn Lumbar puncture (LP) has for a long time been of 55 patients with SAH who had LP, before the mainstay of diagnosis in patients who CT scanning and within 12 hours of the bleed. presented with symptoms or signs of subarach- Intracranial haematomas with brain shift was noid haemorrhage (SAH). At present, com- proven by operation or subsequent CT scan- puted tomography (CT) has replaced LP for ning in six of the seven patients, and it was this indication. In this review we shall outline suspected in the remaining patient who stop- the reasons for this change in diagnostic ped breathing at the end of the procedure.5 approach. In the first place, there are draw- Rebleeding may have occurred in some ofthese backs in starting with an LP. One of these is patients. that patients with SAH may harbour an We therefore agree with Hillman that it is intracerebral haematoma, even if they are fully advisable to perform a CT scan first in all conscious, and that withdrawal of cerebro- patients who present within 72 hours of a spinal fluid (CSF) may occasionally precipitate suspected SAH, even if this requires referral to brain shift and herniation. Another disadvan- another centre.4 tage of LP is the difficulty in distinguishing It could be argued that by first performing between a traumatic tap and true subarachnoid CT the diagnosis may be delayed and that this haemorrhage. -

Iatrogenic Spinal Subarachnoid Hematoma After Diagnostic Lumbar Puncture
https://doi.org/10.14245/kjs.2017.14.4.158 KJS Print ISSN 1738-2262 On-line ISSN 2093-6729 CASE REPORT Korean J Spine 14(4):158-161, 2017 www.e-kjs.org Iatrogenic Spinal Subarachnoid Hematoma after Diagnostic Lumbar Puncture Jung Hyun Park, Spinal subarachnoid hematoma (SSH) following diagnostic lumbar puncture is very rare. Generally, Jong Yeol Kim SSH is more likely to occur when the patient has coagulopathy or is undergoing anticoagulant therapy. Unlike the usual complications, such as headache, dizziness, and back pain at the Department of Neurosurgery, Kosin needle puncture site, SSH may result in permanent neurologic deficits if not properly treated University Gospel Hospital, Kosin within a short period of time. An otherwise healthy 43-year-old female with no predisposing University College of Medicine, factors presented with fever and headache. Diagnostic lumbar puncture was performed under Busan, Korea suspicion of acute meningitis. Lumbar magnetic resonance imaging was performed due to hypo- Corresponding Author: esthesia below the level of T10 that rapidly progressed after the lumbar puncture. SSH was Jong Yeol Kim diagnosed, and high-dose steroid therapy was started. Her neurological symptoms rapidly deterio- Department of Neurosurgery, rated after 12 hours despite the steroids, necessitating emergent decompressive laminectomy Kosin University Gospel Hospital, and hematoma removal. The patient’s condition improved after the surgery from a preoperative Kosin University College of Medicine, 262 Gamcheon-ro, Seo-gu, Busan motor score of 1/5 in the right leg and 4/5 in the left leg to brace-free ambulation (motor grade 49267, Korea 5/5) 3-month postoperative. -

What to Expect After Having a Subarachnoid Hemorrhage (SAH) Information for Patients and Families Table of Contents
What to expect after having a subarachnoid hemorrhage (SAH) Information for patients and families Table of contents What is a subarachnoid hemorrhage (SAH)? .......................................... 3 What are the signs that I may have had an SAH? .................................. 4 How did I get this aneurysm? ..................................................................... 4 Why do aneurysms need to be treated?.................................................... 4 What is an angiogram? .................................................................................. 5 How are aneurysms repaired? ..................................................................... 6 What are common complications after having an SAH? ..................... 8 What is vasospasm? ...................................................................................... 8 What is hydrocephalus? ............................................................................... 10 What is hyponatremia? ................................................................................ 12 What happens as I begin to get better? .................................................... 13 What can I expect after I leave the hospital? .......................................... 13 How will the SAH change my health? ........................................................ 14 Will the SAH cause any long-term effects? ............................................. 14 How will my emotions be affected? .......................................................... 15 When should -
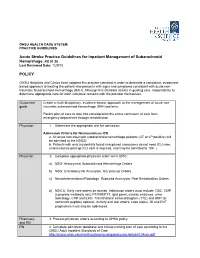
Acute Stroke Practice Guidelines for Inpatient Management of Subarachnoid Hemorrhage, PS 01.20 POLICY
OHSU HEALTH CARE SYSTEM PRACTICE GUIDELINES Acute Stroke Practice Guidelines for Inpatient Management of Subarachnoid Hemorrhage, PS 01.20 Last Reviewed Date: 1/29/10 POLICY OHSU Hospitals and Clinics have adopted this practice standard in order to delineate a consistent, evidenced- based approach to treating the patient who presents with signs and symptoms consistent with acute non- traumatic Subarachnoid Hemorrhage (SAH). Although this standard assists in guiding care, responsibility to determine appropriate care for each individual remains with the provider themselves. Outcomes/ Create a multi-disciplinary, evidence-based, approach to the management of acute non- goals traumatic subarachnoid hemorrhage (SAH) patients. Patient plan of care to take into consideration the entire continuum of care from emergency department through rehabilitation. Physician 1. Determine the appropriate unit for admission. Admission Criteria for Neurosciences ICU a. All acute non-traumatic subarachnoid hemorrhage patients (CT or LP positive) will be admitted to the NSICU. b. Patients with only incidentally found unruptured aneurysms do not need ICU care, unless routine post-op ICU care is required, and may be admitted to 10K. ( Physician 2. Complete appropriate physician order set in EPIC: a) NSG: Aneurysmal Subarachnoid Hemorrhage Orders. b) NSG: Craniotomy for Aneurysm: ICU post-op Orders. c) NeuroInterventional Radiology: Ruptured Aneurysm: Post Embolization Orders. d) NSICU: Daily care orders on rounds. Admission orders must include: CBC, CMP (complete metabolic set), PT/INR/PTT, lipid panel, cardiac enzymes, urine toxicology, CXR and EKG. Transthoracic echocardiogram (TTE) and BNP (B- natriuretic peptide) optional. Activity and diet orders, code status, GI and DVT prophylaxis must also be addressed. -

NIH Public Access Author Manuscript J Neuropathol Exp Neurol
NIH Public Access Author Manuscript J Neuropathol Exp Neurol. Author manuscript; available in PMC 2010 September 24. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: J Neuropathol Exp Neurol. 2009 July ; 68(7): 709±735. doi:10.1097/NEN.0b013e3181a9d503. Chronic Traumatic Encephalopathy in Athletes: Progressive Tauopathy following Repetitive Head Injury Ann C. McKee, MD1,2,3,4, Robert C. Cantu, MD3,5,6,7, Christopher J. Nowinski, AB3,5, E. Tessa Hedley-Whyte, MD8, Brandon E. Gavett, PhD1, Andrew E. Budson, MD1,4, Veronica E. Santini, MD1, Hyo-Soon Lee, MD1, Caroline A. Kubilus1,3, and Robert A. Stern, PhD1,3 1 Department of Neurology, Boston University School of Medicine, Boston, Massachusetts 2 Department of Pathology, Boston University School of Medicine, Boston, Massachusetts 3 Center for the Study of Traumatic Encephalopathy, Boston University School of Medicine, Boston, Massachusetts 4 Geriatric Research Education Clinical Center, Bedford Veterans Administration Medical Center, Bedford, Massachusetts 5 Sports Legacy Institute, Waltham, MA 6 Department of Neurosurgery, Boston University School of Medicine, Boston, Massachusetts 7 Department of Neurosurgery, Emerson Hospital, Concord, MA 8 CS Kubik Laboratory for Neuropathology, Department of Pathology, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts Abstract Since the 1920s, it has been known that the repetitive brain trauma associated with boxing may produce a progressive neurological deterioration, originally termed “dementia pugilistica” and more recently, chronic traumatic encephalopathy (CTE). We review the 47 cases of neuropathologically verified CTE recorded in the literature and document the detailed findings of CTE in 3 professional athletes: one football player and 2 boxers. -

Simultaneous Cranial Subarachnoid Hemorrhage-Subdural Hematoma
Case Report/Olgu Sunumu İstanbul Med J 2021; 22(1): 81-3 DO I: 10.4274/imj.galenos.2020.73658 Simultaneous Cranial Subarachnoid Hemorrhage-Subdural Hematoma and Spinal Subarachnoid Hemorrhage Eşzamanlı Kraniyal Subaraknoid Kanama-Subdural Hematom ve Spinal Subaraknoid Kanama Hatice Kaplanoğlu1, Veysel Kaplanoğlu2, Aynur Turan1, Onur Karacif1 1University of Health Sciences Turkey, Dışkapı Yıldırım Beyazıt Training and Research Hospital, Clinic of Radiology, Ankara, Turkey 2University of Health Sciences Turkey, Keçiören Training and Research Hospital, Clinic of Radiology, Ankara, Turkey ABSTRACT ÖZ Patients with traumatic intracranial subarachnoid hemorrhage Çok nadiren, travmatik intrakraniyal subaraknoid hemorojisi (SAH) rarely develop spinal subarachnoid hemorrhage (SSAH) (SAH) olan hastalarda, doğrudan omurga yaralanması olmadan without direct spinal injury. We present the case of a 76-year- spinal subaraknoid kanama (SSAH) ortaya çıkabilir. Travmatik old male patient with traumatic intracranial SAH and subdural intrakraniyal SAH ve subdural hematomu olan 76 yaşındaki hematoma, back pain and weakness in the both lower erkek hastada, yoğun bakım takibi sırasında travmadan üç gün limbs radiating to the legs three days after the trauma. After sonra bacaklarına yayılan sırt ağrısı ve bilateral alt ekstremitede worsening of pain and numbness, the patient underwent a güçsüzlük ortaya çıktı. Ağrı ve uyuşmanın kötüleşmesi üzerine, lumbar magnetic resonance imaging 7 days after the trauma, travmadan 7 gün sonra hastaya lomber manyetik rezonans in which blood was seen in the spinal canal in the lumbosacral görüntüleme yapıldı. Lumbosakral bölgede intraspinal region. The bleeding was considered SSAH because of the kanama görüldü. Kanamanın sıvı seviyesi göstermesi liquid level. The patient underwent conservative treatment sebebiyle SSAH olarak değerlendirildi. Hasta kardiyak açıdan because the patient was found to be at high cardiac risk and yüksek riskli bulunduğu için ve nörolojik defisiti hafif olduğu the neurological deficit was mild. -

Subarachnoid Hemorrhage (SAH) (A Type of Hemorrhagic Stroke)
Subarachnoid Hemorrhage (SAH) (A type of Hemorrhagic Stroke) A Guide for Patients and Families in the Neurosurgery Intensive Care Unit Department of Neurosurgery Introduction A team of doctors and nurses at The University of Michigan Neurosurgery Intensive Care Unit (Neuro ICU) wrote this booklet for patients who have had a Subarachnoid Hemorrhage (SAH) and for the family members and friends who care about them. The purpose of this booklet is to give answers to questions about the illness and treatment of SAH and about what you can expect during your stay in the Neuro ICU. If you have any additional questions, please ask a Neurosurgery team member. Table of Contents: What is SAH?............................................................................4 What causes SAH?....................................................4 What are the risk factors for SAH?......................5 Treating SAH at the University of Michigan...................6 Reducing possible side-effects………………….8 Preventing a secondary stroke from cerebral vasospasm………………………………………… 8 What you need to know about your hospital stay…..10 How long will it last?.............................................10 The dangers of being bed bound.......................10 How can family and friends help patients achieve the best outcomes?...............................................................10 Your partnership with the Neuro ICU team................ 12 What is the best way to keep informed about a patient’s clinical status?........................................................12 -

Post-Concussion Syndrome
Post-Concussion Syndrome BY DAVID COPPEL Over the last decade, sport-related concussions have fatigue, irritability, sleep disturbance and sensitivity to become an important focus within the general sports inju- light and noise may continue over the next few days. Oth- WHAT CAN COACHES DO? ry and sports medicine field. Clinical and research studies SIGNS AND SYMPTOMS • Make sure student-athletes who sustain a concus- er symptoms seen on post-concussion symptom checklists According to the Diagnostic and Statistical Manual regarding this form/context of mild traumatic brain injury sion are immediately removed from play and that include attention and concentration difficulties, slowed of Mental Disorders – 4th edition (DSM-4) – an individu- have increased geometrically as its position as a public they do not feel pressure from the coaching staff to processing, distractibility, memory problems, slowed visu- al with post-concussion disorder experiences objective health concern elevated and the Centers for Disease Con- return to play before fully recovered. Communicating al tracking or vision problems, balance disturbance, and declines in attention, concentration, learning or memo- with team members before the season about con- trol and Prevention (CDC) became involved. ry. The individual also reports three or more subjective anxiety or depressed mood. Typically, depressed mood or cussion safety, and verbally reinforcing the impor- The CDC has compiled guidelines and resources for symptoms, present for at least three months: tance of concussion safety throughout the season health care providers, coaches, parents and athletes re- • Becoming fatigued easily are important ways to encourage student-athletes garding concussions. Great progress has been made in • Disordered sleep to feel comfortable reporting concussion symptoms WHAT CAN ATHLETIC • Headache understanding and managing sport-related concussions, to medical personnel. -

Concussion Guide for Coaches
Concussion Guide for Youth and High School Coaches SIGNS OBSERVED BY COACHING STAFF THE FACTS • Appears dazed or stunned (such as glassy eyes) • All concussions are serious. • Is confused about assignment or position • Most concussions occur without loss of • Forgets an instruction or play consciousness. • Is unsure of score or opponent • Recognition and proper response to concussions • Moves clumsily or poor balance when they first occur can help aid recovery and • Answers questions slowly prevent further injury, or even death. • Loses consciousness (even briefly) • Shows mood, behavior, or personality changes • Can’t recall events prior to hit or fall A bump, blow, or jolt to the head can cause a concussion, • Can’t recall events after hit or fall a type of traumatic brain injury (TBI). Concussions can also occur from a blow to the body that causes the head and brain to move rapidly back and forth. Even a “ding,” SYMPTOMS REPORTED BY ATHLETE “getting your bell rung,” or what seems to be mild bump • Headache or “pressure” in head or blow to the head can be serious. • Nausea or vomiting • Balance problems or dizziness • Double or blurry vision RECOGNIZING A POSSIBLE CONCUSSION • Sensitivity to light or noise To help recognize a concussion, watch for or ask others to • Feeling sluggish, hazy, foggy, or groggy report the following two things among your athletes: • Concentration or memory problems 1. A forceful bump, blow, or jolt to the head or body • Confusion that results in rapid movement of the head. • Feeling more emotional, nervous, or anxious – and – • Does not “feel right” or is “feeling down” 2. -

The Relationships Between Rugby Union, and Health and Well-Being
Review Br J Sports Med: first published as 10.1136/bjsports-2020-102085 on 28 October 2020. Downloaded from The relationships between rugby union, and health and well- being: a scoping review Steffan A Griffin ,1,2 Nirmala Kanthi Panagodage Perera ,3,4 Andrew Murray ,1,5 Catherine Hartley ,6 Samantha G Fawkner,7 Simon P T Kemp ,2,8 Keith A Stokes ,2,9 Paul Kelly 10 1Centre for Sport and Exercise, ABSTRACT Indeed, there are widely published health benefits The University of Edinburgh, Objective To scope the relationships between rugby associated with participating in various individual Edinburgh, UK 7 8 2 and team sports, including improved aerobic Medical Services, Rugby union, and health and well- being. Football Union, London, UK Design Scoping review. fitness, cardiovascular function, metabolic fitness 3Centre for Sport, Exercise and Data sources Published and unpublished reports of and in some cases reduced mortality.9 Sport is also Osteoarthritis Research Versus any age, identified by searching electronic databases, considered an ‘underused yet important’ contrib- Arthritis, Botnar Research platforms and reference lists. utor to physical activity (PA) and health10 in the Centre, University of Oxford, Oxford, UK Methods A three- step search strategy identified World Health Organisation’s (WHO) 2019 Global 4Sports Medicine, Australian relevant published primary, secondary studies and grey Action Plan for Physical Activity. Institute of Sport, Bruce, literature, which were screened using a priori inclusion Despite global participation in rugby union, there Australian Capital Territory, criteria. Data were extracted using a standardised tool, has not been an overarching review of the evidence Australia 5 on the specific relationships between rugby union, Scottish Rugby Union, to form (1) a numerical analysis and (2) a thematic Edinburgh, UK summary. -

Mild Traumatic Brain Injury and Concussion: Information for Adults
Mild Traumatic Brain Injury and Concussion: Information for Adults Discharge Instructions You were seen today for a mild traumatic brain injury (mild TBI) or concussion. Watch for Danger Signs Use this handout to help you watch In rare cases, a dangerous blood clot that for changes in how you are feeling crowds the brain against the skull can develop or acting and to help you feel better. after a TBI. The people checking on you should call 911 or take you to an emergency Be sure to let a family member or department right away if you have: friend know about your injury and the types of symptoms to look out • A headache that gets worse and does not for. They may notice symptoms go away before you do and can help you. • Significant nausea or repeated vomiting • Unusual behavior, increased confusion, Schedule a follow-up appointment restlessness, or agitation with your regular doctor. • Drowsiness or inability to wake up Due to your injury, you may need to take some • Slurred speech, weakness, numbness, or time off from things like work or school. If so, ask decreased coordination your doctor for written instructions about when • Convulsions or seizures (shaking or you can safely return to work, school, sports, twitching) or other activities such as driving a car, riding a • Loss of consciousness (passing out) bike, or operating heavy equipment. More information on mild TBI and concussion, as well as tips to help you feel better, can be found at www.cdc.gov/TraumaticBrainInjury. Learn About Your Injury Mild TBI and concussions are brain injuries. -
Concussion and Epilepsy: What Is the Link?
COVER STORY Concussion and Epilepsy: What is the Link? Individuals who suffer a traumatic brain injury are at increased risk for developing seizures. Here’s an update the current evidence and implications for monitoring. INSIGHTS FROM G. ALEXANDER HISHAW, MD ccording to a 2003 report by the CDC, mild trau- matic injury results in roughly 500,000 emergency Significant risk factors for later department visits without hospitalization and seizures included brain contusion almost 200,000 hospitalizations per year. However, Ait’s believed this number is an underestimate because a with subdural hematoma, skull number of people with mild traumatic brain injury (TBI) fracture, loss of consciousness or are never seen in an ED. Increasingly, TBI is associated with amnesia for more than one day, and various neurolgical sequelae, as listed in Table 1. Among these, is epilepsy. age of 65 years or older. A population study in seizures after TBI by John Annegers, et al. showed that the standardized incidence UNDERSTANDING THE INJURY ratio was 1.5 after mild injury, 2.9 after moderate injury, According to the Department of Defense definition, acute and 17 after severe injury. Significant risk factors for later injury results from primary (mechanical) physical disrup- seizures included brain contusion with subdural hema- toma, skull fracture, loss of consciousness or amnesia for TABLE 1. NEUROLOGICAL CONDITIONS more than one day, and an age of 65 years or older. LINKED TO TBI Additional data are available from the Southern Arizona VA registry, which show: of 184 patients with TBI, three • Epilepsy percent of mild TBI cases experienced seizures, five per- • Dissociation cent of moderate TBI cases experienced seizures, and 32 • Frontal lobe syndrome percent of severe TBI cases experienced seizures.