Primary Intracerebral and Subarachnoid Hemorrhage
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Management of the Head Injury Patient
Management of the Head Injury Patient William Schecter, MD Epidemilogy • 1.6 million head injury patients in the U.S. annually • 250,000 head injury hospital admissions annually • 60,000 deaths • 70-90,000 permanent disability • Estimated cost: $100 billion per year Causes of Brain Injury • Motor Vehicle Accidents • Falls • Anoxic Encephalopathy • Penetrating Trauma • Air Embolus after blast injury • Ischemia • Intracerebral hemorrhage from Htn/aneurysm • Infection • tumor Brain Injury • Primary Brain Injury • Secondary Brain Injury Primary Brain Injury • Focal Brain Injury – Skull Fracture – Epidural Hematoma – Subdural Hematoma – Subarachnoid Hemorrhage – Intracerebral Hematorma – Cerebral Contusion • Diffuse Axonal Injury Fracture at the Base of the Skull Battle’s Sign • Periorbital Hematoma • Battle’s Sign • CSF Rhinorhea • CSF Otorrhea • Hemotympanum • Possible cranial nerve palsy http://health.allrefer.com/pictures-images/ Fracture of maxillary sinus causing CSF Rhinorrhea battles-sign-behind-the-ear.html Skull Fractures Non-depressed vs Depressed Open vs Closed Linear vs Egg Shell Linear and Depressed Normal Depressed http://www.emedicine.com/med/topic2894.htm Temporal Bone Fracture http://www.vh.org/adult/provider/anatomy/ http://www.bartleby.com/107/illus510.html AnatomicVariants/Cardiovascular/Images0300/0386.html Epidural Hematoma http://www.chestjournal.org/cgi/content/full/122/2/699 http://www.bartleby.com/107/illus769.html Epidural Hematoma • Uncommon (<1% of all head injuries, 10% of post traumatic coma patients) • Located -

Hypertensive Intracerebral Hemorrhage Due to Autonomic Dysreflexia in a Young Man with Cervical Cord Injury
J UOEH(産業医科大学雑誌)35( 2 ): 159-164(2013) 159 [Case Report] Hypertensive Intracerebral Hemorrhage Due to Autonomic Dysreflexia in a Young Man with Cervical Cord Injury Tadashi Sumiya Department of Spinal Care Center, Division of Rehabilitation Medicine 219 Myoji, Katsuragi-cho, Ito-gun, 649-7113, Japan Abstract : The author reports the case of a 36 year old man with cervical cord injury in whom autonomic dysreflexia developed into intracerebral hemorrhage during inpatient rehabilitation. This patient showed complete quadriplegia (motor below C6 and sensory below C7) due to fracture of the 6th cervical vertebra. An indwelling urethral catheter had been inserted into the bladder for 3 months, diminishing bladder expansiveness. Bladder capacity decreased to 200 ml and the patient frequently experienced headaches whenever his bladder was full. To obtain smoother urine flow, a supra-pubic cystostomy was performed. The headaches were temporarily cured, but soon relapsed with extreme increases in blood pressure, representing typical symptoms of autonomic dysreflexia. However, no poten- tial triggers were identified or removed, and lack of blood pressure management led to left putaminal hemorrhage. Despite operative treatment, the right upper extremity showed progressive increases in muscle tonus and finally formed a frozen shoulder with elbow flexion contracture. Two factors contributed to this serious complication: first, autonomic dysreflexia triggered by minor malfunction and/or irritation from the cystostomy catheter; and second, the medical staff lacked sufficient experience in and knowledge about the management of autonomic dysreflexia. It is of the utmost importance for medical staff engaging in rehabilitation of spinal patients to share information regard- ing triggers of autonomic dysreflexia and to be thorough in ensuring proper medical management. -

Intracerebral Hemorrhage ICH Fact Sheet
FACT SHEET FOR PATIENTS AND FAMILIES Intracerebral Hemorrhage (ICH) What is it? An intracerebral [in-truh-suh-REE-bruh l] hemorrhage [HEM-rij], Dura mater or ICH, is bleeding inside or around the brain, which Brain Skull can put pressure on the brain. An ICH robs the brain Intracerebral of oxygen, so it must be identified and managed right hemorrhage away. Other names for ICH are cerebral hemorrhage or intracranial [in-truh-KREY-nee-uh l] hemorrhage. ICH can happen because of trauma or as a result of no known cause (spontaneous ICH), which is a type of stroke called a hemorrhagic [hem-oh-RAJ-ik] stroke. In the U.S. each year, about 1 in 10 people who have strokes do so because of an ICH. Stroke is the leading cause of disability and the 5th-leading cause of death in the U.S. What are the symptoms of spontaneous ICH? Spontaneous ICH symptoms usually develop suddenly, without warning. Key symptoms can include a SUDDEN (see BE FAST on page 2): What causes it? • Loss of balance or coordination An ICH is often caused by a blood vessel leaking or • Change in vision breaking. This can be the result of: • Weakness of the face, arm, or leg • High blood pressure that has damaged a blood vessel • Difficulty speaking • Smoking, overuse of alcohol, or use of illegal drugs Other ICH symptoms can include: such as cocaine or methamphetamine • Severe headache with no known cause (patients • Diabetes often describe it as “the worst headache of my life”) • Abnormal blood vessel proteins in the elderly • Seizures An ICH can also be caused by: • Vomiting or severe nausea, when combined with • Anticoagulant therapy (treatment with blood thinners) other symptoms from this list • Problems with vein structure • Partial or total loss of conciousness • A brain tumor that bleeds • Head injuries caused by a fall or accident 1 How is it diagnosed? What can I expect afterward? Your doctor will explain what tests will be used to Your long-term outlook depends on the location and diagnose ICH, depending on your condition. -

The Diagnosis of Subarachnoid Haemorrhage
Journal ofNeurology, Neurosurgery, and Psychiatry 1990;53:365-372 365 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.53.5.365 on 1 May 1990. Downloaded from OCCASIONAL REVIEW The diagnosis of subarachnoid haemorrhage M Vermeulen, J van Gijn Lumbar puncture (LP) has for a long time been of 55 patients with SAH who had LP, before the mainstay of diagnosis in patients who CT scanning and within 12 hours of the bleed. presented with symptoms or signs of subarach- Intracranial haematomas with brain shift was noid haemorrhage (SAH). At present, com- proven by operation or subsequent CT scan- puted tomography (CT) has replaced LP for ning in six of the seven patients, and it was this indication. In this review we shall outline suspected in the remaining patient who stop- the reasons for this change in diagnostic ped breathing at the end of the procedure.5 approach. In the first place, there are draw- Rebleeding may have occurred in some ofthese backs in starting with an LP. One of these is patients. that patients with SAH may harbour an We therefore agree with Hillman that it is intracerebral haematoma, even if they are fully advisable to perform a CT scan first in all conscious, and that withdrawal of cerebro- patients who present within 72 hours of a spinal fluid (CSF) may occasionally precipitate suspected SAH, even if this requires referral to brain shift and herniation. Another disadvan- another centre.4 tage of LP is the difficulty in distinguishing It could be argued that by first performing between a traumatic tap and true subarachnoid CT the diagnosis may be delayed and that this haemorrhage. -

Intracranial Hemorrhage As Initial Presentation of Cerebral Venous Sinus Thrombosis
Case Report Journal of Heart and Stroke Published: 31 Dec, 2019 Intracranial Hemorrhage as Initial Presentation of Cerebral Venous Sinus Thrombosis Joseph Y Chu1* and Marc Ossip2 1Department of Medicine, University of Toronto, Canada 2Department of Diagnostic Imaging, William Osler Health System, Canada Abstract Intracranial Hemorrhage (ICH) as initial presentation is an uncommon complication of Cerebral Venous-Sinus Thrombosis (CVT). Clinical and neuro-imaging studies of 4 cases of ICH due cerebral venous-sinus thrombosis seen at the William Osler Health System in Toronto will be presented. Discussion of the immediate and long-term management of these interesting cases will be reviewed with emphasis on the appropriate neuro-imaging studies. Literature review of Direct Oral Anticoagulants (DOAC) in the long-term management of these challenging cases will be discussed. Introduction The following are four cases of Cerebral Venous-Sinus Thrombosis (CVT) who present initially as Intracranial Hemorrhage (ICH). Clinical details, including immediate and long term management and neuro-imaging studies are presented. Results Case 1 A 43 years old R-handed house wife, South-Asian decent, who was admitted to hospital on 06- 10-2014 with sudden headache and right hemiparesis. Her past health shows no prior hypertension or stroke. She is not on any hormone replacement therapy, non-smoker and non-drinker. Married with 1 daughter. Examination shows BP=122/80, P=70 regular, GCS=15, with right homonymous hemianopsia, right hemiparesis: arm=leg 1/5, extensor R. Plantar response. She was started on IV Heparin after her unenhanced CT showed acute left parietal intracerebral hemorrhage and her MRV showed extensive sagittal sinus thrombosis extending into the left transverse OPEN ACCESS sinus (Figures 1,2). -

Early Management of Retained Hemothorax in Blunt Head and Chest Trauma
World J Surg https://doi.org/10.1007/s00268-017-4420-x ORIGINAL SCIENTIFIC REPORT Early Management of Retained Hemothorax in Blunt Head and Chest Trauma 1,2 1,8 1,7 1 Fong-Dee Huang • Wen-Bin Yeh • Sheng-Shih Chen • Yuan-Yuarn Liu • 1 1,3,6 4,5 I-Yin Lu • Yi-Pin Chou • Tzu-Chin Wu Ó The Author(s) 2018. This article is an open access publication Abstract Background Major blunt chest injury usually leads to the development of retained hemothorax and pneumothorax, and needs further intervention. However, since blunt chest injury may be combined with blunt head injury that typically requires patient observation for 3–4 days, other critical surgical interventions may be delayed. The purpose of this study is to analyze the outcomes of head injury patients who received early, versus delayed thoracic surgeries. Materials and methods From May 2005 to February 2012, 61 patients with major blunt injuries to the chest and head were prospectively enrolled. These patients had an intracranial hemorrhage without indications of craniotomy. All the patients received video-assisted thoracoscopic surgery (VATS) due to retained hemothorax or pneumothorax. Patients were divided into two groups according to the time from trauma to operation, this being within 4 days for Group 1 and more than 4 days for Group 2. The clinical outcomes included hospital length of stay (LOS), intensive care unit (ICU) LOS, infection rates, and the time period of ventilator use and chest tube intubation. Result All demographics, including age, gender, and trauma severity between the two groups showed no statistical differences. -

Iatrogenic Spinal Subarachnoid Hematoma After Diagnostic Lumbar Puncture
https://doi.org/10.14245/kjs.2017.14.4.158 KJS Print ISSN 1738-2262 On-line ISSN 2093-6729 CASE REPORT Korean J Spine 14(4):158-161, 2017 www.e-kjs.org Iatrogenic Spinal Subarachnoid Hematoma after Diagnostic Lumbar Puncture Jung Hyun Park, Spinal subarachnoid hematoma (SSH) following diagnostic lumbar puncture is very rare. Generally, Jong Yeol Kim SSH is more likely to occur when the patient has coagulopathy or is undergoing anticoagulant therapy. Unlike the usual complications, such as headache, dizziness, and back pain at the Department of Neurosurgery, Kosin needle puncture site, SSH may result in permanent neurologic deficits if not properly treated University Gospel Hospital, Kosin within a short period of time. An otherwise healthy 43-year-old female with no predisposing University College of Medicine, factors presented with fever and headache. Diagnostic lumbar puncture was performed under Busan, Korea suspicion of acute meningitis. Lumbar magnetic resonance imaging was performed due to hypo- Corresponding Author: esthesia below the level of T10 that rapidly progressed after the lumbar puncture. SSH was Jong Yeol Kim diagnosed, and high-dose steroid therapy was started. Her neurological symptoms rapidly deterio- Department of Neurosurgery, rated after 12 hours despite the steroids, necessitating emergent decompressive laminectomy Kosin University Gospel Hospital, and hematoma removal. The patient’s condition improved after the surgery from a preoperative Kosin University College of Medicine, 262 Gamcheon-ro, Seo-gu, Busan motor score of 1/5 in the right leg and 4/5 in the left leg to brace-free ambulation (motor grade 49267, Korea 5/5) 3-month postoperative. -

Symptomatic Intracranial Hemorrhage (Sich) and Activase® (Alteplase) Treatment: Data from Pivotal Clinical Trials and Real-World Analyses
Symptomatic intracranial hemorrhage (sICH) and Activase® (alteplase) treatment: Data from pivotal clinical trials and real-world analyses Indication Activase (alteplase) is indicated for the treatment of acute ischemic stroke. Exclude intracranial hemorrhage as the primary cause of stroke signs and symptoms prior to initiation of treatment. Initiate treatment as soon as possible but within 3 hours after symptom onset. Important Safety Information Contraindications Do not administer Activase to treat acute ischemic stroke in the following situations in which the risk of bleeding is greater than the potential benefit: current intracranial hemorrhage (ICH); subarachnoid hemorrhage; active internal bleeding; recent (within 3 months) intracranial or intraspinal surgery or serious head trauma; presence of intracranial conditions that may increase the risk of bleeding (e.g., some neoplasms, arteriovenous malformations, or aneurysms); bleeding diathesis; and current severe uncontrolled hypertension. Please see select Important Safety Information throughout and the attached full Prescribing Information. Data from parts 1 and 2 of the pivotal NINDS trial NINDS was a 2-part randomized trial of Activase® (alteplase) vs placebo for the treatment of acute ischemic stroke. Part 1 (n=291) assessed changes in neurological deficits 24 hours after the onset of stroke. Part 2 (n=333) assessed if treatment with Activase resulted in clinical benefit at 3 months, defined as minimal or no disability using 4 stroke assessments.1 In part 1, median baseline NIHSS score was 14 (min: 1; max: 37) for Activase- and 14 (min: 1; max: 32) for placebo-treated patients. In part 2, median baseline NIHSS score was 14 (min: 2; max: 37) for Activase- and 15 (min: 2; max: 33) for placebo-treated patients. -

What to Expect After Having a Subarachnoid Hemorrhage (SAH) Information for Patients and Families Table of Contents
What to expect after having a subarachnoid hemorrhage (SAH) Information for patients and families Table of contents What is a subarachnoid hemorrhage (SAH)? .......................................... 3 What are the signs that I may have had an SAH? .................................. 4 How did I get this aneurysm? ..................................................................... 4 Why do aneurysms need to be treated?.................................................... 4 What is an angiogram? .................................................................................. 5 How are aneurysms repaired? ..................................................................... 6 What are common complications after having an SAH? ..................... 8 What is vasospasm? ...................................................................................... 8 What is hydrocephalus? ............................................................................... 10 What is hyponatremia? ................................................................................ 12 What happens as I begin to get better? .................................................... 13 What can I expect after I leave the hospital? .......................................... 13 How will the SAH change my health? ........................................................ 14 Will the SAH cause any long-term effects? ............................................. 14 How will my emotions be affected? .......................................................... 15 When should -
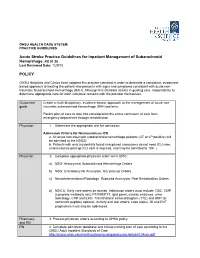
Acute Stroke Practice Guidelines for Inpatient Management of Subarachnoid Hemorrhage, PS 01.20 POLICY
OHSU HEALTH CARE SYSTEM PRACTICE GUIDELINES Acute Stroke Practice Guidelines for Inpatient Management of Subarachnoid Hemorrhage, PS 01.20 Last Reviewed Date: 1/29/10 POLICY OHSU Hospitals and Clinics have adopted this practice standard in order to delineate a consistent, evidenced- based approach to treating the patient who presents with signs and symptoms consistent with acute non- traumatic Subarachnoid Hemorrhage (SAH). Although this standard assists in guiding care, responsibility to determine appropriate care for each individual remains with the provider themselves. Outcomes/ Create a multi-disciplinary, evidence-based, approach to the management of acute non- goals traumatic subarachnoid hemorrhage (SAH) patients. Patient plan of care to take into consideration the entire continuum of care from emergency department through rehabilitation. Physician 1. Determine the appropriate unit for admission. Admission Criteria for Neurosciences ICU a. All acute non-traumatic subarachnoid hemorrhage patients (CT or LP positive) will be admitted to the NSICU. b. Patients with only incidentally found unruptured aneurysms do not need ICU care, unless routine post-op ICU care is required, and may be admitted to 10K. ( Physician 2. Complete appropriate physician order set in EPIC: a) NSG: Aneurysmal Subarachnoid Hemorrhage Orders. b) NSG: Craniotomy for Aneurysm: ICU post-op Orders. c) NeuroInterventional Radiology: Ruptured Aneurysm: Post Embolization Orders. d) NSICU: Daily care orders on rounds. Admission orders must include: CBC, CMP (complete metabolic set), PT/INR/PTT, lipid panel, cardiac enzymes, urine toxicology, CXR and EKG. Transthoracic echocardiogram (TTE) and BNP (B- natriuretic peptide) optional. Activity and diet orders, code status, GI and DVT prophylaxis must also be addressed. -

Of These, About 62% Are Women. STROKE: an OVERV
STROKE: AN OVERVIEW It is estimated that more than 700,000 Americans suffer a cerebrovascular event, or stroke, each year. Approximately 500,000 of these are first strokes, and 200,000 are recurrent attacks. On average, someone suffers a stroke every 45 seconds, and a stroke death occurs every 3.1 minutes (1). According to American Heart Association data, approximately 4,700,000 stroke survivors are alive in the United States today (2). Stroke is the leading In West Virginia, between 1,200 and cause of adult disability in the United States and the 1,300 people die from stroke each year; third leading cause of death nationwide. In West of these, about 62% are women. Virginia, stroke ranks as the fourth leading cause of death, after heart disease, cancer, and chronic lower respiratory disease; between 1,200 and 1,300 people die from stroke each year in the state. Death rates from stroke declined markedly in the 1970s and 1980s in both the state and the country as a whole; however, this decline leveled off in the 1990s (3). Figure 1 illustrates the latter part of this trend, showing 20 years of stroke mortality rates in West Virginia among men and women. Rates among both men and women decreased in the state rather consistently until 1992, after which slight increases occurred. -1- Even though the mortality rate for stroke declined 12.3% from 1990 to 2000 in the United States, the actual number of stroke deaths rose nearly 10% (2) and stroke-related hospitalizations increased 19% (4). National projections for stroke mortality are bleak. -

Simultaneous Cranial Subarachnoid Hemorrhage-Subdural Hematoma
Case Report/Olgu Sunumu İstanbul Med J 2021; 22(1): 81-3 DO I: 10.4274/imj.galenos.2020.73658 Simultaneous Cranial Subarachnoid Hemorrhage-Subdural Hematoma and Spinal Subarachnoid Hemorrhage Eşzamanlı Kraniyal Subaraknoid Kanama-Subdural Hematom ve Spinal Subaraknoid Kanama Hatice Kaplanoğlu1, Veysel Kaplanoğlu2, Aynur Turan1, Onur Karacif1 1University of Health Sciences Turkey, Dışkapı Yıldırım Beyazıt Training and Research Hospital, Clinic of Radiology, Ankara, Turkey 2University of Health Sciences Turkey, Keçiören Training and Research Hospital, Clinic of Radiology, Ankara, Turkey ABSTRACT ÖZ Patients with traumatic intracranial subarachnoid hemorrhage Çok nadiren, travmatik intrakraniyal subaraknoid hemorojisi (SAH) rarely develop spinal subarachnoid hemorrhage (SSAH) (SAH) olan hastalarda, doğrudan omurga yaralanması olmadan without direct spinal injury. We present the case of a 76-year- spinal subaraknoid kanama (SSAH) ortaya çıkabilir. Travmatik old male patient with traumatic intracranial SAH and subdural intrakraniyal SAH ve subdural hematomu olan 76 yaşındaki hematoma, back pain and weakness in the both lower erkek hastada, yoğun bakım takibi sırasında travmadan üç gün limbs radiating to the legs three days after the trauma. After sonra bacaklarına yayılan sırt ağrısı ve bilateral alt ekstremitede worsening of pain and numbness, the patient underwent a güçsüzlük ortaya çıktı. Ağrı ve uyuşmanın kötüleşmesi üzerine, lumbar magnetic resonance imaging 7 days after the trauma, travmadan 7 gün sonra hastaya lomber manyetik rezonans in which blood was seen in the spinal canal in the lumbosacral görüntüleme yapıldı. Lumbosakral bölgede intraspinal region. The bleeding was considered SSAH because of the kanama görüldü. Kanamanın sıvı seviyesi göstermesi liquid level. The patient underwent conservative treatment sebebiyle SSAH olarak değerlendirildi. Hasta kardiyak açıdan because the patient was found to be at high cardiac risk and yüksek riskli bulunduğu için ve nörolojik defisiti hafif olduğu the neurological deficit was mild.