Types of Brain Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Management of the Head Injury Patient
Management of the Head Injury Patient William Schecter, MD Epidemilogy • 1.6 million head injury patients in the U.S. annually • 250,000 head injury hospital admissions annually • 60,000 deaths • 70-90,000 permanent disability • Estimated cost: $100 billion per year Causes of Brain Injury • Motor Vehicle Accidents • Falls • Anoxic Encephalopathy • Penetrating Trauma • Air Embolus after blast injury • Ischemia • Intracerebral hemorrhage from Htn/aneurysm • Infection • tumor Brain Injury • Primary Brain Injury • Secondary Brain Injury Primary Brain Injury • Focal Brain Injury – Skull Fracture – Epidural Hematoma – Subdural Hematoma – Subarachnoid Hemorrhage – Intracerebral Hematorma – Cerebral Contusion • Diffuse Axonal Injury Fracture at the Base of the Skull Battle’s Sign • Periorbital Hematoma • Battle’s Sign • CSF Rhinorhea • CSF Otorrhea • Hemotympanum • Possible cranial nerve palsy http://health.allrefer.com/pictures-images/ Fracture of maxillary sinus causing CSF Rhinorrhea battles-sign-behind-the-ear.html Skull Fractures Non-depressed vs Depressed Open vs Closed Linear vs Egg Shell Linear and Depressed Normal Depressed http://www.emedicine.com/med/topic2894.htm Temporal Bone Fracture http://www.vh.org/adult/provider/anatomy/ http://www.bartleby.com/107/illus510.html AnatomicVariants/Cardiovascular/Images0300/0386.html Epidural Hematoma http://www.chestjournal.org/cgi/content/full/122/2/699 http://www.bartleby.com/107/illus769.html Epidural Hematoma • Uncommon (<1% of all head injuries, 10% of post traumatic coma patients) • Located -

Hypertensive Intracerebral Hemorrhage Due to Autonomic Dysreflexia in a Young Man with Cervical Cord Injury
J UOEH(産業医科大学雑誌)35( 2 ): 159-164(2013) 159 [Case Report] Hypertensive Intracerebral Hemorrhage Due to Autonomic Dysreflexia in a Young Man with Cervical Cord Injury Tadashi Sumiya Department of Spinal Care Center, Division of Rehabilitation Medicine 219 Myoji, Katsuragi-cho, Ito-gun, 649-7113, Japan Abstract : The author reports the case of a 36 year old man with cervical cord injury in whom autonomic dysreflexia developed into intracerebral hemorrhage during inpatient rehabilitation. This patient showed complete quadriplegia (motor below C6 and sensory below C7) due to fracture of the 6th cervical vertebra. An indwelling urethral catheter had been inserted into the bladder for 3 months, diminishing bladder expansiveness. Bladder capacity decreased to 200 ml and the patient frequently experienced headaches whenever his bladder was full. To obtain smoother urine flow, a supra-pubic cystostomy was performed. The headaches were temporarily cured, but soon relapsed with extreme increases in blood pressure, representing typical symptoms of autonomic dysreflexia. However, no poten- tial triggers were identified or removed, and lack of blood pressure management led to left putaminal hemorrhage. Despite operative treatment, the right upper extremity showed progressive increases in muscle tonus and finally formed a frozen shoulder with elbow flexion contracture. Two factors contributed to this serious complication: first, autonomic dysreflexia triggered by minor malfunction and/or irritation from the cystostomy catheter; and second, the medical staff lacked sufficient experience in and knowledge about the management of autonomic dysreflexia. It is of the utmost importance for medical staff engaging in rehabilitation of spinal patients to share information regard- ing triggers of autonomic dysreflexia and to be thorough in ensuring proper medical management. -

Intracerebral Hemorrhage ICH Fact Sheet
FACT SHEET FOR PATIENTS AND FAMILIES Intracerebral Hemorrhage (ICH) What is it? An intracerebral [in-truh-suh-REE-bruh l] hemorrhage [HEM-rij], Dura mater or ICH, is bleeding inside or around the brain, which Brain Skull can put pressure on the brain. An ICH robs the brain Intracerebral of oxygen, so it must be identified and managed right hemorrhage away. Other names for ICH are cerebral hemorrhage or intracranial [in-truh-KREY-nee-uh l] hemorrhage. ICH can happen because of trauma or as a result of no known cause (spontaneous ICH), which is a type of stroke called a hemorrhagic [hem-oh-RAJ-ik] stroke. In the U.S. each year, about 1 in 10 people who have strokes do so because of an ICH. Stroke is the leading cause of disability and the 5th-leading cause of death in the U.S. What are the symptoms of spontaneous ICH? Spontaneous ICH symptoms usually develop suddenly, without warning. Key symptoms can include a SUDDEN (see BE FAST on page 2): What causes it? • Loss of balance or coordination An ICH is often caused by a blood vessel leaking or • Change in vision breaking. This can be the result of: • Weakness of the face, arm, or leg • High blood pressure that has damaged a blood vessel • Difficulty speaking • Smoking, overuse of alcohol, or use of illegal drugs Other ICH symptoms can include: such as cocaine or methamphetamine • Severe headache with no known cause (patients • Diabetes often describe it as “the worst headache of my life”) • Abnormal blood vessel proteins in the elderly • Seizures An ICH can also be caused by: • Vomiting or severe nausea, when combined with • Anticoagulant therapy (treatment with blood thinners) other symptoms from this list • Problems with vein structure • Partial or total loss of conciousness • A brain tumor that bleeds • Head injuries caused by a fall or accident 1 How is it diagnosed? What can I expect afterward? Your doctor will explain what tests will be used to Your long-term outlook depends on the location and diagnose ICH, depending on your condition. -

The Diagnosis of Subarachnoid Haemorrhage
Journal ofNeurology, Neurosurgery, and Psychiatry 1990;53:365-372 365 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.53.5.365 on 1 May 1990. Downloaded from OCCASIONAL REVIEW The diagnosis of subarachnoid haemorrhage M Vermeulen, J van Gijn Lumbar puncture (LP) has for a long time been of 55 patients with SAH who had LP, before the mainstay of diagnosis in patients who CT scanning and within 12 hours of the bleed. presented with symptoms or signs of subarach- Intracranial haematomas with brain shift was noid haemorrhage (SAH). At present, com- proven by operation or subsequent CT scan- puted tomography (CT) has replaced LP for ning in six of the seven patients, and it was this indication. In this review we shall outline suspected in the remaining patient who stop- the reasons for this change in diagnostic ped breathing at the end of the procedure.5 approach. In the first place, there are draw- Rebleeding may have occurred in some ofthese backs in starting with an LP. One of these is patients. that patients with SAH may harbour an We therefore agree with Hillman that it is intracerebral haematoma, even if they are fully advisable to perform a CT scan first in all conscious, and that withdrawal of cerebro- patients who present within 72 hours of a spinal fluid (CSF) may occasionally precipitate suspected SAH, even if this requires referral to brain shift and herniation. Another disadvan- another centre.4 tage of LP is the difficulty in distinguishing It could be argued that by first performing between a traumatic tap and true subarachnoid CT the diagnosis may be delayed and that this haemorrhage. -

Iatrogenic Spinal Subarachnoid Hematoma After Diagnostic Lumbar Puncture
https://doi.org/10.14245/kjs.2017.14.4.158 KJS Print ISSN 1738-2262 On-line ISSN 2093-6729 CASE REPORT Korean J Spine 14(4):158-161, 2017 www.e-kjs.org Iatrogenic Spinal Subarachnoid Hematoma after Diagnostic Lumbar Puncture Jung Hyun Park, Spinal subarachnoid hematoma (SSH) following diagnostic lumbar puncture is very rare. Generally, Jong Yeol Kim SSH is more likely to occur when the patient has coagulopathy or is undergoing anticoagulant therapy. Unlike the usual complications, such as headache, dizziness, and back pain at the Department of Neurosurgery, Kosin needle puncture site, SSH may result in permanent neurologic deficits if not properly treated University Gospel Hospital, Kosin within a short period of time. An otherwise healthy 43-year-old female with no predisposing University College of Medicine, factors presented with fever and headache. Diagnostic lumbar puncture was performed under Busan, Korea suspicion of acute meningitis. Lumbar magnetic resonance imaging was performed due to hypo- Corresponding Author: esthesia below the level of T10 that rapidly progressed after the lumbar puncture. SSH was Jong Yeol Kim diagnosed, and high-dose steroid therapy was started. Her neurological symptoms rapidly deterio- Department of Neurosurgery, rated after 12 hours despite the steroids, necessitating emergent decompressive laminectomy Kosin University Gospel Hospital, and hematoma removal. The patient’s condition improved after the surgery from a preoperative Kosin University College of Medicine, 262 Gamcheon-ro, Seo-gu, Busan motor score of 1/5 in the right leg and 4/5 in the left leg to brace-free ambulation (motor grade 49267, Korea 5/5) 3-month postoperative. -

What to Expect After Having a Subarachnoid Hemorrhage (SAH) Information for Patients and Families Table of Contents
What to expect after having a subarachnoid hemorrhage (SAH) Information for patients and families Table of contents What is a subarachnoid hemorrhage (SAH)? .......................................... 3 What are the signs that I may have had an SAH? .................................. 4 How did I get this aneurysm? ..................................................................... 4 Why do aneurysms need to be treated?.................................................... 4 What is an angiogram? .................................................................................. 5 How are aneurysms repaired? ..................................................................... 6 What are common complications after having an SAH? ..................... 8 What is vasospasm? ...................................................................................... 8 What is hydrocephalus? ............................................................................... 10 What is hyponatremia? ................................................................................ 12 What happens as I begin to get better? .................................................... 13 What can I expect after I leave the hospital? .......................................... 13 How will the SAH change my health? ........................................................ 14 Will the SAH cause any long-term effects? ............................................. 14 How will my emotions be affected? .......................................................... 15 When should -
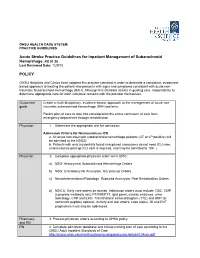
Acute Stroke Practice Guidelines for Inpatient Management of Subarachnoid Hemorrhage, PS 01.20 POLICY
OHSU HEALTH CARE SYSTEM PRACTICE GUIDELINES Acute Stroke Practice Guidelines for Inpatient Management of Subarachnoid Hemorrhage, PS 01.20 Last Reviewed Date: 1/29/10 POLICY OHSU Hospitals and Clinics have adopted this practice standard in order to delineate a consistent, evidenced- based approach to treating the patient who presents with signs and symptoms consistent with acute non- traumatic Subarachnoid Hemorrhage (SAH). Although this standard assists in guiding care, responsibility to determine appropriate care for each individual remains with the provider themselves. Outcomes/ Create a multi-disciplinary, evidence-based, approach to the management of acute non- goals traumatic subarachnoid hemorrhage (SAH) patients. Patient plan of care to take into consideration the entire continuum of care from emergency department through rehabilitation. Physician 1. Determine the appropriate unit for admission. Admission Criteria for Neurosciences ICU a. All acute non-traumatic subarachnoid hemorrhage patients (CT or LP positive) will be admitted to the NSICU. b. Patients with only incidentally found unruptured aneurysms do not need ICU care, unless routine post-op ICU care is required, and may be admitted to 10K. ( Physician 2. Complete appropriate physician order set in EPIC: a) NSG: Aneurysmal Subarachnoid Hemorrhage Orders. b) NSG: Craniotomy for Aneurysm: ICU post-op Orders. c) NeuroInterventional Radiology: Ruptured Aneurysm: Post Embolization Orders. d) NSICU: Daily care orders on rounds. Admission orders must include: CBC, CMP (complete metabolic set), PT/INR/PTT, lipid panel, cardiac enzymes, urine toxicology, CXR and EKG. Transthoracic echocardiogram (TTE) and BNP (B- natriuretic peptide) optional. Activity and diet orders, code status, GI and DVT prophylaxis must also be addressed. -

NIH Public Access Author Manuscript J Neuropathol Exp Neurol
NIH Public Access Author Manuscript J Neuropathol Exp Neurol. Author manuscript; available in PMC 2010 September 24. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: J Neuropathol Exp Neurol. 2009 July ; 68(7): 709±735. doi:10.1097/NEN.0b013e3181a9d503. Chronic Traumatic Encephalopathy in Athletes: Progressive Tauopathy following Repetitive Head Injury Ann C. McKee, MD1,2,3,4, Robert C. Cantu, MD3,5,6,7, Christopher J. Nowinski, AB3,5, E. Tessa Hedley-Whyte, MD8, Brandon E. Gavett, PhD1, Andrew E. Budson, MD1,4, Veronica E. Santini, MD1, Hyo-Soon Lee, MD1, Caroline A. Kubilus1,3, and Robert A. Stern, PhD1,3 1 Department of Neurology, Boston University School of Medicine, Boston, Massachusetts 2 Department of Pathology, Boston University School of Medicine, Boston, Massachusetts 3 Center for the Study of Traumatic Encephalopathy, Boston University School of Medicine, Boston, Massachusetts 4 Geriatric Research Education Clinical Center, Bedford Veterans Administration Medical Center, Bedford, Massachusetts 5 Sports Legacy Institute, Waltham, MA 6 Department of Neurosurgery, Boston University School of Medicine, Boston, Massachusetts 7 Department of Neurosurgery, Emerson Hospital, Concord, MA 8 CS Kubik Laboratory for Neuropathology, Department of Pathology, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts Abstract Since the 1920s, it has been known that the repetitive brain trauma associated with boxing may produce a progressive neurological deterioration, originally termed “dementia pugilistica” and more recently, chronic traumatic encephalopathy (CTE). We review the 47 cases of neuropathologically verified CTE recorded in the literature and document the detailed findings of CTE in 3 professional athletes: one football player and 2 boxers. -

Of These, About 62% Are Women. STROKE: an OVERV
STROKE: AN OVERVIEW It is estimated that more than 700,000 Americans suffer a cerebrovascular event, or stroke, each year. Approximately 500,000 of these are first strokes, and 200,000 are recurrent attacks. On average, someone suffers a stroke every 45 seconds, and a stroke death occurs every 3.1 minutes (1). According to American Heart Association data, approximately 4,700,000 stroke survivors are alive in the United States today (2). Stroke is the leading In West Virginia, between 1,200 and cause of adult disability in the United States and the 1,300 people die from stroke each year; third leading cause of death nationwide. In West of these, about 62% are women. Virginia, stroke ranks as the fourth leading cause of death, after heart disease, cancer, and chronic lower respiratory disease; between 1,200 and 1,300 people die from stroke each year in the state. Death rates from stroke declined markedly in the 1970s and 1980s in both the state and the country as a whole; however, this decline leveled off in the 1990s (3). Figure 1 illustrates the latter part of this trend, showing 20 years of stroke mortality rates in West Virginia among men and women. Rates among both men and women decreased in the state rather consistently until 1992, after which slight increases occurred. -1- Even though the mortality rate for stroke declined 12.3% from 1990 to 2000 in the United States, the actual number of stroke deaths rose nearly 10% (2) and stroke-related hospitalizations increased 19% (4). National projections for stroke mortality are bleak. -

Simultaneous Cranial Subarachnoid Hemorrhage-Subdural Hematoma
Case Report/Olgu Sunumu İstanbul Med J 2021; 22(1): 81-3 DO I: 10.4274/imj.galenos.2020.73658 Simultaneous Cranial Subarachnoid Hemorrhage-Subdural Hematoma and Spinal Subarachnoid Hemorrhage Eşzamanlı Kraniyal Subaraknoid Kanama-Subdural Hematom ve Spinal Subaraknoid Kanama Hatice Kaplanoğlu1, Veysel Kaplanoğlu2, Aynur Turan1, Onur Karacif1 1University of Health Sciences Turkey, Dışkapı Yıldırım Beyazıt Training and Research Hospital, Clinic of Radiology, Ankara, Turkey 2University of Health Sciences Turkey, Keçiören Training and Research Hospital, Clinic of Radiology, Ankara, Turkey ABSTRACT ÖZ Patients with traumatic intracranial subarachnoid hemorrhage Çok nadiren, travmatik intrakraniyal subaraknoid hemorojisi (SAH) rarely develop spinal subarachnoid hemorrhage (SSAH) (SAH) olan hastalarda, doğrudan omurga yaralanması olmadan without direct spinal injury. We present the case of a 76-year- spinal subaraknoid kanama (SSAH) ortaya çıkabilir. Travmatik old male patient with traumatic intracranial SAH and subdural intrakraniyal SAH ve subdural hematomu olan 76 yaşındaki hematoma, back pain and weakness in the both lower erkek hastada, yoğun bakım takibi sırasında travmadan üç gün limbs radiating to the legs three days after the trauma. After sonra bacaklarına yayılan sırt ağrısı ve bilateral alt ekstremitede worsening of pain and numbness, the patient underwent a güçsüzlük ortaya çıktı. Ağrı ve uyuşmanın kötüleşmesi üzerine, lumbar magnetic resonance imaging 7 days after the trauma, travmadan 7 gün sonra hastaya lomber manyetik rezonans in which blood was seen in the spinal canal in the lumbosacral görüntüleme yapıldı. Lumbosakral bölgede intraspinal region. The bleeding was considered SSAH because of the kanama görüldü. Kanamanın sıvı seviyesi göstermesi liquid level. The patient underwent conservative treatment sebebiyle SSAH olarak değerlendirildi. Hasta kardiyak açıdan because the patient was found to be at high cardiac risk and yüksek riskli bulunduğu için ve nörolojik defisiti hafif olduğu the neurological deficit was mild. -

Canadian Stroke Best Practice Recommendations
CANADIAN STROKE BEST PRACTICE RECOMMENDATIONS MANAGEMENT OF SPONTANEOUS INTRACEREBRAL HEMORRHAGE Seventh Edition - New Module 2020 Ashkan Shoamanesh (Co-chair), M. Patrice Lindsay, Lana A Castellucci, Anne Cayley, Mark Crowther, Kerstin de Wit, Shane W English, Sharon Hoosein, Thien Huynh, Michael Kelly, Cian J O’Kelly, Jeanne Teitelbaum, Samuel Yip, Dar Dowlatshahi, Eric E Smith, Norine Foley, Aleksandra Pikula, Anita Mountain, Gord Gubitz and Laura C. Gioia(Co-chair), on behalf of the Canadian Stroke Best Practices Advisory Committee in collaboration with the Canadian Stroke Consortium and the Canadian Hemorrhagic Stroke Trials Initiative Network (CoHESIVE). © 2020 Heart & Stroke October 2020 Heart and Stroke Foundation Management of Spontaneous Intracerebral Hemorrhage Canadian Stroke Best Practice Recommendations Table of Contents CANADIAN STROKE BEST PRACTICE RECOMMENDATIONS MANAGEMENT OF SPONTANEOUS INTRACERBRAL HEMORRHAGE SEVENTH EDITION, 2020 Table of Contents Topic Page Part One: Canadian Stroke Best Practice Recommendations Introduction and Overview I. Introduction 3 II. Spontaneous Intracerebral Hemorrhage Module Overview 3 III. Spontaneous Intracerebral Hemorrhage Definitions 4 IV. Guideline Development Methodology 4 V. Acknowledgements, Funding, Citation 6 VI. Figure One: Intracerebral Hemorrhage Patient Flow Map 8 Part Two: Canadian Stroke Best Practice Recommendations Spontaneous Intracerebral Hemorrhage 1. Emergency Management of Intracerebral Hemorrhage 9 1.1 Initial Clinical Assessment of Intracerebral Hemorrhage 9 1.2 Blood Pressure Management 10 1.3 Management of Anticoagulation 11 1.4 Consultation with Neurosurgery 12 1.5 Neuroimaging 12 1.5.1 Recommended additional urgent neuroimaging to confirm ICH diagnosis 12 1.5.2 Recommended additional etiological neuroimaging 13 1.6 Surgical management of Intracerebral Hemorrhage 13 Box One: Symptoms of Intracerebral Hemorrhage: 15 Box Two: Modified Boston Criteria (Linn 2010) 16 2. -

Subarachnoid Hemorrhage (SAH) (A Type of Hemorrhagic Stroke)
Subarachnoid Hemorrhage (SAH) (A type of Hemorrhagic Stroke) A Guide for Patients and Families in the Neurosurgery Intensive Care Unit Department of Neurosurgery Introduction A team of doctors and nurses at The University of Michigan Neurosurgery Intensive Care Unit (Neuro ICU) wrote this booklet for patients who have had a Subarachnoid Hemorrhage (SAH) and for the family members and friends who care about them. The purpose of this booklet is to give answers to questions about the illness and treatment of SAH and about what you can expect during your stay in the Neuro ICU. If you have any additional questions, please ask a Neurosurgery team member. Table of Contents: What is SAH?............................................................................4 What causes SAH?....................................................4 What are the risk factors for SAH?......................5 Treating SAH at the University of Michigan...................6 Reducing possible side-effects………………….8 Preventing a secondary stroke from cerebral vasospasm………………………………………… 8 What you need to know about your hospital stay…..10 How long will it last?.............................................10 The dangers of being bed bound.......................10 How can family and friends help patients achieve the best outcomes?...............................................................10 Your partnership with the Neuro ICU team................ 12 What is the best way to keep informed about a patient’s clinical status?........................................................12