Chronic Invasive Rhinosinusitis by Conidiobolus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Epidemiological, Clinical and Diagnostic Aspects of Sheep Conidiobolomycosis in Brazil
Ciência Rural, Santa Maria,Epidemiological, v.46, n.5, p.839-846, clinical mai, and 2016 diagnostic aspects of sheep conidiobolomycosis http://dx.doi.org/10.1590/0103-8478cr20150935 in Brazil. 839 ISSN 1678-4596 MICROBIOLOGY Epidemiological, clinical and diagnostic aspects of sheep conidiobolomycosis in Brazil Aspectos epidemiológicos, clínicos e de diagnóstico da conidiobolomicose ovina no Brasil Carla WeiblenI Daniela Isabel Brayer PereiraII Valéria DutraIII Isabela de GodoyIII Luciano NakazatoIII Luís Antonio SangioniI Janio Morais SanturioIV Sônia de Avila BottonI* — REVIEW — ABSTRACT As lesões da conidiobolomicose normalmente são de caráter granulomatoso e necrótico, apresentando-se sob duas formas Conidiobolomycosis is an emerging disease caused clínicas: rinofacial e nasofaríngea. O presente artigo tem como by fungi of the cosmopolitan genus Conidiobolus. Particular objetivo revisar as principais características da doença em ovinos, strains of Conidiobolus coronatus, Conidiobolus incongruus and particularizando a epidemiologia, assim como os aspectos clínicos Conidiobolus lamprauges, mainly from tropical or sub-tropical e o diagnóstico das infecções causadas por Conidiobolus spp. no origin, cause the mycosis in humans and animals, domestic or Brasil. Neste País, a enfermidade é endêmica nas regiões nordeste wild. Lesions are usually granulomatous and necrotic in character, e centro-oeste, afetando ovinos predominantemente de raças presenting two clinical forms: rhinofacial and nasopharyngeal. deslanadas, ocasionando a morte na grande maioria dos casos This review includes the main features of the disease in sheep, with estudados. As espécies do fungo responsáveis pelas infecções an emphasis on the epidemiology, clinical aspects, and diagnosis em ovinos são C. coronatus e C. lamprauges e a forma clínica of infections caused by Conidiobolus spp. -

A New Species of <I>Conidiobolus</I> (<I>Ancylistaceae</I>) from Anhui, China
ISSN (print) 0093-4666 © 2012. Mycotaxon, Ltd. ISSN (online) 2154-8889 MYCOTAXON http://dx.doi.org/10.5248/120.427 Volume 120, pp. 427–435 April–June 2012 A new species of Conidiobolus (Ancylistaceae) from Anhui, China Yong Nie1, Cui-Zhu Yu1, Xiao-Yong Liu2* & Bo Huang1* 1Anhui Provincial Key Laboratory of Microbial Control, Anhui Agricultural University, West Changjiang Road 130, Hefei, Anhui 230036, China 2State Key Laboratory of Mycology, Institute of Microbiology, Chinese Academy of Sciences, Beijing 100101, China * Correspondence to: [email protected], [email protected] Abstract —Conidiobolus sinensis was isolated from plant detritus in Huoshan, Anhui Province, eastern China. It produces primary conidiophores from cushion mycelium, which is distinct from all other species in the genus except C. stromoideus and C. lichenicola. Morphologically C. sinensis differs from C. stromoideus in the shape of the mycelia at the colony edge and conidiophore length and from C. lichenicola by colony color and mycelial form. A phylogram based on partial 28S rDNA and EF-1α sequences from 14 Conidiobolus species shows C. sinensis most closely related to C. stromoideus, forming a clade of sister taxa with a 100% bootstrap. DNA similarity levels between these two species were 94% (28S rDNA) and 96% (EF-1α). Based on the morphological and molecular evidence, C. sinensis is considered a new species. Key words —Entomophthorales, hyphal knots, taxonomy Introduction Species belonging to Conidiobolus can be easily isolated from soil, decaying leaf litter, rotten vegetables and some dead insects, although the type of the genus, C. utriculosus Bref., was first isolated from the decaying fleshy fruitbodies of Exidia and Hirneola. -
Human and Microbial Proteins from Corpora Amylacea of Alzheimer's
www.nature.com/scientificreports OPEN Human and Microbial Proteins From Corpora Amylacea of Alzheimer’s Disease Received: 24 November 2017 Diana Pisa1, Ruth Alonso1, Ana Isabel Marina1, Alberto Rábano2 & Luis Carrasco1 Accepted: 14 June 2018 Corpora amylacea (CA) are spherical bodies mainly composed of polyglucans and, to a lesser extent, Published: xx xx xxxx proteins. They are abundant in brains from patients with neurodegenerative diseases, particularly Alzheimer’s disease. Although CA were discovered many years ago, their precise origin and function remain obscure. CA from the insular cortex of two Alzheimer’s patients were purifed and the protein composition was assessed by proteomic analysis. A number of microbial proteins were identifed and fungal DNA was detected by nested PCR.A wide variety of human proteins form part of CA. In addition, we unequivocally demonstrated several fungal and bacterial proteins in purifed CA. In addition to a variety of human proteins, CA also contain fungal and bacterial polypeptides.In conclusion, this paper suggests that the function of CA is to scavenge cellular debris provoked by microbial infections. Several diferent types of polyglucan bodies have been found in the central nervous system (CNS) of elderly peo- ple, as well as in patients with a variety of pathologies, including Alzheimer’s disease (AD), epilepsy, amyotrophic lateral sclerosis (ALS), multiple sclerosis (MS) and hippocampal sclerosis1,2. Among these polyglucan structures, Lafora bodies, Bielschowsky bodies and corpora amylacea (CA) have been identifed based on their morphological characteristics3–5. Although CA were described early in the 18th century, their precise origin and potential function in normal or pathological conditions remains an enigma. -

1 Naming Names: the Etymology of Fungal Entomopathogens
Research Signpost 37/661 (2), Fort P.O., Trivandrum-695 023, Kerala, India Use of Entomopathogenic Fungi in Biological Pest Management, 2007: 1-11 ISBN: 978-81-308-0192-6 Editors: Sunday Ekesi and Nguya K. Maniania Naming names: The etymology 1 of fungal entomopathogens Fernando E. Vega Sustainable Perennial Crops Laboratory, USDA, ARS, Bldg. 011A, BARC-W Beltsville Maryland 20705, USA Abstract This chapter introduces the reader to the etymology of the generic names given to 26 fungal entomopathogens. Possessing some knowledge on how a name originates sometimes provides us with information on a fungal characteristic that might help us identify the organism, e.g., Conidiobolus, Cordyceps, Pandora, Regiocrella, Orthomyces, etc. In other cases, the name won’t tell us what the fungus looks like, but serves to honor those for whom the fungus was named, e.g., Aschersonia, Batkoa, Beauveria, Nomuraea, Strongwellsea, etc. Correspondence/Reprint request: Dr. Fernando E. Vega, Sustainable Perennial Crops Laboratory, USDA ARS, Bldg. 011A, BARC-W, Beltsville, Maryland 20705, USA. E-mail: [email protected] 2 Fernando E. Vega 1. Introduction One interesting aspect in the business of science is the naming of taxonomic species: the reasons why organisms are baptized with a certain name, which might or might not change as science progresses. Related to this topic, the scientific illustrator Louis C. C. Krieger (1873-1940) [1] self-published an eight- page long article in 1924, entitled “The millennium of systematic mycology: a phantasy” where the main character is a “... systematic mycologist, who, from too much “digging” in the mighty “scrapheap” of synonymy, fell into a deep coma.” As he lies in this state, he dreams about being in Heaven, and unable to leave behind his collecting habits, picks up an amanita and upon examining it finds a small capsule hidden within it. -
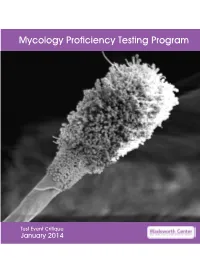
Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2014 Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 13 Mold Descriptions 14 M-1 Stachybotrys chartarum 14 M-2 Aspergillus clavatus 18 M-3 Microsporum gypseum 22 M-4 Scopulariopsis species 26 M-5 Sporothrix schenckii species complex 30 Yeast Descriptions 34 Y-1 Cryptococcus uniguttulatus 34 Y-2 Saccharomyces cerevisiae 37 Y-3 Candida dubliniensis 40 Y-4 Candida lipolytica 43 Y-5 Cryptococcus laurentii 46 Direct Detection - Cryptococcal Antigen 49 Antifungal Susceptibility Testing - Yeast 52 Antifungal Susceptibility Testing - Mold (Educational) 54 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally. -

Jamaica UHSM ¤ 1,2* University Hospital Harish Gugnani , David W Denning of South Manchester NHS Foundation Trust ¤Professor of Microbiology & Epidemiology, St
Burden of serious fungal infections in Jamaica UHSM ¤ 1,2* University Hospital Harish Gugnani , David W Denning of South Manchester NHS Foundation Trust ¤Professor of Microbiology & Epidemiology, St. James School of Medicine, Kralendjik, Bonaire (Dutch Caribbean). 1 LEADING WI The University of Manchester, Manchester Academic Health Science Centre, Manchester, U.K. INTERNATIONAL 2 FUNGAL The University Hospital of South Manchester, (*Corresponding Author) National Aspergillosis Centre (NAC) Manchester, U.K. EDUCATION Background and Rationale The incidence and prevalence of fungal infections in Jamaica is unknown. The first human case of Conidiobolus coronatus infection was discovered in Jamaica (Bras et al. 1965). Cases of histoplasmosis and eumycetoma are reported (Fincharn & DeCeulaer 1980, Nicholson et al., 2004; Fletcher et al, 2001). Tinea capitis is very frequent in children Chronic pulmonary (East-Innis et al., 2006), because of the population being aspergillosis with aspergilloma (in the left upper lobe) in a 53- predominantly of African ancestry. In a one year study of 665 HIV yr-old, HIV-negative Jamaican male, developing after one infected patients, 46% of whom had CD4 cell counts <200/uL, 23 had year of antitubercular treatment; his baseline IgG pneumocystis pneumonia and 3 had cryptococcal meningitis (Barrow titer was 741 mg/L (0-40). As a smoker, he also had moderate et al. 2010). We estimated the burden of fungal infections in Jamaica emphysema. from published literature and modelling. Table 1. Estimated burden of fungal disease in Jamaica Fungal None HIV Respiratory Cancer ICU Total Rate Methods condition /AIDS /Tx burden 100k We also extracted data from published papers on epidemiology and Oesophageal ? 2,100 - ? - 2,100 77 from the WHO STOP TB program and UNAIDS. -

A Morphological and Molecular Survey of Neoconidiobolus Reveals a New Species and Two New Combinations
A morphological and molecular survey of Neoconidiobolus reveals a new species and two new combinations Yong Nie Anhui University of Technology Zi-Min Wang Anhui University of Technology Xiao-Yong Liu Chinese Academy of Sciences Bo Huang ( [email protected] ) Anhui Agricultural University Research Article Keywords: Ancylistaceae, Morphology, Taxonomy, Molecular Phylogeny Posted Date: June 1st, 2021 DOI: https://doi.org/10.21203/rs.3.rs-186207/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/16 Abstract The genus Neoconidiobolus was recently established to accommodate all members of the Conidiobolus subgenus Conidiobolus. Based on mitochondrial small subunit (mtSSU), nuclear large subunit (nucLSU) of rDNA and translation elongation factor 1-alpha (TEF1), this study further resolved the genus Neoconidiobolus into three clades, with three new taxa being added. They are N. kunyushanensis B. Huang & Y. Nie, sp. nov., N. lamprauges (Drechsler) B. Huang & Y. Nie, comb. nov., and N. nanodes (Drechsler) B. Huang & Y. Nie, comb. nov. Meanwhile, a morphologial comparison among species in the three clades and a key to the species of the genus Neoconidiobolus are provided herein. Introduction Conidiobolus Brefeld (Ancylistaceae, Entomophthorales) was erected by Brefeld (1884). It is a large and worldwide distributed group containing 80 records in the Index Fungorum database (http://www.indexfungorum.org/). Most members of Conidiobolus occur saprophytically in soil and on decaying leaves, and few have been noted as pathogens of insects, animals and humans (Vilela et al. 2010; Gryganskyi et al. 2012; Mendoza et al. 2014). During 1950s–1960s, almost all the 40 Conidiobolus species have been reported in the North America and South Asia (Drechsler 1952; Srinivasan and Thirumalachar 1961; Nie et al. -

Fungal Infections
FUNGAL INFECTIONS SUPERFICIAL MYCOSES DEEP MYCOSES MIXED MYCOSES • Subcutaneous mycoses : important infections • Mycologists and clinicians • Common tropical subcutaneous mycoses • Signs, symptoms, diagnostic methods, therapy • Identify the causative agent • Adequate treatment Clinical classification of Mycoses CUTANEOUS SUBCUTANEOUS OPPORTUNISTIC SYSTEMIC Superficial Chromoblastomycosis Aspergillosis Aspergillosis mycoses Sporotrichosis Candidosis Blastomycosis Tinea Mycetoma Cryptococcosis Candidosis Piedra (eumycotic) Geotrichosis Coccidioidomycosis Candidosis Phaeohyphomycosis Dermatophytosis Zygomycosis Histoplasmosis Fusariosis Cryptococcosis Trichosporonosis Geotrichosis Paracoccidioidomyc osis Zygomycosis Fusariosis Trichosporonosis Sporotrichosis • Deep / subcutaneous mycosis • Sporothrix schenckii • Saprophytic , I.P. : 8-30 days • Geographical distribution Clinical varieties (Sporotrichosis) Cutaneous • Lymphangitic or Pulmonary lymphocutaneous Renal Systemic • Fixed or endemic Bone • Mycetoma like Joint • Cellulitic Meninges Lymphangitic form (Sporotrichosis) • Commonest • Exposed sites • Dermal nodule pustule ulcer sporotrichotic chancre) (Sporotrichosis) (Sporotrichosis) • Draining lymphatic inflamed & swollen • Multiple nodules along lymphatics • New nodules - every few (Sporotrichosis) days • Thin purulent discharge • Chronic - regional lymph nodes swollen - break down • Primary lesion may heal spontaneously • General health - may not be affected (Sporotrichosis) (Sporotrichosis) Fixed/Endemic variety (Sporotrichosis) • -

Human Fungal Pathogens
This is a free sample of content from Human Fungal Pathogens. Click here for more information on how to buy the book. The Spectrum of Fungi That Infects Humans Julia R. Ko¨hler1, Arturo Casadevall2, and John Perfect3 1Division of Infectious Diseases, Children’s Hospital, Harvard Medical School, Boston, Massachusetts 02115 2Departments of Microbiology and Immunology and Medicine, Division of Infectious Diseases, Albert Einstein College of Medicine, New York, New York 10461 3Division of Infectious Diseases, Duke Medical Center, Durham, North Carolina 27710 Correspondence: [email protected] Few among the millions of fungal species fulfill four basic conditions necessary to infect humans: high temperature tolerance, ability to invade the human host, lysis and absorption of human tissue, and resistance to the human immune system. In previously healthy individu- als, invasive fungal disease is rare because animals’sophisticated immune systems evolved in constant response to fungal challenges. In contrast, fungal diseases occur frequently in immunocompromised patients. Paradoxically, successes of modern medicine have put in- creasing numbers of patients at risk for invasive fungal infections. Uncontrolled HIV infection additionally makes millions vulnerable to lethal fungal diseases. A concerted scientific and social effort is needed to meet these challenges. ungal infections today are among the most by which living humans became substrates for Fdifficult diseases to manage in humans. fungi. Given the tremendous wealth of recent Some fungi cause disease in healthy people, but findings on fungal evolution, phylogenetics, ge- most fungal infections occur in individuals al- nomics, development, and pathogenesis, this ready experiencing serious illness, and frequent- overview will necessarily omit much work criti- ly jeopardize the success of the newest medical cal to our understanding of fungi, which the advances in cancer care, solid organ and hema- other articles in this collection will focus on in topoietic stem cell transplantation, neonatal detail. -

Dodecanol, Metabolite of Entomopathogenic Fungus
www.nature.com/scientificreports OPEN Dodecanol, metabolite of entomopathogenic fungus Conidiobolus coronatus, afects fatty acid composition and cellular immunity of Galleria mellonella and Calliphora vicina Michalina Kazek1*, Agata Kaczmarek1, Anna Katarzyna Wrońska1 & Mieczysława Irena Boguś1,2 One group of promising pest control agents are the entomopathogenic fungi; one such example is Conidiobolus coronatus, which produces a range of metabolites. Our present fndings reveal for the frst time that C. coronatus also produces dodecanol, a compound widely used to make surfactants and pharmaceuticals, and enhance favors in food. The main aim of the study was to determine the infuence of dodecanol on insect defense systems, i.e. cuticular lipid composition and the condition of insect immunocompetent cells; hence, its efect was examined in detail on two species difering in susceptibility to fungal infection: Galleria mellonella and Calliphora vicina. Dodecanol treatment elicited signifcant quantitative and qualitative diferences in cuticular free fatty acid (FFA) profles between the species, based on gas chromatography analysis with mass spectrometry (GC/MS), and had a negative efect on G. mellonella and C. vicina hemocytes and a Sf9 cell line in vitro: after 48 h, almost all the cells were completely disintegrated. The metabolite had a negative efect on the insect defense system, suggesting that it could play an important role during C. coronatus infection. Its high insecticidal activity and lack of toxicity towards vertebrates suggest it could be an efective insecticide. In their natural environment, insects have to cope with a variety of microorganisms, and as such, have developed a complex and efcient defense system. Te frst line of defense is a cuticle formed of several layers, with an epi- cuticle on the outside, a procuticle underneath it and an epidermis beneath that. -

Entomopathogenic Fungal Identification
Entomopathogenic Fungal Identification updated November 2005 RICHARD A. HUMBER USDA-ARS Plant Protection Research Unit US Plant, Soil & Nutrition Laboratory Tower Road Ithaca, NY 14853-2901 Phone: 607-255-1276 / Fax: 607-255-1132 Email: Richard [email protected] or [email protected] http://arsef.fpsnl.cornell.edu Originally prepared for a workshop jointly sponsored by the American Phytopathological Society and Entomological Society of America Las Vegas, Nevada – 7 November 1998 - 2 - CONTENTS Foreword ......................................................................................................... 4 Important Techniques for Working with Entomopathogenic Fungi Compound micrscopes and Köhler illumination ................................... 5 Slide mounts ........................................................................................ 5 Key to Major Genera of Fungal Entomopathogens ........................................... 7 Brief Glossary of Mycological Terms ................................................................. 12 Fungal Genera Zygomycota: Entomophthorales Batkoa (Entomophthoraceae) ............................................................... 13 Conidiobolus (Ancylistaceae) .............................................................. 14 Entomophaga (Entomophthoraceae) .................................................. 15 Entomophthora (Entomophthoraceae) ............................................... 16 Neozygites (Neozygitaceae) ................................................................. 17 Pandora -

Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2013 Mycology Laboratory Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 15 Mold Descriptions 16 M-1 Exserohilum species 16 M-2 Phialophora species 20 M-3 Chrysosporium species 25 M-4 Fusarium species 30 M-5 Rhizopus species 34 Yeast Descriptions 38 Y-1 Rhodotorula mucilaginosa 38 Y-2 Trichosporon asahii 41 Y-3 Candida glabrata 44 Y-4 Candida albicans 47 Y-5 Geotrichum candidum 50 Direct Detection - Cryptococcal Antigen 53 Antifungal Susceptibility Testing - Yeast 55 Antifungal Susceptibility Testing - Mold (Educational) 60 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally.