Human Fungal Pathogens
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fungal Infections from Human and Animal Contact
Journal of Patient-Centered Research and Reviews Volume 4 Issue 2 Article 4 4-25-2017 Fungal Infections From Human and Animal Contact Dennis J. Baumgardner Follow this and additional works at: https://aurora.org/jpcrr Part of the Bacterial Infections and Mycoses Commons, Infectious Disease Commons, and the Skin and Connective Tissue Diseases Commons Recommended Citation Baumgardner DJ. Fungal infections from human and animal contact. J Patient Cent Res Rev. 2017;4:78-89. doi: 10.17294/2330-0698.1418 Published quarterly by Midwest-based health system Advocate Aurora Health and indexed in PubMed Central, the Journal of Patient-Centered Research and Reviews (JPCRR) is an open access, peer-reviewed medical journal focused on disseminating scholarly works devoted to improving patient-centered care practices, health outcomes, and the patient experience. REVIEW Fungal Infections From Human and Animal Contact Dennis J. Baumgardner, MD Aurora University of Wisconsin Medical Group, Aurora Health Care, Milwaukee, WI; Department of Family Medicine and Community Health, University of Wisconsin School of Medicine and Public Health, Madison, WI; Center for Urban Population Health, Milwaukee, WI Abstract Fungal infections in humans resulting from human or animal contact are relatively uncommon, but they include a significant proportion of dermatophyte infections. Some of the most commonly encountered diseases of the integument are dermatomycoses. Human or animal contact may be the source of all types of tinea infections, occasional candidal infections, and some other types of superficial or deep fungal infections. This narrative review focuses on the epidemiology, clinical features, diagnosis and treatment of anthropophilic dermatophyte infections primarily found in North America. -

Emerging Fungal Infections Among Children: a Review on Its Clinical Manifestations, Diagnosis, and Prevention
Review Article www.jpbsonline.org Emerging fungal infections among children: A review on its clinical manifestations, diagnosis, and prevention Akansha Jain, Shubham Jain, Swati Rawat1 SAFE Institute of ABSTRACT Pharmacy, Gram The incidence of fungal infections is increasing at an alarming rate, presenting an enormous challenge to Kanadiya, Indore, 1Shri healthcare professionals. This increase is directly related to the growing population of immunocompromised Bhagwan College of Pharmacy, Aurangabad, individuals especially children resulting from changes in medical practice such as the use of intensive India chemotherapy and immunosuppressive drugs. Although healthy children have strong natural immunity against fungal infections, then also fungal infection among children are increasing very fast. Virtually not all fungi are Address for correspondence: pathogenic and their infection is opportunistic. Fungi can occur in the form of yeast, mould, and dimorph. In Dr. Akansha Jain, children fungi can cause superficial infection, i.e., on skin, nails, and hair like oral thrush, candida diaper rash, E-mail: akanshajain_2711@ yahoo.com tinea infections, etc., are various types of superficial fungal infections, subcutaneous fungal infection in tissues under the skin and lastly it causes systemic infection in deeper tissues. Most superficial and subcutaneous fungal infections are easily diagnosed and readily amenable to treatment. Opportunistic fungal infections are those that cause diseases exclusively in immunocompromised individuals, e.g., aspergillosis, zygomycosis, etc. Systemic infections can be life-threatening and are associated with high morbidity and mortality. Because diagnosis is difficult and the causative agent is often confirmed only at autopsy, the exact incidence of systemic infections is difficult to determine. The most frequently encountered pathogens are Candida albicans and Received : 16-05-10 Aspergillus spp. -

Epidemiological, Clinical and Diagnostic Aspects of Sheep Conidiobolomycosis in Brazil
Ciência Rural, Santa Maria,Epidemiological, v.46, n.5, p.839-846, clinical mai, and 2016 diagnostic aspects of sheep conidiobolomycosis http://dx.doi.org/10.1590/0103-8478cr20150935 in Brazil. 839 ISSN 1678-4596 MICROBIOLOGY Epidemiological, clinical and diagnostic aspects of sheep conidiobolomycosis in Brazil Aspectos epidemiológicos, clínicos e de diagnóstico da conidiobolomicose ovina no Brasil Carla WeiblenI Daniela Isabel Brayer PereiraII Valéria DutraIII Isabela de GodoyIII Luciano NakazatoIII Luís Antonio SangioniI Janio Morais SanturioIV Sônia de Avila BottonI* — REVIEW — ABSTRACT As lesões da conidiobolomicose normalmente são de caráter granulomatoso e necrótico, apresentando-se sob duas formas Conidiobolomycosis is an emerging disease caused clínicas: rinofacial e nasofaríngea. O presente artigo tem como by fungi of the cosmopolitan genus Conidiobolus. Particular objetivo revisar as principais características da doença em ovinos, strains of Conidiobolus coronatus, Conidiobolus incongruus and particularizando a epidemiologia, assim como os aspectos clínicos Conidiobolus lamprauges, mainly from tropical or sub-tropical e o diagnóstico das infecções causadas por Conidiobolus spp. no origin, cause the mycosis in humans and animals, domestic or Brasil. Neste País, a enfermidade é endêmica nas regiões nordeste wild. Lesions are usually granulomatous and necrotic in character, e centro-oeste, afetando ovinos predominantemente de raças presenting two clinical forms: rhinofacial and nasopharyngeal. deslanadas, ocasionando a morte na grande maioria dos casos This review includes the main features of the disease in sheep, with estudados. As espécies do fungo responsáveis pelas infecções an emphasis on the epidemiology, clinical aspects, and diagnosis em ovinos são C. coronatus e C. lamprauges e a forma clínica of infections caused by Conidiobolus spp. -
Human and Microbial Proteins from Corpora Amylacea of Alzheimer's
www.nature.com/scientificreports OPEN Human and Microbial Proteins From Corpora Amylacea of Alzheimer’s Disease Received: 24 November 2017 Diana Pisa1, Ruth Alonso1, Ana Isabel Marina1, Alberto Rábano2 & Luis Carrasco1 Accepted: 14 June 2018 Corpora amylacea (CA) are spherical bodies mainly composed of polyglucans and, to a lesser extent, Published: xx xx xxxx proteins. They are abundant in brains from patients with neurodegenerative diseases, particularly Alzheimer’s disease. Although CA were discovered many years ago, their precise origin and function remain obscure. CA from the insular cortex of two Alzheimer’s patients were purifed and the protein composition was assessed by proteomic analysis. A number of microbial proteins were identifed and fungal DNA was detected by nested PCR.A wide variety of human proteins form part of CA. In addition, we unequivocally demonstrated several fungal and bacterial proteins in purifed CA. In addition to a variety of human proteins, CA also contain fungal and bacterial polypeptides.In conclusion, this paper suggests that the function of CA is to scavenge cellular debris provoked by microbial infections. Several diferent types of polyglucan bodies have been found in the central nervous system (CNS) of elderly peo- ple, as well as in patients with a variety of pathologies, including Alzheimer’s disease (AD), epilepsy, amyotrophic lateral sclerosis (ALS), multiple sclerosis (MS) and hippocampal sclerosis1,2. Among these polyglucan structures, Lafora bodies, Bielschowsky bodies and corpora amylacea (CA) have been identifed based on their morphological characteristics3–5. Although CA were described early in the 18th century, their precise origin and potential function in normal or pathological conditions remains an enigma. -
Mycology Proficiency Testing Program
Mycology Proficiency Testing Program Test Event Critique January 2014 Table of Contents Mycology Laboratory 2 Mycology Proficiency Testing Program 3 Test Specimens & Grading Policy 5 Test Analyte Master Lists 7 Performance Summary 11 Commercial Device Usage Statistics 13 Mold Descriptions 14 M-1 Stachybotrys chartarum 14 M-2 Aspergillus clavatus 18 M-3 Microsporum gypseum 22 M-4 Scopulariopsis species 26 M-5 Sporothrix schenckii species complex 30 Yeast Descriptions 34 Y-1 Cryptococcus uniguttulatus 34 Y-2 Saccharomyces cerevisiae 37 Y-3 Candida dubliniensis 40 Y-4 Candida lipolytica 43 Y-5 Cryptococcus laurentii 46 Direct Detection - Cryptococcal Antigen 49 Antifungal Susceptibility Testing - Yeast 52 Antifungal Susceptibility Testing - Mold (Educational) 54 1 Mycology Laboratory Mycology Laboratory at the Wadsworth Center, New York State Department of Health (NYSDOH) is a reference diagnostic laboratory for the fungal diseases. The laboratory services include testing for the dimorphic pathogenic fungi, unusual molds and yeasts pathogens, antifungal susceptibility testing including tests with research protocols, molecular tests including rapid identification and strain typing, outbreak and pseudo-outbreak investigations, laboratory contamination and accident investigations and related environmental surveys. The Fungal Culture Collection of the Mycology Laboratory is an important resource for high quality cultures used in the proficiency-testing program and for the in-house development and standardization of new diagnostic tests. Mycology Proficiency Testing Program provides technical expertise to NYSDOH Clinical Laboratory Evaluation Program (CLEP). The program is responsible for conducting the Clinical Laboratory Improvement Amendments (CLIA)-compliant Proficiency Testing (Mycology) for clinical laboratories in New York State. All analytes for these test events are prepared and standardized internally. -

Jamaica UHSM ¤ 1,2* University Hospital Harish Gugnani , David W Denning of South Manchester NHS Foundation Trust ¤Professor of Microbiology & Epidemiology, St
Burden of serious fungal infections in Jamaica UHSM ¤ 1,2* University Hospital Harish Gugnani , David W Denning of South Manchester NHS Foundation Trust ¤Professor of Microbiology & Epidemiology, St. James School of Medicine, Kralendjik, Bonaire (Dutch Caribbean). 1 LEADING WI The University of Manchester, Manchester Academic Health Science Centre, Manchester, U.K. INTERNATIONAL 2 FUNGAL The University Hospital of South Manchester, (*Corresponding Author) National Aspergillosis Centre (NAC) Manchester, U.K. EDUCATION Background and Rationale The incidence and prevalence of fungal infections in Jamaica is unknown. The first human case of Conidiobolus coronatus infection was discovered in Jamaica (Bras et al. 1965). Cases of histoplasmosis and eumycetoma are reported (Fincharn & DeCeulaer 1980, Nicholson et al., 2004; Fletcher et al, 2001). Tinea capitis is very frequent in children Chronic pulmonary (East-Innis et al., 2006), because of the population being aspergillosis with aspergilloma (in the left upper lobe) in a 53- predominantly of African ancestry. In a one year study of 665 HIV yr-old, HIV-negative Jamaican male, developing after one infected patients, 46% of whom had CD4 cell counts <200/uL, 23 had year of antitubercular treatment; his baseline IgG pneumocystis pneumonia and 3 had cryptococcal meningitis (Barrow titer was 741 mg/L (0-40). As a smoker, he also had moderate et al. 2010). We estimated the burden of fungal infections in Jamaica emphysema. from published literature and modelling. Table 1. Estimated burden of fungal disease in Jamaica Fungal None HIV Respiratory Cancer ICU Total Rate Methods condition /AIDS /Tx burden 100k We also extracted data from published papers on epidemiology and Oesophageal ? 2,100 - ? - 2,100 77 from the WHO STOP TB program and UNAIDS. -

Epidemiology of Superficial Fungal Diseases in French Guiana: a Three
Medical Mycology August 2011, 49, 608–611 Epidemiology of superfi cial fungal diseases in French Guiana: a three-year retrospective analysis CHRISTINE SIMONNET * , FRANCK BERGER * & JEAN-CHARLES GANTIER † * Institut Pasteur de la Guyane , Cayenne , France , and † Institut Pasteur , Paris , France A three-year retrospective analysis of fungi isolated from specimens of patients with superfi cial fungal infections in French Guiana is presented. Clinical samples from 726 Downloaded from https://academic.oup.com/mmy/article/49/6/608/972117 by guest on 27 September 2021 patients with presumptive diagnoses of onychomycosis (28.2% of the patients), tinea capitis (27.8%), superfi cial cutaneous mycoses of the feet (22.0%), and of other areas of the body (21.9%), were assessed by microscopic examination and culture. Dermato- phytes accounted for 59.2% of the isolates, followed by yeasts (27.5%) and non-der- matophytic molds (13.1%). Trichophyton rubrum was the most common dermatophyte recovered from cases of onychomycosis (67.4%), tinea pedis (70.6%) and tinea corporis (52.4%). In contrast, Trichophyton tonsurans was the predominant species associated with tinea capitis (73.9%). Yeasts were identifi ed as the principal etiologic agents of onychomycosis of the fi ngernails (74.2%), whereas molds were found mainly in cases of onychomycosis of the toenails. In such instances, Neo s cytalidium dimidiatum (70.8%) was the most common mold recovered in culture. In conclusion, the prevalence of T. rubrum and the occurrence of onychomycosis and fungal infections of the feet in French Guiana are similar to results reported from Europe, whereas the frequency of tinea capi- tis and the importance of T. -

Fungal Infections
FUNGAL INFECTIONS SUPERFICIAL MYCOSES DEEP MYCOSES MIXED MYCOSES • Subcutaneous mycoses : important infections • Mycologists and clinicians • Common tropical subcutaneous mycoses • Signs, symptoms, diagnostic methods, therapy • Identify the causative agent • Adequate treatment Clinical classification of Mycoses CUTANEOUS SUBCUTANEOUS OPPORTUNISTIC SYSTEMIC Superficial Chromoblastomycosis Aspergillosis Aspergillosis mycoses Sporotrichosis Candidosis Blastomycosis Tinea Mycetoma Cryptococcosis Candidosis Piedra (eumycotic) Geotrichosis Coccidioidomycosis Candidosis Phaeohyphomycosis Dermatophytosis Zygomycosis Histoplasmosis Fusariosis Cryptococcosis Trichosporonosis Geotrichosis Paracoccidioidomyc osis Zygomycosis Fusariosis Trichosporonosis Sporotrichosis • Deep / subcutaneous mycosis • Sporothrix schenckii • Saprophytic , I.P. : 8-30 days • Geographical distribution Clinical varieties (Sporotrichosis) Cutaneous • Lymphangitic or Pulmonary lymphocutaneous Renal Systemic • Fixed or endemic Bone • Mycetoma like Joint • Cellulitic Meninges Lymphangitic form (Sporotrichosis) • Commonest • Exposed sites • Dermal nodule pustule ulcer sporotrichotic chancre) (Sporotrichosis) (Sporotrichosis) • Draining lymphatic inflamed & swollen • Multiple nodules along lymphatics • New nodules - every few (Sporotrichosis) days • Thin purulent discharge • Chronic - regional lymph nodes swollen - break down • Primary lesion may heal spontaneously • General health - may not be affected (Sporotrichosis) (Sporotrichosis) Fixed/Endemic variety (Sporotrichosis) • -

Mediastinal Mass in a Healthy Adolescent at the Children's
Chest clinic CASE BASED DISCUSSIONS Thorax: first published as 10.1136/thoraxjnl-2014-205764 on 10 October 2014. Downloaded from Mediastinal mass in a healthy adolescent at The Children’s Hospital at Westmead, Australia Ameneh Khatami,1 Alex C Outhred,1 Philip N Britton,1,2 Emilie Huguon,3 David J E Lord,4 Melanie Wong,5 Amanda Charlton,6 Alison M Kesson,1,2 David Isaacs1 For numbered affiliations see Ameneh Khatami and Emilie Huguon gamma release assay (IGRA) on whole blood was end of article. A previously well adolescent from the tropical positive. Percutaneous core biopsies of the medias- fi fi Correspondence to South Paci c island of Futuna was transferred due tinal mass demonstrated fungal hyphae in a broin- Dr Ameneh Khatami, to a 3-month to 4-month history of intermittent flammatory background and Splendore–Hoeppli Department of Infectious fevers, anorexia, weight loss, lethargy and haemop- phenomena (SHP) (figure 2A). Diseases and Microbiology, tysis. A Mantoux test was negative. CT scan ’ The Children s Hospital at demonstrated a large mediastinal mass and lymph- Westmead, Locked Bag 4001, Alison M Kesson and David Isaacs Westmead 2145, Australia; adenopathy with broncho-vascular compression, A positive IGRA in an adolescent from a [email protected]. and bilateral pleural and pericardial effusions, TB-endemic region is not unexpected. The histo- gov.au, ameneh.khatami@ (figure 1A). At admission, he was persistently gmail.com pathology suggests an invasive fungal infection, and febrile with non-tender cervical lymphadenopathy the patient’s raised eosinophil count would be con- Received 19 May 2014 and hepatomegaly, and had moderate respiratory sistent with this. -

Clinical Policy: Topical Agents: Anti-Fungals Reference Number: OH.PHAR.PPA.90 Effective Date: 01/01/2020 Revision Log Last Review Date: Line of Business: Medicaid
Clinical Policy: Topical Agents: Anti-Fungals Reference Number: OH.PHAR.PPA.90 Effective Date: 01/01/2020 Revision Log Last Review Date: Line of Business: Medicaid See Important Reminder at the end of this policy for important regulatory and legal information. Description NO PA REQUIRED “PREFERRED” PA REQUIRED “NON-PREFERRED” CICLOPIROX cream, gel, topical suspension, shampoo CICLOPIROX kit (generic of CNL® Nail lacquer kit) (generic of Loprox®) ERTACZO® (sertaconazole) CICLOPIROX solution (generic of Penlac®) EXELDERM® (sulconazole) CLOTRIMAZOLE (generic of Lotrimin®) JUBLIA® solution (efinaconazole) CLOTRIMAZOLE/BETAMETHASONE (generic of KERYDIN® solution (tavaborole) Lotrisone®) KETOCONAZOLE foam(generic of Extina®) ECONAZOLE (generic of Spectazole®) LUZU® (luliconazole) KETOCONAZOLE cream & shampoo (generic of Kuric®, MENTAX® (butenafine) Nizoral®) NAFTIFINE CREAM MICONAZOLE NAFTIN® GEL (naftifine) NYSTATIN OXICONAZOLE (generic of OXISTAT®) NYSTATIN/TRIAMCINOLONE PEDIADERM AF® cream (nystatin) TERBINAFINE (generic of Lamisil®) VUSION® ointment (miconazole/zinc) TOLNAFTATE (generic of Tinactin®) FDA approved indication(s) Ciclopirox is indicated for: • Topical treatment of mild to moderate onychomycosis of fingernails and toenails without lunula involvement, due to Trichophyton rubrum in immunocompetent patients (Penlac®, Ciclodan Nail Lacquer®) • Topical treatment of seborrheic dermatitis of the scalp (Loprox®) • Topical treatment of tinea corporis, tinea cruris, or tinea pedis (Epidermophyton floccosum; Microsporum canis; Trichophyton -
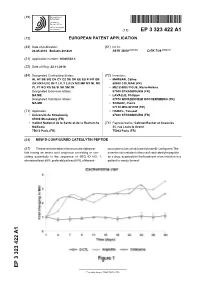
Ep 3323422 A1
(19) TZZ¥¥ ¥ _T (11) EP 3 323 422 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 23.05.2018 Bulletin 2018/21 A61K 38/00 (2006.01) C07K 7/08 (2006.01) (21) Application number: 16306539.4 (22) Date of filing: 22.11.2016 (84) Designated Contracting States: (72) Inventors: AL AT BE BG CH CY CZ DE DK EE ES FI FR GB • MARBAN, Céline GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO 68000 COLMAR (FR) PL PT RO RS SE SI SK SM TR • METZ-BOUTIGUE, Marie-Hélène Designated Extension States: 67000 STRASBOURG (FR) BA ME • LAVALLE, Philippe Designated Validation States: 67370 WINTZENHEIM KOCHERSBERG (FR) MA MD • SCHAAF, Pierre 67120 MOLSHEIM (FR) (71) Applicants: • HAIKEL, Youssef • Université de Strasbourg 67000 STRASBOURG (FR) 67000 Strasbourg (FR) • Institut National de la Santé et de la Recherche (74) Representative: Cabinet Becker et Associés Médicale 25, rue Louis le Grand 75013 Paris (FR) 75002 Paris (FR) (54) NEW D-CONFIGURED CATESLYTIN PEPTIDE (57) The present invention relates to a cateslytin pep- no acids residues of said cateslytin are D-configured. The tide having an amino acid sequence consisting or con- invention also relates to the use of said cateslytin peptide sisting essentially in the sequence of SEQ ID NO: 1, as a drug, especially in the treatment of an infection in a wherein at least 80%, preferably at least 90%, of the ami- patient in needs thereof. EP 3 323 422 A1 Printed by Jouve, 75001 PARIS (FR) EP 3 323 422 A1 Description Field of the Invention 5 [0001] The present invention relates to the field of medicine, in particular of infections. -

The New Species Concept in Dermatophytes—A Polyphasic Approach
Mycopathologia DOI 10.1007/s11046-008-9099-y The New Species Concept in Dermatophytes—a Polyphasic Approach Yvonne Gra¨ser Æ James Scott Æ Richard Summerbell Received: 15 October 2007 / Accepted: 30 January 2008 Ó Springer Science+Business Media B.V. 2008 Abstract The dermatophytes are among the most among these are the cosmopolitan bane of nails and frequently observed organisms in biomedicine, yet feet, Trichophyton rubrum, and the endemic African there has never been stability in the taxonomy, agent of childhood tinea capitis, Trichophyton identification and naming of the approximately 25 soudanense, which are effectively inseparable in all pathogenic species involved. Since the identification analyses. The molecular data require some reinter- of these species is often epidemiologically and pretation of results seen in conventional phenotypic ethically important, the difficulties in dermatophyte tests, but in most cases, phylogenetic insight is identification are a fruitful topic for modern molec- readily integrated with current laboratory testing ular biological investigation, done in tandem with procedures. renewed investigation of phenotypic characters. Molecular phylogenetic analyses such as multilocus Keywords Dermatophytes Á Taxonomy Á sequence typing have had to be tailored to accom- Molecular identification Á modate differing the mechanisms of speciation that Morphological identification Á Species concept have produced the dermatophytes that are commonly seen today. Even so, some biotypes that were unambiguously considered species in the past, based Introduction: Why Dermatophyte Biosystematics on profound differences in morphology and pattern of and Identification are Important (Medical infection, appear consistently not to be distinct and Scientific Aspects) species in modern molecular analyses. Most notable The dermatophytes belong to the small category of disease organisms that almost every human alive will Y.