1 Department of Radiology Residency Program Manual
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Cardiothoracic Fellowship Program
Cardiothoracic Fellowship Program Table of Contents Program Contact ............................................................................................ 3 Other contact numbers .................................................................................. 4 Introduction ........................................................................................................... 5 Goals and Objectives of Fellowship: ..................................................................... 6 Rotation Schedule: ........................................................................................ 7 Core Curriculum .................................................................................................... 8 Fellow’s Responsibilities ..................................................................................... 22 Resources ........................................................................................................... 23 Facilities ....................................................................................................... 23 Educational Program .......................................................................................... 26 Duty Hours .......................................................................................................... 29 Evaluation ........................................................................................................... 30 Table of Appendices .................................................................................... 31 Appendix A -
Screening Chest X-Ray Interpretations and Radiographic Techniques IOM GUIDELINES FIRST EDITION Iii
FIRST EDITION 2015 Screening Chest X-Ray Interpretations and Radiographic Techniques IOM GUIDELINES Global Radiology Coordination and Teleradiology Centre Migration Health Division International Organization for Migration (Manila Administrative Centre) 24th floor Citibank Tower, Paseo De Roxas 8741, Makati city 1226 Metro Manila, Philippines Email: [email protected] • [email protected] Tel: +632 230 1674 The opinions expressed in the report are those of the authors and do not necessarily reflect the views of the International Organization for Migration (IOM). The designations employed and the presentation of material throughout the report do not imply the expression of any opinion whatsoever on the part of IOM concerning the legal status of any country, territory, city or area, or of its authorities, or concerning its frontiers or boundaries. IOM is committed to the principle that humane and orderly migration benefits migrants and society. As an intergovernmental organization, IOM acts with its partners in the international community to: assist in meeting the operational challenges of migration; advance understanding of migration issues; encourage social and economic development through migration; and uphold the human dignity and well-being of migrants. Author Sifrash Meseret GELAW, MD Radiologist, MPH; Global Radiology Coordinator IOM, Manila Administrative Centre, Manila, Philippines Major Contributor Anthony MACDERMOTT, MD former Global HAP Quality Coordinator, IOM, Regional Office for Asia and the Pacific, Bangkok, Thailand Additional -
Radiology Fundamentals: Introduction to Imaging & Technology
Radiology Fundamentals Harjit Singh ● Janet A Neutze Editors Jonathan R Enterline ● Joseph S Fotos Associate Editors Jonathan J Douds ● Megan Jenkins Kalambo ● Marsha J Bluto Contributing Editors Radiology Fundamentals Introduction to Imaging & Technology Fourth Edition Editors Harjit Singh, MD, FSIR Janet A Neutze, MD Professor of Radiology, Surgery, Associate Professor of Radiology and Medicine Associate Division Chief, Ultrasound Director of Education, Penn State Heart Co-director, Radiology Medical Student and Vascular Institute Education Program Fellowship Director, Cardiovascular Pennsylvania State College of Medicine and Interventional Radiology Penn State Hershey Medical Center Pennsylvania State College of Medicine Hershey, PA, USA Penn State Hershey Medical Center [email protected] Hershey, PA, USA [email protected] Associate Editors Jonathan R Enterline, MD Joseph S Fotos, MD Resident, Department of Radiology Resident, Department of Radiology Pennsylvania State College of Medicine Pennsylvania State College of Medicine Penn State Hershey Medical Center Penn State Hershey Medical Center Hershey, PA, USA Hershey, PA, USA Contributing Editors Jonathan J Douds, BS Megan Jenkins Kalambo, MD Medical Student Resident, Department of Radiology Pennsylvania State College of Medicine University of Texas Health Science Center Penn State Hershey Medical Center at Houston, Houston, TX, USA Hershey, PA, USA Marsha J Bluto, MD Practicing Physician Physical Medicine and Rehabilitation Mill Valley, CA, USA ISBN 978-1-4614-0943-4 e-ISBN 978-1-4614-0944-1 DOI 10.1007/978-1-4614-0944-1 Springer New York Dordrecht Heidelberg London Library of Congress Control Number: 2011938463 © Springer Science+Business Media, LLC 2012 All rights reserved. This work may not be translated or copied in whole or in part without the written permission of the publisher (Springer Science+Business Media, LLC, 233 Spring Street, New York, NY 10013, USA), except for brief excerpts in connection with reviews or scholarly analysis. -

İstanbul University Cerrahpaşa Medical Faculty 2015-2016 Academic Year Synopsis of Curricula
İstanbul University Cerrahpaşa Medical Faculty 2015-2016 Academic Year Synopsis of Curricula For details visit: http://www.ctf.edu.tr/egitim_ogretim/indexen.htm Istanbul University, Cerrahpaşa Medical Faculty 2015-2016 Academic Year Synopsis of Curricula; Version 14-Jul-15; Page 1/125 Table of Contents 1st Year Courses .................................................................................................................................. 3 Course 1.1: Introduction to Medical Sciences ..................................................................................... 3 Course 1.2: Cell Tissue and Organ Systems I ...................................................................................... 8 Course 1.3: Cell Tissue and Organ Systems II .................................................................................. 12 Course 1.4: Introduction to Clinical Medicine ................................................................................... 19 2nd Year Courses ............................................................................................................................... 25 Course 2.1: Locomotor System .......................................................................................................... 25 Course 2.2: Cardiovascular System ................................................................................................... 28 Course 2.3: Respiratory System ......................................................................................................... 32 Course 2.4: -

CHEST RADIOLOGY: Goals and Objectives
Harlem Hospital Center Department of Radiology Residency Training Program CHEST RADIOLOGY: Goals and Objectives ROTATION 1 (Radiology Years 1): Resident responsibilities: • ED chest CTs • Inpatient and outpatient plain films including the portable intensive care unit radiographs • Consultations with referring clinicians MEDICAL KNOWLEDGE: • Residents must demonstrate knowledge about established and evolving biomedical, clinical, and cognitive sciences and the application of this knowledge to patient care. At the end of the rotation, the resident should be able to: • Identify normal radiographic and CT anatomy of the chest • Identify and describe common variants of normal, including aging changes. • Demonstrate a basic knowledge of radiographic interpretation of atelectasis, pulmonary infection, congestive heart failure, pleural effusion and common neoplastic diseases of the chest • Identify the common radiologic manifestation of thoracic trauma, including widened mediastinum, signs of aortic laceration, pulmonary contusion/laceration, esophageal and diaphragmatic rupture. • Know the expected postoperative appearance in patients s/p thoracic surgery and the expected location of the life support and monitoring devices on chest radiographs of critically ill patients (intensive care radiology); be able to recognize malpositioned devices. • Identify cardiac enlargement and know the radiographic appearance of the dilated right vs. left atria and right vs. left ventricles, and pulmonary vascular congestion • Recognize common life-threatening -

Pneumonia (CAP)
肺實質化病變與肺塌陷 胸腔內科周百謙醫師 Dr. Pai-chien Chou MD PhD Department of Thoracic Medicine Taipei Medical University Hospital Chest X-ray • P-A view • Lateral view • Oblique view • Lordotic view • Expiratory film • Decubitus view • Overpenetrated grid film The Elements of a chest x-ray (CXR) • The Broncho-vascular markings in the lung • The borders of the heart • The contours of the mediastinum and pleural space • The ribs and spine Segmental anatomy Segmental Anatomy Cardiomediastinal outlines on Chest X-ray Density of image ◆ Gas ◆ Water ◆ Fat ◆ Metal and bone ◆ Thinking of pathogenesis Basic thinking of a lesion on Chest X-ray ◆ Size ◆ Location (Silhouette sign) – Anterior, posterior – Which lobe is involved ◆ Intrapulmonary (Air bronchogram sign) ◆ Extrapulmonary (Incomplete border sign) Infiltrate in the lungs • Fluid accumulates in lung, predominate in the alveolar (airspace) compartment or the interstitial compartment. interstitial compartment Lymphatic compartment Alveolar unit Vascular unit Air space opacification The opacification is caused by fluid or solid material within the airways that causes a difference in the relative attenuation of the lung: • transudate, e.g. pulmonary edema secondary to heart failure • pus, e.g. bacterial pneumonia • blood, e.g. pulmonary hemorrhage • cells, e.g. bronchoalveolar carcinoma • protein, e.g. alveolar proteinosis • fat, e.g. lipoid pneumonia • gastric contents, e.g. aspiration pneumonia • water, e.g. drowning When considering the likely causes of airspace opacification, it is useful to determine chronicity -

Signs in Chest Imaging
Diagn Interv Radiol 2011; 17:18–29 CHEST IMAGING © Turkish Society of Radiology 2011 PICTORIAL ESSAY Signs in chest imaging Oktay Algın, Gökhan Gökalp, Uğur Topal ABSTRACT adiological practice includes classification of illnesses with similar A radiological sign can sometimes resemble a particular object characteristics through recognizable signs. Knowledge of and abil- or pattern and is often highly suggestive of a group of similar pathologies. Awareness of such similarities can shorten the dif- R ity to recognize these signs can aid the physician in shortening ferential diagnosis list. Many such signs have been described the differential diagnosis list and deciding on the ultimate diagnosis for for X-ray and computed tomography (CT) images. In this ar- ticle, we present the most frequently encountered plain film a patient. In this report, 23 important and frequently seen radiological and CT signs in chest imaging. These signs include for plain signs are presented and described using chest X-rays, computed tomog- films the air bronchogram sign, silhouette sign, deep sulcus raphy (CT) images, illustrations and photographs. sign, Continuous diaphragm sign, air crescent (“meniscus”) sign, Golden S sign, cervicothoracic sign, Luftsichel sign, scim- itar sign, doughnut sign, Hampton hump sign, Westermark Plain films sign, and juxtaphrenic peak sign, and for CT the gloved finger Air bronchogram sign sign, CT halo sign, signet ring sign, comet tail sign, CT an- giogram sign, crazy paving pattern, tree-in-bud sign, feeding Bronchi, which are not normally seen, become visible as a result of vessel sign, split pleura sign, and reversed halo sign. opacification of the lung parenchyma. -
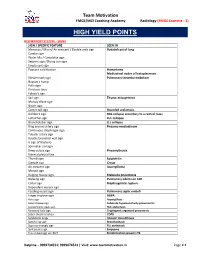
High Yield Points
Team Motivation FMGE/MCI Coaching Academy Radiology (FMGE Essentia - 3) HIGH YIELD POINTS RESPIRATORY SYSTEM – SIGNS SIGN / SPECIFIC FEATURE SEEN IN Meniscus / Moon/ Air crescent / Double arch sign Hydatid cyst of lung Cumbo sign Water lilly / Camalotte sign Serpent sign / Rising sun sign Empty cyst sign Popcorn calcification Hamartoma Mediastinal nodes of histoplasmosis Westermark sign Pulmonary thrombo-embolism Hapton’s hump Palla sign Fleishner lines Felson’s sign Sail sign Thymic enlargement Mulvay Wave sign Notch sign Comet tail sign Rounded atelectasis Golden S sign RUL collapse secondary to a central mass Luftsichel sign LUL collapse Broncholobar sign LLL collapse Ring around artery sign Pneumo-mediastinum Continuous diaphragm sign Tubular artery sign Double bronchial wall sign V sign of Naclerio Spinnaker sail sign Deep sulcus sign Pneumothorax Visceral pleural line Thumb sign Epiglottitis Steeple sign Croup Air crescent sign Aspergilloma Monod sign Bulging fissure sign Klebsiella pneumonia Batwing sign Pulmonary edema on CXR Collar sign Diaphragmatic rupture Dependant viscera sign Feeding vessel sign Pulmonary septic emboli Finger in glove sign ABPA Halo sign Aspergillosis Head cheese sign Subacute hypersensitivity pneumonitis Juxtaphrenic peak sign RUL atelectasis Reversed halo sign Cryptogenic organized pneumonia Saber sheath trachea COPD Sandstorm lungs Alveolar microlithiasis Signet ring sign Bronchiectasis Superior triangle sign RLL atelectasis Split pleura sign Empyema Tree in bud sign on HRCT Endobronchial spread in TB -

100 CASES in Radiology This Page Intentionally Left Blank 100 CASES in Radiology
100 CASES in Radiology This page intentionally left blank 100 CASES in Radiology Robert Thomas Specialist Registrar, Guy’s and St Thomas’ Hospital, London, UK James Connelly Specialist Registrar, Guy’s and St Thomas’ Hospital, London, UK Christopher Burke Specialist Registrar, Guy’s and St Thomas’ Hospital, London, UK 100 Cases Series Editor: Professor P John Rees MD FRCP Dean of Medical Undergraduate Education, King’s College London School of Medicine at Guy’s, King’s and St Thomas’ Hospitals, London, UK First published in Great Britain in 2012 by Hodder Arnold, an imprint of Hodder Education, Hodder and Stoughton Ltd, a division of Hachette UK 338 Euston Road, London NW1 3BH http://www.hodderarnold.com © 2012 Robert Thomas, James Connelly and Christopher Burke All rights reserved. Apart from any use permitted under UK copyright law, this publication may only be reproduced, stored or transmitted, in any form, or by any means with prior permission in writing of the publishers or in the case of reprographic production in accordance with the terms of licences issued by the Copyright Licensing Agency. In the United Kingdom such licences are issued by the Copyright Licensing Agency: Saffron House, 6–10 Kirby Street, London EC1N 8TS. Hachette UK’s policy is to use papers that are natural, renewable and recyclable products and made from wood grown in sustainable forests. The logging and manufacturing processes are expected to conform to the environmental regulations of the country of origin. Whilst the advice and information in this book are believed to be true and accurate at the date of going to press, neither the author[s] nor the publisher can accept any legal responsibility or liability for any errors or omissions that may be made. -

Chest Imaging Using Signs, Symbols, and Naturalistic Images
Chiarenza et al. Insights into Imaging (2019) 10:114 https://doi.org/10.1186/s13244-019-0789-4 Insights into Imaging EDUCATIONAL REVIEW Open Access Chest imaging using signs, symbols, and naturalistic images: a practical guide for radiologists and non-radiologists Alessandra Chiarenza1, Luca Esposto Ultimo1, Daniele Falsaperla1, Mario Travali1, Pietro Valerio Foti1, Sebastiano Emanuele Torrisi2,3, Matteo Schisano2, Letizia Antonella Mauro1, Gianluca Sambataro2,4, Antonio Basile1, Carlo Vancheri2 and Stefano Palmucci1* Abstract Several imaging findings of thoracic diseases have been referred—on chest radiographs or CT scans—to signs, symbols, or naturalistic images. Most of these imaging findings include the air bronchogram sign, the air crescent sign, the arcade-like sign, the atoll sign, the cheerios sign, the crazy paving appearance, the comet-tail sign, the darkus bronchus sign, the doughnut sign, the pattern of eggshell calcifications, the feeding vessel sign, the finger- in-gloove sign, the galaxy sign, the ginkgo leaf sign, the Golden-S sign, the halo sign, the headcheese sign, the honeycombing appearance, the interface sign, the knuckle sign, the monod sign, the mosaic attenuation, the Oreo- cookie sign, the polo-mint sign, the presence of popcorn calcifications, the positive bronchus sign, the railway track appearance, the scimitar sign, the signet ring sign, the snowstorm sign, the sunburst sign, the tree-in-bud distribution, and the tram truck line appearance. These associations are very helpful for radiologists and non-radiologists and increase learning and assimilation of concepts. Therefore, the aim of this pictorial review is to highlight the main thoracic imaging findings that may be associated with signs, symbols, or naturalistic images: an “iconographic” glossary of terms used for thoracic imaging is reproduced— placing side by side radiological features and naturalistic figures, symbols, and schematic drawings. -

Juerg Hodler Rahel A. Kubik-Huch Gustav K. Von Schulthess Editors Diagnostic and Interventional Imaging
IDKD Springer Series Series Editors: Juerg Hodler · Rahel A. Kubik-Huch · Gustav K. von Schulthess Juerg Hodler Rahel A. Kubik-Huch Gustav K. von Schulthess Editors Diseases of the Chest, Breast, Heart and Vessels 2019–2022 Diagnostic and Interventional Imaging IDKD Springer Series Series Editors Juerg Hodler Department of Radiology University Hospital of Zürich Zürich, Switzerland Rahel A. Kubik-Huch Department of Radiology Kantonsspital Baden Zürich, Switzerland Gustav K. von Schulthess Deptartment of Nuclear Medicine University Hospital of Zürich Zürich, Switzerland The world-renowned International Diagnostic Course in Davos (IDKD) represents a unique learning experience for imaging specialists in training as well as for experienced radiologists and clinicians. IDKD reinforces his role of educator offering to the scientific community tools of both basic knowledge and clinical practice. Aim of this Series, based on the faculty of the Davos Course and now launched as open access publication, is to provide a periodically renewed update on the current state of the art and the latest developments in the field of organ- based imaging (chest, neuro, MSK, and abdominal). More information about this series at http://www.springer.com/series/15856 Juerg Hodler • Rahel A. Kubik-Huch Gustav K. von Schulthess Editors Diseases of the Chest, Breast, Heart and Vessels 2019–2022 Diagnostic and Interventional Imaging Editors Juerg Hodler Rahel A. Kubik-Huch Department of Radiology Department of Radiology University Hospital of Zürich Kantonsspital Baden -

Rotation: VGH Chest Radiography VGH 899 West 12Th Ave., Vancouver, BC V5Z 1M9
Rotation: VGH Chest Radiography VGH 899 West 12th Ave., Vancouver, BC V5Z 1M9 Level: PGY 2‐5 Rotation Supervisor: Dr. Ana‐Maria Bilawich During the course of the four years, residents will receive one month of chest radiography training as a junior resident and one month of chest radiography training as a senior resident. Residents are expected to develop graded responsibility as they rise from junior to senior resident level. Each resident will be given guidance at the beginning of a rotation, an interim evaluation will occur mid rotation, and a final evaluation will be given at the end of each rotation. Each final evaluation will be submitted to the residency training program director. All residents are expected to arrive in the department by 0800 hours and stay until the conclusion of the working day. Ongoing teaching and interaction with the staff occurs throughout the day. If a resident is absent from his/her chest plain radiography rotation for any reason, he/she should give ample warning to Dr. Mayo (Chest Section Head) and Dr. Bilawich (rotation supervisor). Vacation and conference requests must be booked with Dr. Mayo and Dr. Bilawich in advance, at least two weeks prior to any planned absence from the rotation. Medical Expert: 1. Basic Science: a) Knowledge of anatomy (PA and lateral chest radiographs) At the end of first Chest radiography rotation, the junior resident (PGY2/3) will demonstrate learning all of the following anatomy on PA and lateral chest radiographs. At the end of the second Chest radiography rotation, the senior resident (PGY4/5) will demonstrate learning all of the following anatomy on PA and lateral chest radiographs.