LESOTHO Global AIDS Response Country Progress Report January
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sacu Member States Geographic and Economic Profiles Sacu Member States Geographic and Economic Profiles
SACU MEMBER STATES GEOGRAPHIC AND ECONOMIC PROFILES SACU MEMBER STATES GEOGRAPHIC AND ECONOMIC PROFILES BOTSWANA ESWATINI LESOTHO NAMIBIA SOUTH AFRICA PB 1 SACU MEMBER STATES GEOGRAPHIC AND ECONOMIC PROFILES SACU MEMBER STATES GEOGRAPHIC AND ECONOMIC PROFILES This Publication aims to provide a succinct overview on the geographical and economic indicators of the SACU VISION Member States. An economic community with equitable and sustainable development, dedicated to the welfare of its people for a common ABOUT SACU future. The Southern African Customs Union (SACU) is the oldest Customs Union in the world, having been established in 1910 MISSION between the then Union of South Africa (current Republic of South Africa) and the then British High Commission Territories of Basutoland (now the Kingdom of Lesotho), Bechuanaland (now the Republic of Botswana) and the Kingdom of Swaziland Serve as an engine for regional integration and development, industrial and economic diversification, the expansion of (now the Kingdom of Eswatini).South-West Africa (now the Republic of Namibia) – then a colony of South Africa – was a de intra-regional trade and investment, and global competitiveness. facto member of SACU at the time. (a) Build economic policy coherence, harmonization and convergence to meet the development needs of the region; The political changes following the independence of Botswana, Swaziland and Lesotho (BLS) in the 1960s necessitated a (b) Promote sustainable economic growth and development for employment creation and poverty reduction; re-negotiation of the 1910 Agreement. This culminated in the conclusion of the Agreement between the BLS and South (c) Serve as a building block of an ever-closer community amongst the peoples of Southern Africa; Africa in 1969. -

Remarks by the Right Honourable the Prime Minister of the Kingdom of Lesotho, Dr
REMARKS BY THE RIGHT HONOURABLE THE PRIME MINISTER OF THE KINGDOM OF LESOTHO, DR. MOEKETSI MAJORO ON THE OCCASION OF THE 50TH ANNIVERSARY OF THEEXISTANCE OF FORMAL DIPLOMATIC RELATIONS BETWEEN THE KINGDOM OF LESOTHO AND JAPAN 29th JULY, 2021 Program Director, please allow me to begin by paying my respects to: • His Majesty King Letsie III, • Honourable Deputy Prime Minister, • Honourable Ministers and Deputy Ministers, • Your Excellency the Ambassador of Japan to the Kingdom of Lesotho, Mr. Maruyama Norio, • Senior Government Officials, • Distinguished Guests, • Ladies and Gentlemen. As I begin my remarks this morning Your Excellency, I wish to note that the Government of Lesotho has learnt with a deep sense of regret of the passing away of your dear father a few days ago. I therefore take this opportunity to convey to you, and through you, to the entire family, our deepest condolences and words of sympathy for this untimely loss of a loved one. Our hearts and minds are with you during this challenging time. Today, is a great day in the history of our two countries. A day on which I join you, with great pleasure and jubilation in commemoration of the 50th anniversary of the establishment of formal diplomatic relations between the Kingdom of Lesotho and Japan. On this auspicious day in the history of our two sister countries, I invite You, Your Excellency, and all those who are with us today, to congratulate ourselves for the long standing cordial bonds of friendship and cooperation that have so happily subsisted between our two countries and their peoples. -

TANKISO LUCIA MOTJOPE-MOKHALI Submitted in Accordance with the Requirements for the Degree of Doctor of Literature and Philosoph
A COMPARATIVE ANALYSIS OF SESUTO-ENGLISH DICTIONARY AND SETHANTŠO SA SESOTHO WITH REFERENCE TO LEXICAL ENTRIES AND DICTIONARY DESIGN by TANKISO LUCIA MOTJOPE-MOKHALI submitted in accordance with the requirements for the degree of Doctor of Literature and Philosophy in the subject African Language at the UNIVERSITY OF SOUTH AFRICA SUPERVISOR: PROFESSOR I.M. KOSCH CO-SUPERVISOR: PROFESSOR M.J. MAFELA November 2016 Student No.: 53328183 DECLARATION I, Tankiso Lucia Motjope-Mokhali, declare that A Comparative Analysis of Sesuto- English Dictionary and Sethantšo sa Sesotho with Reference to Lexical Entries and Dictionary Design is my own work and that all the sources that I have used or cited have been indicated and acknowledged by means of complete references. Signature……………………………… Date………………………….. i ACKNOWLEDGEMENTS I thank God for giving me the strength, power, good health and guidance to complete this race. I would not have made it if it were not for His mercy. As the African saying affirms ‘A person is a person because of other people’, which in Sesotho is translated as Motho ke motho ka batho, I believe that this thesis would not have been completed if it had not been for the assistance of other people. In particular, I extend my sincere gratitude to my Supervisors Professor I.M. Kosch and Professor M.J. Mafela for their guidance throughout the completion of this thesis. Their hard work, encouragement, constant support (both academically and personally) as well as their insightful comments offered throughout this study, gave me courage to continue. My special thanks also go to NIHSS/SAHUDA for its financial support during the carrying out of this study. -

UNICEF Lesotho
Data Requirement Analysis and Data Mapping UNICEF Lesotho September 2018 PREPARED BY Ms. Paige Kirby Development Gateway, Inc. 1110 Vermont Ave NW Suite 500 Washington, DC 20008 USA Cover image: © UNICEF/UN04420/Marrion Table of Contents LIST OF ABBREVIATIONS 4 EXECUTIVE SUMMARY 5 I. INTRODUCTION 5 II. LESOTHO CONTEXT 6 III. DATA DEMAND 6 IV. DATA SUPPLY 7 V. DATA USE AND ECOSYSTEM OPPORTUNITIES 7 VI. CONCLUSION 7 INTRODUCTION 8 I. PROJECT BACKGROUND 8 A. DIAGNOSTIC REPORT OVERVIEW 8 II. PURPOSE AND INTENDED USE 9 LESOTHO CONTEXT 10 I. SITUATIONAL OVERVIEW 10 A. POLITICAL ECONOMY 11 II. STRATEGIC PRIORITIES AND PROCESSES 12 A. GOVERNMENT OF LESOTHO 12 B. UNICEF LESOTHO PROCESSES AND PRIORITIES 14 III. OTHER ECOSYSTEM ACTORS 16 IV. SECTION CONCLUSION 17 DATA DEMAND 18 I. INTRODUCTION 18 II. GOVERNMENT PRIORITIES 18 A. DATA DEMANDERS 18 B. DATA PRODUCERS 19 C. DATA DEMANDERS AND PRODUCERS 19 III. UNICEF PRIORITIES 21 A. OUTCOME AREA 1 22 B. OUTCOME AREA 2 23 C. OUTCOME AREA 3 24 D. OUTCOME AREA 4 25 IV. PROMINENT NEEDS 26 A. POLICY COMPLIANCE 26 B. LEADERSHIP 27 V. SECTION CONCLUSION 28 DATA SUPPLY 29 I. INTRODUCTION 29 II. EXISTING DATA SOURCES 29 | 2 A. GOVERNMENT DATA SOURCES 30 B. OTHER UNICEF DATA SOURCES 35 III. PROMINENT NEEDS 36 A. ACCESS 36 B. AVAILABILITY 37 C. TIMELINESS 39 D. QUALITY 40 E. CAPACITY 42 IV. SECTION CONCLUSION 44 DATA USE 45 I. INTRODUCTION 45 II. EXISTING PROCESSES 46 A. GOVERNMENT 46 B. UNICEF 46 C. MAPPING DEMAND AGAINST SUPPLY 46 III. PROMINENT NEEDS 48 A. CAPACITY 48 B. -

The Executive Survey General Information and Guidelines
The Executive Survey General Information and Guidelines Dear Country Expert, In this section, we distinguish between the head of state (HOS) and the head of government (HOG). • The Head of State (HOS) is an individual or collective body that serves as the chief public representative of the country; his or her function could be purely ceremonial. • The Head of Government (HOG) is the chief officer(s) of the executive branch of government; the HOG may also be HOS, in which case the executive survey only pertains to the HOS. • The executive survey applies to the person who effectively holds these positions in practice. • The HOS/HOG pair will always include the effective ruler of the country, even if for a period this is the commander of foreign occupying forces. • The HOS and/or HOG must rule over a significant part of the country’s territory. • The HOS and/or HOG must be a resident of the country — governments in exile are not listed. • By implication, if you are considering a semi-sovereign territory, such as a colony or an annexed territory, the HOS and/or HOG will be a person located in the territory in question, not in the capital of the colonizing/annexing country. • Only HOSs and/or HOGs who stay in power for 100 consecutive days or more will be included in the surveys. • A country may go without a HOG but there will be no period listed with only a HOG and no HOS. • If a HOG also becomes HOS (interim or full), s/he is moved to the HOS list and removed from the HOG list for the duration of their tenure. -

ARBEITSHILFE Zur Projektsammlung 2019/2020 Des Kinderwerks Der Evangelisch-Methodistischen Kirche in Deutschland Inhalt
ARBEITSHILFE zur Projektsammlung 2019/2020 des Kinderwerks der Evangelisch-methodistischen Kirche in Deutschland Inhalt Liebe Mitarbeitende und Unterstützende von „Kinder helfen Kindern“ 2019/2020 ......................................................................... 3 Unsere Autoren ���������������������������������������������������������������������������������������������������������������������������������������������������������������������������������������������������������� 5 Lesotho – das Königreich im Himmel ................................................................................................................................................................. 6 Die Lage Lesothos und Besonderheiten • Wasserreichtum in Lesotho ................................................................................................. 7 Wer wohnt in Lesotho? ��������������������������������������������������������������������������������������������������������������������������������������������������������������������������������������������� 8 Das Klima in Lesotho ������������������������������������������������������������������������������������������������������������������������������������������������������������������������������������������������ 9 Die Wirtschaft Lesothos ........................................................................................................................................................................................ 10 Thema Gesundheit in Lesotho • Bildung in Lesotho ................................................................................................................................... -

Letlhogonolo Mpho Letshele
COPYRIGHT AND CITATION CONSIDERATIONS FOR THIS THESIS/ DISSERTATION o Attribution — You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use. o NonCommercial — You may not use the material for commercial purposes. o ShareAlike — If you remix, transform, or build upon the material, you must distribute your contributions under the same license as the original. How to cite this thesis Surname, Initial(s). (2012). Title of the thesis or dissertation (Doctoral Thesis / Master’s Dissertation). Johannesburg: University of Johannesburg. Available from: http://hdl.handle.net/102000/0002 (Accessed: 22 August 2017). A CRITICAL ANALYSIS OF THE RECURRENCE OF COUPS IN THE KINGDOM OF LESOTHO – 1970-2014 A Dissertation Submitted to the Department of Politics and International Relations of the Faculty of Humanities at the University of Johannesburg by Letlhogonolo Mpho Letshele 201417806 October 2019 In Fulfilment of the Requirements For the Degree of MASTER OF ARTS IN POLITICS AND INTERNATIONAL RELATIONS Johannesburg, South Africa Supervisor: Prof Annie Barbara Chikwanha Co-Supervisor: Prof Chris Landsberg 1 ABSTRACT Since its independence, the Kingdom of Lesotho has experienced the recurrence of coups (1970-2014). A process of re-democratisation was attempted in the country in 1993 but another coup succeeded the elections. The next elections in 1998 were marked by the worst political violence in the history of Lesotho. Electoral reforms were then introduced in 2002. Still, the reforms did not prevent the coup attempt in 2014. -
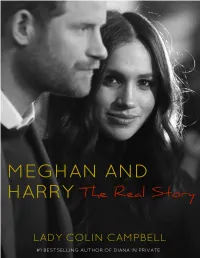
Meghan and Harry That They Would Have to Accept What Was on Offer and Not Demand What Was Not
Contents Title Page Chapter 1 Chapter 2 Chapter 3 Chapter 4 Chapter 5 Chapter 6 Chapter 7 Chapter 8 Chapter 9 Chapter 10 Chapter 11 Chapter 12 Photo Section Copyright CHAPTER 1 On May 19th 2018, when Meghan Markle stepped out of the antique Rolls Royce conveying her and her mother Doria Ragland from the former Astor stately home Cliveden to St. George’s Chapel, Windsor, where she was due to be married at 12 noon, she was a veritable vision of loveliness. At that moment, one of the biggest names of the age was born. As the actress ascended the steps of St. George’s Chapel, its interior and exterior gorgeously decorated in the most lavish and tasteful spring flowers, she was a picture of demure and fetching modesty, stylish elegance, transparent joyousness, and radiant beauty. The simplicity of her white silk wedding dress, designed by Clare Waight Keller of Givenchy, with its bateau neckline, three-quarter length sleeves, and stark, unadorned but stunningly simple bodice and skirt, coupled with the extravagant veil, five metres long and three metres wide, heavily embroidered with two of her favourite flowers (wintersweet and California poppy, as well as the fifty three native flowers of the various Commonwealth countries, and symbolic crops of wheat, and a piece of the blue dress that the bride had worn on her first date with the groom), gave out a powerful message. All bridal gowns make statements. Diana, Princess of Wales, according to her friend Carolyn Pride, used hers to announce to the world, ‘Here I am. -

Executive Database 10 September 2020 Nb
EXECUTIVE DATABASE 10 SEPTEMBER 2020 NB: THIS DATABASE IS BASED ON INFORMATION RECEIVED FROM SA MISSIONS POLITICAL DESKS FOREIGN MISSIONS COUNTRY HEAD OF STATE DATE OF HEAD OF GOVERNMENT DATE OF MINISTER OF FOREIGN CAPITAL CITY INAUGURATION (PRIME MINISTER) APPOINTMENT AFFAIRS African Union HE Mr Matamela Cyril 12/02/2020 HE Mr Moussa Faki 14/03/2017 Addis Ababa (AU) Ramaphosa Mahamat Chairperson Chairperson of the African Union Commission0 Islamic Republic HE Mr Ashraf Ghani 29/09/2014 Chief Executive 29/09/2014 HE Haroon Kabul of Afghanistan Chakhansuri (acting) President Mr Abdullah Abdullah Minister of Foreign Affairs 23/01/2020 Republic of HE Mr Ilir Rexhep Metaj 24/07/2017 HE Mr Edi Rama 15/09/2013 HE Mr Edi Rama Tirana Albania President Prime Minister Prime Minister and Minister of Foreign Affairs 21/01/2019 Gent Cakaj Deputy Minister of Foreign Affairs (with full responsibility as a Minister) 22/01/2019 Democratic HE Mr Abdelmadjid Tebboune 19/12/2019 HE Mr Abdelaziz Djerad 28/12/2019 HE Ms Sabri Boukadoum Algiers People’s President Prime Minister presiding Minister of Foreign Affairs Republic of over the Council of and International Algeria Ministers Cooperation Head of Government 02/04/2019 Principality of HE Bishop Joan Enric VIVES I 16/05/2019 HE Mr Xavier Espot 17/07/2017 HE Mrs Maria Ubach Font Andorra La Andorra SICILIA Zamora Vella Minister of Foreign Affairs (Co-Prince of Andorra) Prime Minister (Letters to each HE Mr Emmanuel Macron Co-Prince) (Co-Prince of Andorra) Republic of HE Mr João Manuel 26/09/2017 HOS is -

Abstracts from the Regional Psychosocial Support Forum 2013
Regional Psychosocial Support Forum 2013 Mainstreaming Psychosocial Support for Child Protection: Linking Evidence and Practice Book of Abstracts October 29 – 31 Kenyatta International Conference Centre Nairobi Kenya Contents PLENARY SEssIONS 5 Plenary 1: 6 Plenary 2: 8 Plenary 3: 10 Plenary 4: 13 TRACK SEssIONS 17 Track 1: Child Protection Programs 1 18 Track 2: Parenting 22 Track 3: Highly vulnerable populations 23 Track 4: Economic Strengthening 27 Track 5: Disclosure 30 Track 6: Education 33 Track 7: Humanitarian Emergencies 1 36 Track 8: Child Trafficking & Labour 39 Track 9: Child Protection Programs 2 42 Track 10: Humanitarian Emergencies 2 47 Track 11: Children Living with HIV 1 52 Track 12: Children Living with HIV 2 56 Track 13: Capacity Building for CP Systems Strengthening 59 Track 14: Children Living with Disability 62 Track 15: Child Protection Programmes 3 65 Contents SKILLS BUILDING SEssIONS AND SPECIAL SESSIONS 70 Skills Building Session 1: 71 Skills Building Session 2: 73 Skills Building Session 3: 74 Skills Building Sessions 4: 75 Skills Building Session 5: 77 Skills Building Session 6: 77 Skills Building Session 7: 78 Skills Building Session 8: 79 Special Session 1: 80 Special Session 2: 81 Special Session 3: 82 Special Session 4: 83 ACKNOWLEDGEMENts 84 Plenary Sessions 5 Plenary 1: GOVERNMENT OF KENYA: CHILD PROTECTION FRAMEWORK Ahmed Hussein (Government of Kenya) Abstract not available at time of printing INTEGRATION OF PSYCHOSOCIAL SUppOrt IN CARE AND SUppOrt TO OVC: A HOLIstIC ApprOACH Ana Rosa Durão Gama Mondle, Linda Lovick, Juliana Canjera, Integration of Psychosocial Support in Care and Support to OVC A Holistic Approach Issues: In Mozambique, as in many other developing countries, orphans and vulnerable children (OVC) living in households affected by HIV/AIDS are turned into caregivers for sick parents, and also for their younger brothers and sisters. -

List of Participants Information Received by Wednesday, 20 September 2017
General Conference GC (61)/INF/3 Date: 22 September 2017 General Distribution English only Sixty-first regular session Vienna, 18–22 September 2017 List of Participants Information received by Wednesday, 20 September 2017 Pages 1. Member States 1–137 2. Entities Having Received a Standing Invitation to 138 Participate as Observers 3. United Nations and Specialized Agencies 139 4. Other Intergovernmental Organizations 140–144 5. Non-Governmental Organizations 145–152 The List of Participants contains information as provided by delegations. Member States Ms Nandini VENKATA Intern Permanent Mission in Vienna Afghanistan Head of Delegation: Mr Mohammad Ibrahim GHAFOORI Albania Deputy Director General Head of Delegation: United Nations and International Conferences Department Ms Ravesa LLESHI Ministry of Foreign Affairs Minister Plenipotentiary Charge d'Affaires, a.i. Alternates: Permanent Mission to the IAEA in Vienna Mr Mohammad Naeem POYESH Other members: Counsellor Chargé d'Affaires Mr Adhurim RESULI Permanent Mission to the IAEA in Vienna Minister Plenipotentiary Alternate to the Resident Representative Advisers: Permanent Mission to the IAEA in Vienna Mr Abdulhai NAZIFI Ms Viola KALOSHI Director General First Secretary Afghan Atomic Energy High Commission Alternate to the Resident Representative Permanent Mission to the IAEA in Vienna Mr Shirin Aqa ZARIF Director Mr Jovan THERESKA Kabul Medical University Expert Adviser Permanent Mission in Vienna Other members: Mr Alisadiq AKBARI Second Secretary Algeria Permanent Mission in Vienna -

H.M. King Bhumibol Adulyadej
President of the United States, Donald J. Trump, sent a Presidential Delegation to attend the cremation ceremony. President Trump extended his condolences and said “the late King was a champion of the Thai people… and his innovative work, diplomacy, and 70 years of selfless service will ensure that his legacy will live on for many generations to come.” In Memoriam The special envoy of China’s President Xi H.M. King Bhumibol Adulyadej Jinping, Vice-Premier Zhang Gaoli attended December 5, 1927 – October 13, 2016 the royal cremation ceremony and expressed China's deep condolences and reverence to The cremation and ceremonies for our the late king and conveyed President Xi's best beloved departed King have now concluded. wishes to King Vajiralongkorn. Zhang said “the We sincerely thank everyone for all the kind late King had made a great contribution to the words of support and thoughtful sharing development of Thailand and the with us during our difficult times. Over 50 improvement of the Thai people's livelihoods countries sent dignitaries and official and was also a great friend of the Chinese delegations to attend the cremation and people.” funeral ceremonies including HM Queen Silvia of Sweden, HM Queen Maxima of the Federal Minister for Energy Awais Ahmad Netherlands, HM Queen Mathilde of Khan Leghari of Pakistan attended the Royal Belgium, HM Queen Sofia of Spain, HRH cremation ceremony and said “the late King Crown Prince Frederik of Denmark, HRH played a fundamental role in the development Crown Prince Haakon Magnus of Norway, of Thailand and the wellbeing of the Thai Their Majesties King Letsie III and Queen people.