Geographical and Temporal Distribution of the Residual Clusters of Human Leptospirosis in China, 2005–2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Annual Report 2019 CORPORATE INFORMATION
CONTENTS 2 Company Profile 3 Corporate Information 5 Financial Highlights 7 Chairman’s Statement 8 Management Discussion and Analysis 29 Report of Directors 55 Directors and Senior Management 59 Corporate Governance Report 69 Environmental, Social and Governance (ESG) Report 97 Independent Auditor’s Report 101 Consolidated Statement of Profit or Loss and Other Comprehensive Income 102 Consolidated Statement of Financial Position 104 Consolidated Statement of Changes in Equity 105 Consolidated Statement of Cash Flows 107 Notes to the Consolidated Financial Statements 167 Definitions MANAGEMENT DISCUSSION AND ANALYSIS Company Profile We are one of the leading private education service groups in Chengdu, Sichuan Province, the PRC with a track record of more than 18 years in the provision of private education services. Through our schools, we provide education services to students of different age groups from kindergarten to high school. As at 1 September 2019, we operated a total 11 schools, comprising six kindergartens, one primary and middle school, two middle schools and one middle and high school in Chengdu, as well as one primary and middle school in each of Bazhong, Guangyuan and Ziyang, Sichuan Province. As at 1 September 2019, we had an enrollment of 12,082 students supported by 1,709 employees, including 986 teachers. Since 2001, we have built the foundation of our business We aim to provide quality education services with a strong upon private preschool education and expanded our emphasis on the all-round development of students. footprints to the private primary and middle school With increasing demand for quality private education education industry. In June 2001, we established Chengdu from parents in the PRC, we have undergone significant Youshi Experimental Kindergarten, our first kindergarten development since the opening of our first school in 2001. -

Research on the Influencing Factors of the Construction of Tourism and Leisure Characteristic Towns in Sichuan Province Under Th
2021 International Conference on Education, Humanity and Language, Art (EHLA 2021) ISBN: 978-1-60595-137-9 Research on the Influencing Factors of the Construction of Tourism and Leisure Characteristic Towns in Sichuan Province under the Background of New Urbanization Yi-ping WANG1,a,* and Xian-li ZHANG2,b 1,2School of Business, Southwest Jiaotong University Hope College, Chengdu, Sichuan, China [email protected], [email protected] *Corresponding author Keywords: Tourism and leisure characteristic towns, Influencing factors, New urbanization. Abstract. Promoting the construction of characteristic towns under the background of new urbanization is an important way for my country to break the bottleneck of economic development and realize economic transformation and upgrading. In recent years, although the construction of characteristic towns in Sichuan Province has achieved remarkable results and a large number, especially tourist and leisure characteristic towns accounted for the largest proportion, they still face urgent problems such as avoiding redundant construction, achieving scientific development, and overall planning. This study takes 20 cultural tourism characteristic towns selected by the first batch of Sichuan Province as the research object, combined with field research and tourist questionnaire surveys, and screened out relevant influencing factors of characteristic towns from different aspects such as transportation, economy, industry, ecology, historical and cultural heritage. Analyze the correlation with the development level of characteristic towns in order to find out the key factors affecting the development of characteristic towns of this type, provide a policy basis for the scientific development and overall planning of reserve characteristic towns in our province, and contribute to the construction of new urbanization And provide advice and suggestions on the development of tourism industry in our province. -
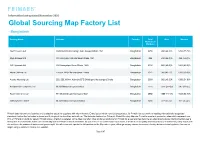
Primark Does Not Own Any Factories and Is Selective About the Suppliers with Whom We Work
Information last updated November 2020 Global Sourcing Map Factory List - Bangladesh Factory Name Address Country Total Men Women Number of Workers A&A Trousers Ltd Haribaritek Pubail College Gate Gazipur Dhaka 1721 Bangladesh 2250 996 (44.3)% 1254 (55.7)% Afiya Knitwear Ltd 10/ 2 Durgapur Ashulia Savar Dhaka 1341 Bangladesh 496 232 (46.8)% 264 (53.2)% AKH Apparels Ltd 128 Hemayetpur Savar Dhaka 1340 Bangladesh 2136 855 (40.0)% 1281 (60.0)% Alpha Clothing Ltd Tenguri, BKSP Ashulia Savar Dhaka Bangladesh 1971 968 (49.1)% 1003 (50.9)% Ananta Huaxiang Ltd 222, 223, H2-H4, Adamjee EPZ Shiddirgonj Narayanganj Dhaka Bangladesh 2038 982 (48.2)% 1056 (51.8)% Anowara Knit Composite Ltd Mulaid Mawna Sreepur Gazipur Bangladesh 2276 1329 (58.4)% 947 (41.6)% Aspire Garments Ltd 491 Dhalla Singair Manikganj 1822 Bangladesh 2992 1389 (46.4)% 1603 (53.6)% ASR Sweater Limited Mulaied Maona Sreepur Gazipur Bangladesh 1458 927 (63.6)% 531 (36.4)% Primark does not own any factories and is selective about the suppliers with whom we work. Every factory which manufactures product for Primark has to commit to meeting internationally recognised standards, before the first order is placed and throughout the time they work with us. The factories featured on Primark’s Global Sourcing Map are Primark’s suppliers’ production sites which represent over 95% of Primark products for sale in Primark stores. A factory is detailed on the Map only after it has produced products for Primark for a year and has become an established supplier. During the first year a factory has to demonstrate that it can consistently work to Primark’s ethical standards, as well as meet our commercial requirements in areas such as quality and timely delivery. -

TITLE HERE Introductions to Chengdu Tianfu International Airport and Ziyang City
TITLE HERE Introductions to Chengdu Tianfu International Airport and Ziyang City Chengdu Tianfu International Airport Chengdu Tianfu International Airport locates in Lu Jia Town, jianyang city. Chengdu Tianfu International Airport is only 18 kilometers away from Ziyang CBD while 50 kilometers away from the center of Chengdu CBD. The airport is positioned as Hub Airport, which plans to put into public in 2020. Chengdu Tianfu International Airport has facilitated development of airport economy for Ziyang, which 45-50 km2 has been included into airport economy zone. We plan to develop manufacturing service and high-tech agriculture and form industrial clusters including airport service, modern logistic, cultural innovation, thus making it an international center for foreign exchanges. Our visit this time is expected to exchange ideas with local government and industrial zone which have good practice in this regard, assimilate what works best. Also, we wish to build relationship in airport manufacturing, service sector and agriculture for possible cooperation in future. Ziyang City Located in the central part of Sichuan Basin, Ziyang was established as a prefecture in 1998 and upgraded to the status of city in 2000. It governs Yanjiang District, Anyue County and Lezhi County, covering an area of 5,747 km2 and with a total population of 3.55 million. Ziyang has a long History and rich culture. Back to 35,000 years ago, ancestors of Ziyang people unlocked the gate of the human civilization of Sichuan. In 135BC under the rule of Western Han Dynasty, counties are set up here then followed by state and prefecture, and the history of governmental establishment has stretched to more than 2100 years. -

Advanced Manufacturing Processing Technology Forum
2020 Advanced Manufacturing Processing Technology Forum Focus: Equipment Manufacturing, Electronic Information Automobile Manufacturing May 12-13th | Chengdu·China Sponsors www.ringierevents.com Background: Manufacturing is the foundation of modern industry. Under the background of the continuous deepening of “Made in China 2025”, the traditional manufacturing industry is facing deeply transformation and upgrad- ing.The future industry is steadily moving towards large-scale flexible manufacturing, full-process transparent production, distributed production, and intelligent automatic production. How to improve the productivity, reduce manufacturing costs, and accelerate the innovation and quality management of quality products have become common problems of many manufacturing enterprises. In this context,2020 Advanced Manufacturing Processing Technology Forum will be held in Chengdu on May 12-13th.The conference theme is "Efficient Production, Manufacturing Upgrade",and will focus on southwest China manufacturing market,discussed the hot topics such as machining technology, material selection, and process improvement in the production process of the company, and jointly explored effective "intelligence" solutions! Highlights: Business200+ Thematic Professional18+ Featured30+ 2+ Speaker Elite venue Booth Hot Topics: Section1:High Performance Machining and Section 2: Material Selection and Intelligent Production Process Change - How to build an intelligent production line? - Advanced cutting process for hard and brittle materials - How will -

Download Document
CDM-PoA-VCR-FORM Verification and certification report form for CDM programme of activities (version 02.0) Complete this form in accordance with the instructions attached at the end of this form. BASIC INFORMATION Title and UNFCCC reference number of Title: Sichuan Rural Poor-Household Biogas Development the programme of activities (PoA) Programme UNFCCC reference number: 2898 Version number(s) of the PoA-DD(s) to which this report applies 2 Version number of the verification and certification report 01 Completion date of the verification and certification report 17/08/2018 th Monitoring period number and duration Monitoring period number: 5 of this morning period Duration of this morning period: 01/01/2016 – 31/12/2016 (both days are included) Number and version number of the Number of the monitoring report: Single monitoring report monitoring report to which this report is prepared for all covered CPAs for this monitoring period applies Version number of the monitoring report: 2 Coordinating/managing entity (CME) Chengdu Oasis Science & Technology Co., Ltd. Host Parties Is this a host Party to a CPA Host Parties of the PoA covered in this report? (yes/no) People’s Republic of China Yes Applied methodologies and standardized Methodologies: AMS-I.I.– Biogas/biomass thermal baselines applications for households/small users (version 04) (EB68, Annex 25); AMS-III.R.– Methane recovery in agricultural activities at household/small farm level (version 02) (EB59, Annex 4) Standardized baselines: N/A Mandatory sectoral scopes linked to the Scope -

Global Sourcing Map Factory List - Bangladesh
Information last updated July 2018 Global Sourcing Map Factory List - Bangladesh Factory Name Address Country Total Men Women Number of Workers Afiya Knitwear Ltd 10/ 2 Durgapur Ashulia Savar Dhaka 1341 Bangladesh 579 288 (49.7)% 291 (50.3)% AKH Apparels Ltd 128 Hemayetpur Savar Dhaka 1340 Bangladesh 2188 971 (44.4)% 1217 (55.6)% AKH Eco Apparels Ltd 495 Balitha Shah-Belishwer Dhamrai Dhaka 1800 Bangladesh 5418 3000 (55.4)% 2418 (44.6)% Alpha Knitting Wear Limited 888 Shewrapara, 1St & 2Nd Floor Begum Rokeya Shoroni Mirpur Dhaka 1216 Bangladesh 2307 682 (29.6)% 1625 (70.4)% Ananta Denim Technology Ltd Noyabari Kanchpur Sonargaon Narayanganj Bangladesh 4833 2394 (49.5)% 2439 (50.5)% Ananta Huaxiang Ltd 222, 223, H2-H4, Adamjee Epz Shiddirgonj Narayanganj Dhaka Bangladesh 2039 1184 (58.1)% 855 (41.9)% Anowara Knit Composite Ltd Mulaid Mawna Sreepur Gazipur Bangladesh 1979 1088 (55.0)% 891 (45.0)% Apex Lingerie Limited Chandora Kaliakoir Gazipur Bangladesh 3937 2041 (51.8)% 1896 (48.2)% Arunima Sportswear Ltd Dewan Idris Road Zirabo Ashulia Savar Dhaka Bangladesh 4481 2561 (57.2)% 1920 (42.8)% Primark does not own any factories and is selective about the suppliers with whom we work. Every factory which manufactures product for Primark has to commit to meeting internationally recognised standards, before the first order is placed and throughout the time they work with us. The factories featured on Primark’s Global Sourcing Map are Primark’s suppliers’ production sites which represent over 95% of Primark products for sale in Primark stores. A factory is detailed on the Map only after it has produced products for Primark for a year and has become an established supplier. -

Download Document
Verification and certification report form for GS programme of activities (version 02.0) Complete this form in accordance with the instructions attached at the end of this form. BASIC INFORMATION Title and UNFCCC reference number of Title: Sichuan Rural Poor-Household Biogas Development the programme of activities (PoA) Programme GS Registration Reference Number:PoA GS1239 UNFCCC reference number: 2898 Version number(s) of the PoA-DD(s) to which this report applies 2 Version number of the verification and certification report 01 Completion date of the verification and certification report 18/10/2019 th Monitoring period number and duration Monitoring period number: 5 of this morning period Duration of this morning period: 01/01/2016 – 31/12/2016 (both days are included) Version number of the monitoring report to which this report applies 2.1 Coordinating/managing entity (CME) Chengdu Oasis Science & Technology Co., Ltd. Host Parties Is this a host Party to a CPA Host Parties of the PoA covered in this report? (yes/no) People’s Republic of China Yes Applied methodologies and standardized Methodologies: AMS-I.I.– Biogas/biomass thermal baselines applications for households/small users (version 04) (EB68, Annex 25); AMS-III.R.– Methane recovery in agricultural activities at household/small farm level (version 02) (EB59, Annex 4) Standardized baselines: N/A Mandatory sectoral scopes linked to the Scope 1: Energy industries (renewable - / non-renewable applied methodologies sources) Scope 13: Waste handling and disposal Conditional sectoral -

Open Dissertation-XIANG.Pdf
The Pennsylvania State University The Graduate School The College of the Liberal Arts LAND, CHURCH, AND POWER: FRENCH CATHOLIC MISSION IN GUANGZHOU, 1840-1930 A Dissertation in History by Hongyan Xiang 2014 Hongyan Xiang Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy August 2014 ii The dissertation of Hongyan Xiang was reviewed and approved* by the following: Ronnie Hsia Edwin Earle Sparks Professor of History Dissertation Advisor Chair of Committee David G. Atwill Associate Professor of History and Asian Studies Kate Merkel-Hess Assistant Professor of History and Asian Studies Anouk Patel-Campillo Assistant Professor of Rural Sociology Michael Kulikowski Professor of History and Classics and Ancient Mediterranean Studies Head, Department of History *Signatures are on file in the Graduate School iii Abstract This is a study of the economic and financial history of the Paris Foreign Missions Society (Société des Missions Étrangères de Paris) in the southern Chinese province of Guangdong (formerly known as Canton) from the late nineteenth to the early twentieth century. It examines how missionaries acquired and utilized local properties, demonstrating how property acquisitions provided a testing ground for Sino-Western relations. While historians have typically focused on the ways that missionaries affected Chinese populations and policies, I instead argue that living and attempting to gain influence in Guangdong altered missionaries’ tactics and strategies in ways that had far-reaching consequences. The government of China (which over the course of my study changed from an empire to a republic) consistently attempted to restrict foreign missions’ right to purchase Chinese properties. -

Western Provinces Rural Water Supply, Sanitation and Hygiene Promotion Project (World Bank / DFID)
E1491 v 4 Western Provinces Rural Water Supply, Sanitation and Hygiene Promotion Project (World Bank / DFID) Public Disclosure Authorized Sichuan Province ABSTRACT OF DAM SAFETY IN 20 PERCENT OF PROJECT AREAS Public Disclosure Authorized Southwest Jiaotong University Public Disclosure Authorized Nov.2006 Public Disclosure Authorized Contents 1 Brief Introduction to the Project ..............................................................................1 2 Basic Information of the Dams in 20 Percent of Project Areas.................................1 3 Description of Dam Safety ......................................................................................4 3.1 Safety of the Dams Already Appraised .........................................................4 3.2 Analysis of the Safety Appraisal Results of the Dams...................................6 4 The Counter-measures for Safety Problems of the Dams .........................................6 5 Proposals Concerning the Safety Management of the Dams...................................12 5.1 Requirements for the Dams yet to be Appraised..........................................12 5.2 Requirements for Dams Already Appraised ................................................14 5.3 Monitoring of Dam Safety ..........................................................................16 5.4 Fund Sources for Dam Safety Management ................................................17 6 Conclusion and Suggestions..................................................................................17 -

Major Chinese Industrial Companies
AllChinaReports.com Industry Reports, Company Reports & Industry Analysis Directory: Major Chinese Industrial Companies ● 186 Industries ● 1435 Top Companies ● 999 Company Websites Beijing Zeefer Consulting Ltd. April 2012 Disclaimer Authorized by: Beijing Zeefer Consulting Ltd. Company Site: http://www.Zeefer.org Online Store of China Industry Reports: http://www.AllChinaReports.com Beijing Zeefer Consulting Ltd. and (or) its affiliates (hereafter, "Zeefer") provide this document with the greatest possible care. Nevertheless, Zeefer makes no guarantee whatsoever regarding the accuracy, utility, or certainty of the information in this document. Further, Zeefer disclaims any and all responsibility for damages that may result from the use or non-use of the information in this document. The information in this document may be incomplete and/or may differ in expression from other information in elsewhere by other means. The information contained in this document may also be changed or removed without prior notice. Table of Contents CIC Code Industry Page 0610 Coal Mining 1 0620 Lignite Mining 2 0690 Other Coal Mining 3 0710 Crude Petroleum & Natural Gas Extraction 3 0810 Iron Ores Mining 5 1320 Feed Processing 6 1331 Edible Vegetable Oil Processing 7 1332 Inedible Vegetable Oil Processing 8 1340 Sugar Mfg. 9 1351 Livestock & Poultry Slaughtering 10 1352 Meat Processing 11 1361 Frozen Aquatic Products Processing 12 1411 Pastry & Bread Mfg. 13 1419 Biscuit & Other Baked Foods Mfg. 14 1421 Candy & Chocolate Mfg. 16 1422 Preserved Fruits Mfg. 17 1431 Rice & Flour Products Mfg. 18 1432 Quick Frozen Foods Mfg. 19 1439 Instant Noodle & Other Convenient Foods Mfg. 21 1440 Liquid Dairy & Dairy Products Mfg. -

World Bank Document
41555 Public Disclosure Authorized China Western Provinces Rural Water Supply, Sanitation and Hygiene Promotion Project Procurement Plan for Sichuan Province The annual procurement plan was prepared according to the content of the 2007-2008 annual plan and requirements of the procurement manual while considering the actual needs of project work in Sichuan Province. The Public Disclosure Authorized procurement plan consists of provincial procurement and county procurement, the former is the procurement of the goods and consultancy required by the public activity component, while the latter is the procurement of civil works and part of the consultancy. For the county procurement, some of the 20% projects counties has been reviewed by WB therefore it could be commenced in a early stage. The other 80% county projects could only be commenced upon annual plan approved by the WB. This procurement plan Public Disclosure Authorized lists the Summary of the procurement at provincial level and 20% project counties, and the procurement plan of the 80% of the project will be worked out after the approval of the annual work plan, according to the contents of the approval, and then report to the World Bank for Approval. Procurement packaging plan for the rest of the counties are included in the procurement section of the annual plan for each county. Public Disclosure Authorized Summary of the Provincial Procurement Plan Procurement of Goods National Competitive Bidding(NCB) Shopping Procurement (Shopping/Small Civil Works) Procurement Type Cost Estimate