Provisional Peer-Reviewed Toxicity Values for Rubidium Compounds
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
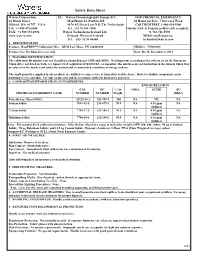
Safety Data Sheet 1
Safety Data Sheet 1. Waters Corporation EU: Waters Chromatography Europe B.V. FOR CHEMICAL EMERGENCY 34 Maple Street Mon Plaisir 12, Postbus 215 24 Hours per Day, 7 Days per Week Milford, MA 01757 U.S.A. 4870 AE Etten-Leur N B, The Netherlands Call CHEMTREC 1-800-424-9300 Tel: +1 508 478-2000 Tel: +31 76 508 1800 Outside USA & Canada (collect calls accepted) FAX: +1 508 872-1990 Waters Technologies Ireland Ltd +1 703-741-5970 www.waters.com Drinagh, Wexford, Ireland MSDS email inquiries: Tel: +353 53 91 60400 [email protected] 1. IDENTIFICATION Product: MassPREP™ Calibration Mix - DIOS Low Mass, PN 186002820 MSDS #: 715001038 Product Use: For laboratory use only. Date: Rev B, December 1, 2014 2. HAZARDS IDENTIFICATION: The calibration kit mixtures are not classified as hazardous per GHS and OSHA. Not dangerous according to the criteria set by the European Union (EU); not listed in Table 3.1 Annex VI of regulation 1272/2008/EU, as amended. The mixtures are not hazardous in the form in which they are placed on the market and under the normal and recommended conditions of storage and use. The small quantities supplied in our products are unlikely to cause severe or immediate health effects. However idodide compounds can be irritating to eyes and skin. Use only as directed and in accordance with safe laboratory practices. 3. COMPOSITION/INFORMATION ON INGREDIENTS: EXPOSURE LIMITS CAS EC % by OSHA ACGIH EU CHEMICAL INGREDIENT NAME NUMBER NUMBER Weight IOELV Polyethylene Glycol (PEG) 25322-68-3 203-989-9 100 NA NE NA Sodium Iodide 7681-82-5 231-679-3 99.9 NA 0.01 ppm NA (iodides) Cesium Iodide 7789-17-5 232-145-2 99.9 NA 0.01 ppm NA (iodides) Rubidium Iodide 7790-29-6 232-198-1 99.9 NA 0.01 ppm NA (iodides) Notes: Kit contains dried calibration mixtures: Polyethylene Glycol in a range of molecular weights (MW 200, 600, 1000); 50 ug of Sodium Iodide; 50 ug Rubidium Iodide; and 12.5 ug Cesium Iodide. -

WO 2015/084416 Al 11 June 2015 (11.06.2015) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2015/084416 Al 11 June 2015 (11.06.2015) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C09K 8/05 (2006.01) C07C 51/42 (2006.01) kind of national protection available): AE, AG, AL, AM, COW 17/00 (2006.01) E21B 21/06 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, (21) Number: International Application DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/US20 13/076445 HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, (22) International Filing Date: KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, 19 December 2013 (19. 12.2013) MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (25) Filing Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, (26) Publication Language: English TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 61/910,976 3 December 2013 (03. 12.2013) US (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant: CABOT CORPORATION [US/US]; Two GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, Seaport Lane, Suite 1300, Boston, MA 01220 (US). -

Thermal Studies on Rubidium Dinitramide
University of Huddersfield Repository Charsley, Edward L., Laye, Peter G., Markham, H.M., Rooney, James J., Berger, B., Griffiths, Trevor T. and Wasko, M.P. Thermal Studies on Rubidium Dinitramide Original Citation Charsley, Edward L., Laye, Peter G., Markham, H.M., Rooney, James J., Berger, B., Griffiths, Trevor T. and Wasko, M.P. (2008) Thermal Studies on Rubidium Dinitramide. In: 35th International Pyrotechnics Seminar, 13-18 July 2008, Fort Collins, USA. This version is available at http://eprints.hud.ac.uk/id/eprint/15577/ The University Repository is a digital collection of the research output of the University, available on Open Access. Copyright and Moral Rights for the items on this site are retained by the individual author and/or other copyright owners. Users may access full items free of charge; copies of full text items generally can be reproduced, displayed or performed and given to third parties in any format or medium for personal research or study, educational or not-for-profit purposes without prior permission or charge, provided: • The authors, title and full bibliographic details is credited in any copy; • A hyperlink and/or URL is included for the original metadata page; and • The content is not changed in any way. For more information, including our policy and submission procedure, please contact the Repository Team at: [email protected]. http://eprints.hud.ac.uk/ Proceedings 35 th International Pyrotechnic Seminar, Fort Collins, USA, IPSUSA, INC, 2008, 331. Thermal Studies on Rubidium Dinitramide E.L.Charsley l, P.G.Laye 1, H.M.Markham 1, J.J.Rooney 1, B.Berger 2, T.T.Griffiths 3 and M. -

Everything Chemistry Poster
Common Polyatomic Ions by Charge and Ion Family Functional Groups +1 Charge -1 Charge -2 Charge -3 Charge H + - 2- 3- | Ammonium NH4 Dihydrogen phosphite H2PO3 Hydrogen phosphite HPO3 Phosphite PO3 R—OH Alcohol 1° H—C—R + - 2- 3- Hydronium H3O Dihydrogen phosphate H2PO4 Hydrogen phosphate HPO4 Phosphate PO4 | - 2- 3- H Hydrogen carbonate HCO Carbonate CO Hypophosphite PO 3 3 2 - 2- 3- H Ammonia NH3 Hydrogen sulfite HSO3 Sulfite SO3 Arsenite AsO3 R | - 2- 3- | Hydrogen sulfate HSO Sulfate SO Arsenate AsO Amine 2° H—C—R 4 4 4 R—N—R - 2- | Nitrite NO2 Thiosulfate S2O3 - 2- R’ Nitrate NO3 Silicate SIO3 -4 Charge H - 2- 4- Hydroxide OH Carbide C2 Pyrophosphate P2O7 | R—O—R C - 2- Ether 3° R”—C—R Acetate CH3COO Oxalate C2O4 - 2- | Chromite CrO2 Chromate CrO4 R’ - 2- Cyanide CN Dichromate Cr2O7 H R’” - 2- O Cyanate CNO Tartrate C4H4O6 || | - 2- Aldehyde 4° R”—C—R Thiocyanate CNS Molybdate MoO R—C—H 4 | E - 2- Superoxide O2 Peroxide O2 R’ - 2- Permanganate MnO Disulfide S 4 2 O R - 2- Amide n-butyl M Hypochlorite ClO Oxalate C2O4 || | - R—C—N—R R Chlorite ClO2 - Chlorate ClO3 Strong Acids and Bases O I - Carboxylic Acid iso-butyl Perchlorate ClO4 Acids Bases || R Hypobromite BrO- Hydrochloric Acid HCl Lithium Hydroxide LiOH R—C—OH S - Bromite BrO2 Hydrobromic Acid HBr Sodium Hydroxide NaOH O - Ester || sec-butyl Bromate BrO3 Hydroiodic Acid HI Potassium Hydroxide KOH R—C—O—R R Perbromate BrO - Nitric Acid HNO Rubidium Hydroxide RbOH T 4 3 - Hypoiodite IO Sulfuric Acid H2SO4 Cesium Hydroxide CsOH O - Ketone || tert-butyl Iodite IO2 Perchloric -

The Structure and Stability of Simple Tri-Iodides
THE STRUCTURE AND STABILITY OF SIMPLE TRI -IODIDES by ANTHONY JOHN THOMPSON FINNEY B.Sc.(Hons.) submitted in fulfilment of the requirements for the Degree of Doctor of Philosophy UNIVERSITY OF TASMANIA HOBART OCTOBER, 1973 . r " • f (i) Frontispiece (reproduced as Plate 6 - 1, Chapter 1) - two views of a large single crystal of KI 3 .H20. The dimensions of this specimen were approximately 3.0 cm x 1.5 cm x 0.5 cm. • - - . ;or • - This thesis contains no material which has been accepted for the award of any other degree or diploma in any University, and to the best of my knowledge and belief, this thesis contains no copy or paraphrase of material previously published or written by another person, except where reference is made in the text of this thesis. Anthony John Finney Contents page Abstract (iv) Acknowledgements (vii) Chapter 1 - The Structure and Stability of Simple 1 Tri-iodides Chapter 2 - The Theoretical Basis of X-Ray Structural 32 Analysis Chapter 3 - The Crystallographic Program Suite 50 Chapter 4 - The Refinement of the Structure of NH I 94 4 3 Chapter 5 - The Solution of the Structure of RbI 115 3 Chapter 6 - The Solution of the Structure of KI 3 .1120 135 Chapter 7 Discussion of the Inter-relation of 201 Structure and Stability Bibliography 255 Appendix A - Programming Details 267 Appendix B - Density Determinations 286 Appendix C - Derivation of the Unit Cell Constants of 292 KI .H 0 3 2 Appendix D - I -3 force constant Calculation 299 Appendix E - Publications 311 ( iv) THE STRUCTURE AND STABILITY OF SIMPLE TRI-IODIDES Abstract In this work the simple tri-iodides are regarded as being those in which the crystal lattice contains only cations, tri-iodide anions and possibly solvate molecules. -

1000004316196.Pdf
(This is a sample cover image for this issue. The actual cover is not yet available at this time.) This article appeared in a journal published by Elsevier. The attached copy is furnished to the author for internal non-commercial research and education use, including for instruction at the authors institution and sharing with colleagues. Other uses, including reproduction and distribution, or selling or licensing copies, or posting to personal, institutional or third party websites are prohibited. In most cases authors are permitted to post their version of the article (e.g. in Word or Tex form) to their personal website or institutional repository. Authors requiring further information regarding Elsevier’s archiving and manuscript policies are encouraged to visit: http://www.elsevier.com/copyright Author's personal copy Fluid Phase Equilibria 336 (2012) 34–40 Contents lists available at SciVerse ScienceDirect Fluid Phase Equilibria journa l homepage: www.elsevier.com/locate/fluid Osmotic and activity coefficients for the CsF + methanol or ethanol + water ternary systems determined by potentiometric measurements ∗ ∗ Jing Tang, Lei Wang, Shu’ni Li , Quanguo Zhai, Yucheng Jiang, Mancheng Hu Key Laboratory of Macromolecular Science of Shaanxi Province, School of Chemistry and Chemical Engineering, Shaanxi Normal University, Xi’an, Shaanxi 710062, PR China a r t i c l e i n f o a b s t r a c t Article history: The thermodynamic properties of CsF in the ROH (R = methyl or ethyl) + water mixtures were determined Received 18 July 2012 using potentiometric measurements at 298.15 K with the mass fraction of ROH varying from 0.00 to 0.30. -

Chemical List
1 EXHIBIT 1 2 CHEMICAL CLASSIFICATION LIST 3 4 1. Pyrophoric Chemicals 5 1.1. Aluminum alkyls: R3Al, R2AlCl, RAlCl2 6 Examples: Et3Al, Et2AlCl, EtAlCl2, Me3Al, Diethylethoxyaluminium 7 1.2. Grignard Reagents: RMgX (R=alkyl, aryl, vinyl X=halogen) 8 1.3. Lithium Reagents: RLi (R = alkyls, aryls, vinyls) 9 Examples: Butyllithium, Isobutyllithium, sec-Butyllithium, tert-Butyllithium, 10 Ethyllithium, Isopropyllithium, Methyllithium, (Trimethylsilyl)methyllithium, 11 Phenyllithium, 2-Thienyllithium, Vinyllithium, Lithium acetylide ethylenediamine 12 complex, Lithium (trimethylsilyl)acetylide, Lithium phenylacetylide 13 1.4. Zinc Alkyl Reagents: RZnX, R2Zn 14 Examples: Et2Zn 15 1.5. Metal carbonyls: Lithium carbonyl, Nickel tetracarbonyl, Dicobalt octacarbonyl 16 1.6. Metal powders (finely divided): Bismuth, Calcium, Cobalt, Hafnium, Iron, 17 Magnesium, Titanium, Uranium, Zinc, Zirconium 18 1.7. Low Valent Metals: Titanium dichloride 19 1.8. Metal hydrides: Potassium Hydride, Sodium hydride, Lithium Aluminum Hydride, 20 Diethylaluminium hydride, Diisobutylaluminum hydride 21 1.9. Nonmetal hydrides: Arsine, Boranes, Diethylarsine, diethylphosphine, Germane, 22 Phosphine, phenylphosphine, Silane, Methanetellurol (CH3TeH) 23 1.10. Non-metal alkyls: R3B, R3P, R3As; Tributylphosphine, Dichloro(methyl)silane 24 1.11. Used hydrogenation catalysts: Raney nickel, Palladium, Platinum 25 1.12. Activated Copper fuel cell catalysts, e.g. Cu/ZnO/Al2O3 26 1.13. Finely Divided Sulfides: Iron Sulfides (FeS, FeS2, Fe3S4), and Potassium Sulfide 27 (K2S) 28 REFERRAL -

Boiling Rubidium A8 a Reactor : Coolant
UNITED STATES ATOMlC ENERGY CUMMISSiON -F - - 71013 BOILING RUBIDIUM A8 A REACTOR : COOLANT. PREPARkTION OF RUBDIUM adETAL, PHYBICAL AND 33PBER.MO~AMIcC PROFERTLES, AND COMPATIBILITY WITH INCONEL , technical Infor~ionEx?snsion, Oak Ridgs, Timnessee DISCLAIMER This report was prepared as an account of work sponsored by an agency of the United States Government. Neither the United States Government nor any agency Thereof, nor any of their employees, makes any warranty, express or implied, or assumes any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, apparatus, product, or process disclosed, or represents that its use would not infringe privately owned rights. Reference herein to any specific commercial product, process, or service by trade name, trademark, manufacturer, or otherwise does not necessarily constitute or imply its endorsement, recommendation, or favoring by the United States Government or any agency thereof. The views and opinions of authors expressed herein do not necessarily state or reflect those of the United States Government or any agency thereof. DISCLAIMER Portions of this document may be illegible in electronic image products. Images are produced from the best available original document. This mprt em~~$utrraf 2 gtwks, Pcljrt I asd Pea*t 11. *. .I. I *** .* ** . ... .. : :: . :*:. *::: /f- 8. .* .*** . e.. 0.. .* 0.. * *. 0... 0.. *I *to.. 0 *a ** . ..a . .a* .* - -8 OPSE RIDCE SCHOOL OF REACTOR TECHNOUXY ''BOI~RUBIDIUM AS A BEACTOR.COOLANT : , PREPAMTION OF RUBIDIUM METALg PHYSICAL AND THERMJDYNAMIC PROPERTIESg AND COMPATIBILI!PY WII"H INCONEX" This report cont~insinformaticg. geiierated by E. group of @$SORT students under .the leadershim df S; Reed Nixon aa part of an assigned summer project. -

WO 2016/074683 Al 19 May 2016 (19.05.2016) W P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/074683 Al 19 May 2016 (19.05.2016) W P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C12N 15/10 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/DK20 15/050343 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 11 November 2015 ( 11. 1 1.2015) KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (25) Filing Language: English PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, (26) Publication Language: English SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: PA 2014 00655 11 November 2014 ( 11. 1 1.2014) DK (84) Designated States (unless otherwise indicated, for every 62/077,933 11 November 2014 ( 11. 11.2014) US kind of regional protection available): ARIPO (BW, GH, 62/202,3 18 7 August 2015 (07.08.2015) US GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, (71) Applicant: LUNDORF PEDERSEN MATERIALS APS TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, [DK/DK]; Nordvej 16 B, Himmelev, DK-4000 Roskilde DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, (DK). -

Standard Thermodynamic Properties of Chemical
STANDARD THERMODYNAMIC PROPERTIES OF CHEMICAL SUBSTANCES ∆ ° –1 ∆ ° –1 ° –1 –1 –1 –1 Molecular fH /kJ mol fG /kJ mol S /J mol K Cp/J mol K formula Name Crys. Liq. Gas Crys. Liq. Gas Crys. Liq. Gas Crys. Liq. Gas Ac Actinium 0.0 406.0 366.0 56.5 188.1 27.2 20.8 Ag Silver 0.0 284.9 246.0 42.6 173.0 25.4 20.8 AgBr Silver(I) bromide -100.4 -96.9 107.1 52.4 AgBrO3 Silver(I) bromate -10.5 71.3 151.9 AgCl Silver(I) chloride -127.0 -109.8 96.3 50.8 AgClO3 Silver(I) chlorate -30.3 64.5 142.0 AgClO4 Silver(I) perchlorate -31.1 AgF Silver(I) fluoride -204.6 AgF2 Silver(II) fluoride -360.0 AgI Silver(I) iodide -61.8 -66.2 115.5 56.8 AgIO3 Silver(I) iodate -171.1 -93.7 149.4 102.9 AgNO3 Silver(I) nitrate -124.4 -33.4 140.9 93.1 Ag2 Disilver 410.0 358.8 257.1 37.0 Ag2CrO4 Silver(I) chromate -731.7 -641.8 217.6 142.3 Ag2O Silver(I) oxide -31.1 -11.2 121.3 65.9 Ag2O2 Silver(II) oxide -24.3 27.6 117.0 88.0 Ag2O3 Silver(III) oxide 33.9 121.4 100.0 Ag2O4S Silver(I) sulfate -715.9 -618.4 200.4 131.4 Ag2S Silver(I) sulfide (argentite) -32.6 -40.7 144.0 76.5 Al Aluminum 0.0 330.0 289.4 28.3 164.6 24.4 21.4 AlB3H12 Aluminum borohydride -16.3 13.0 145.0 147.0 289.1 379.2 194.6 AlBr Aluminum monobromide -4.0 -42.0 239.5 35.6 AlBr3 Aluminum tribromide -527.2 -425.1 180.2 100.6 AlCl Aluminum monochloride -47.7 -74.1 228.1 35.0 AlCl2 Aluminum dichloride -331.0 AlCl3 Aluminum trichloride -704.2 -583.2 -628.8 109.3 91.1 AlF Aluminum monofluoride -258.2 -283.7 215.0 31.9 AlF3 Aluminum trifluoride -1510.4 -1204.6 -1431.1 -1188.2 66.5 277.1 75.1 62.6 AlF4Na Sodium tetrafluoroaluminate -

High Purity Inorganics
High Purity Inorganics www.alfa.com INCLUDING: • Puratronic® High Purity Inorganics • Ultra Dry Anhydrous Materials • REacton® Rare Earth Products www.alfa.com Where Science Meets Service High Purity Inorganics from Alfa Aesar Known worldwide as a leading manufacturer of high purity inorganic compounds, Alfa Aesar produces thousands of distinct materials to exacting standards for research, development and production applications. Custom production and packaging services are part of our regular offering. Our brands are recognized for purity and quality and are backed up by technical and sales teams dedicated to providing the best service. This catalog contains only a selection of our wide range of high purity inorganic materials. Many more products from our full range of over 46,000 items are available in our main catalog or online at www.alfa.com. APPLICATION FOR INORGANICS High Purity Products for Crystal Growth Typically, materials are manufactured to 99.995+% purity levels (metals basis). All materials are manufactured to have suitably low chloride, nitrate, sulfate and water content. Products include: • Lutetium(III) oxide • Niobium(V) oxide • Potassium carbonate • Sodium fluoride • Thulium(III) oxide • Tungsten(VI) oxide About Us GLOBAL INVENTORY The majority of our high purity inorganic compounds and related products are available in research and development quantities from stock. We also supply most products from stock in semi-bulk or bulk quantities. Many are in regular production and are available in bulk for next day shipment. Our experience in manufacturing, sourcing and handling a wide range of products enables us to respond quickly and efficiently to your needs. CUSTOM SYNTHESIS We offer flexible custom manufacturing services with the assurance of quality and confidentiality. -

The Preparation and Identification of Rubidium
THE PREPARATION AND IDENTIFICATION OF RUBIDIUM TELLURO-MOLYBDATE AND OF CESIIDl TELLURO- MOLYBDA.TE SEP ZI 193B THE PREPARATION AlJD IDENTIFICATION or :RUBIDIUM TELLURO-MOLYBDATE AND OF CESIUM '?ELLURO-MOLYBDATE By HENRY ARTHUR CARLSON \ \ Bachelor of Science Drury College Springfield. Missouri 1936 Submitted to the Department of Chemistry Oklahoma Agricultural and Meohanica.l College In Partial Fulfillment of the Requirements For the degree of MASTER OF SCIENCE 1938 . ... ... .. .. .. ... .. ' :· ·. : : . .. .. ii S£p C"·J"··} ;.;:{ I' ' """"''· APPROVED:- \ Head~~stry 108627 iii ACKNOWLEDGMENT The author wishes to acknowledge the valuabl e advice and assistance of Dr. Sylvan R~ Wood, under whose direction this work was done. Acknowledgment is also made of the many help ful suggestions and cordial cooperation of Dr. H. M. Trimble. The author wishes to express his sincere appreciation to the Oklahoma Agricultural and Mechanical College for financial assistance in the fonn of a graduate assistantship in the Depart ment of Chemistry during the school years 1936-37 and 1937-38. iv TABLE OF CONTENTS I. Introduction------------------------------ 1 II. Materials Used-------------"--------------- 3 III. Preparation of Rubidium Telluro-molybdate---- 5 IV. Methods of Analysis------------------------ 6 Telluriur a-"---------"----------------------- 6 Molybdenum•----------------------------- 8 Rubi di um------------------"-------------... 10 \Yater of Hydration---------------------- 11 v. Calculation of: Formula---------------------- 12 VI. Preparation