Uncommon Cancers of the Small Intestine, Appendix and Colon: an Analysis of SEER 1973-2004, and Current Diagnosis and Therapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mouth Esophagus Stomach Rectum and Anus Large Intestine Small
1 Liver The liver produces bile, which aids in digestion of fats through a dissolving process known as emulsification. In this process, bile secreted into the small intestine 4 combines with large drops of liquid fat to form Healthy tiny molecular-sized spheres. Within these spheres (micelles), pancreatic enzymes can break down fat (triglycerides) into free fatty acids. Pancreas Digestion The pancreas not only regulates blood glucose 2 levels through production of insulin, but it also manufactures enzymes necessary to break complex The digestive system consists of a long tube (alimen- 5 carbohydrates down into simple sugars (sucrases), tary canal) that varies in shape and purpose as it winds proteins into individual amino acids (proteases), and its way through the body from the mouth to the anus fats into free fatty acids (lipase). These enzymes are (see diagram). The size and shape of the digestive tract secreted into the small intestine. varies in each individual (e.g., age, size, gender, and disease state). The upper part of the GI tract includes the mouth, throat (pharynx), esophagus, and stomach. The lower Gallbladder part includes the small intestine, large intestine, The gallbladder stores bile produced in the liver appendix, and rectum. While not part of the alimentary 6 and releases it into the duodenum in varying canal, the liver, pancreas, and gallbladder are all organs concentrations. that are vital to healthy digestion. 3 Small Intestine Mouth Within the small intestine, millions of tiny finger-like When food enters the mouth, chewing breaks it 4 protrusions called villi, which are covered in hair-like down and mixes it with saliva, thus beginning the first 5 protrusions called microvilli, aid in absorption of of many steps in the digestive process. -

Multiple Epithelia Are Required to Develop Teeth Deep Inside the Pharynx
Multiple epithelia are required to develop teeth deep inside the pharynx Veronika Oralováa,1, Joana Teixeira Rosaa,2, Daria Larionovaa, P. Eckhard Wittena, and Ann Huysseunea,3 aResearch Group Evolutionary Developmental Biology, Biology Department, Ghent University, B-9000 Ghent, Belgium Edited by Irma Thesleff, Institute of Biotechnology, University of Helsinki, Helsinki, Finland, and approved April 1, 2020 (received for review January 7, 2020) To explain the evolutionary origin of vertebrate teeth from closure of the gill slits (15). Consequently, previous studies have odontodes, it has been proposed that competent epithelium spread stressed the importance of gill slits for pharyngeal tooth formation into the oropharyngeal cavity via the mouth and other possible (12, 13). channels such as the gill slits [Huysseune et al., 2009, J. Anat. 214, Gill slits arise in areas where ectoderm meets endoderm. In 465–476]. Whether tooth formation deep inside the pharynx in ex- vertebrates, the endodermal epithelium of the developing pharynx tant vertebrates continues to require external epithelia has not produces a series of bilateral outpocketings, called pharyngeal been addressed so far. Using zebrafish we have previously demon- pouches, that eventually contact the skin ectoderm at corre- strated that cells derived from the periderm penetrate the oropha- sponding clefts (16). In primary aquatic osteichthyans, most ryngeal cavity via the mouth and via the endodermal pouches and pouch–cleft contacts eventually break through to create openings, connect to periderm-like cells that subsequently cover the entire or gill slits (17–19). In teleost fishes, such as the zebrafish, six endoderm-derived pharyngeal epithelium [Rosa et al., 2019, Sci. -

Immune Functions of the Vermiform Appendix
The Proceedings of the International Conference on Creationism Volume 3 Print Reference: Pages 335-342 Article 30 1994 Immune Functions of the Vermiform Appendix Frank Maas Follow this and additional works at: https://digitalcommons.cedarville.edu/icc_proceedings DigitalCommons@Cedarville provides a publication platform for fully open access journals, which means that all articles are available on the Internet to all users immediately upon publication. However, the opinions and sentiments expressed by the authors of articles published in our journals do not necessarily indicate the endorsement or reflect the views of DigitalCommons@Cedarville, the Centennial Library, or Cedarville University and its employees. The authors are solely responsible for the content of their work. Please address questions to [email protected]. Browse the contents of this volume of The Proceedings of the International Conference on Creationism. Recommended Citation Maas, Frank (1994) "Immune Functions of the Vermiform Appendix," The Proceedings of the International Conference on Creationism: Vol. 3 , Article 30. Available at: https://digitalcommons.cedarville.edu/icc_proceedings/vol3/iss1/30 IMMUNE FUNCTIONS OF THE VERMIFORM APPENDIX FRANK MAAS, M.S. 320 7TH STREET GERVAIS, OR 97026 KEYWORDS Mucosal immunology, gut-associated lymphoid tissues. immunocompetence, appendix (human and rabbit), appendectomy, neoplasm, vestigial organs. ABSTRACT The vermiform appendix Is purported to be the classic example of a vestigial organ, yet for nearly a century it has been known to be a specialized organ highly infiltrated with lymphoid tissue. This lymphoid tissue may help protect against local gut infections. As the vertebrate taxonomic scale increases, the lymphoid tissue of the large bowel tends to be concentrated In a specific region of the gut: the cecal apex or vermiform appendix. -
Appendicitis
Appendicitis National Digestive Diseases Information Clearinghouse The appendix is a small, tube-like structure abdomen. Anyone can get appendicitis, attached to the first part of the large intes- but it occurs most often between the ages tine, also called the colon. The appendix of 10 and 30. is located in the lower right portion of National Institute of the abdomen. It has no known function. Diabetes and Removal of the appendix appears to cause Causes Digestive The cause of appendicitis relates to block- and Kidney no change in digestive function. Diseases age of the inside of the appendix, known Appendicitis is an inflammation of the as the lumen. The blockage leads to NATIONAL INSTITUTES appendix. Once it starts, there is no effec- increased pressure, impaired blood flow, OF HEALTH tive medical therapy, so appendicitis is and inflammation. If the blockage is not considered a medical emergency. When treated, gangrene and rupture (breaking treated promptly, most patients recover or tearing) of the appendix can result. without difficulty. If treatment is delayed, the appendix can burst, causing infection Most commonly, feces blocks the inside and even death. Appendicitis is the most of the appendix. Also, bacterial or viral common acute surgical emergency of the infections in the digestive tract can lead to Inflamed appendix Small intestine Appendix Large intestine U.S. Department The appendix is a small, tube-like structure attached to the first part of the large intestine, also called the colon. The of Health and appendix is located in the lower right portion of the abdomen, near where the small intestine attaches to the large Human Services intestine. -

Reflux Esophagitis
Reflux Esophagitis KEY FACTS TERMINOLOGY • Caustic esophagitis • Inflammation of esophageal mucosa due to PATHOLOGY gastroesophageal (GE) reflux • Lower esophageal sphincter: Decreased tone leads to IMAGING increased reflux • Irregular ulcerated mucosa of distal esophagus • Hydrochloric acid and pepsin: Synergistic effect • Foreshortening of esophagus: Due to muscle spasm CLINICAL ISSUES • Inflammatory esophagogastric polyps: Smooth, ovoid • 15-20% of Americans commonly have heartburn due to elevations reflux; ~ 30% fail to respond to standard-dose medical • Hiatal hernia in > 95% of patients with stricture therapy ○ Probably is result, not cause, of reflux ○ Prevalence of GE reflux disease has increased sharply • Peptic stricture (1- to 4-cm length): Concentric, smooth, with obesity epidemic tapered narrowing of distal esophagus • Symptoms: Heartburn, regurgitation, angina-like pain TOP DIFFERENTIAL DIAGNOSES ○ Dysphagia, odynophagia • Scleroderma • Confirmatory testing: Manometric/ambulatory pH- monitoring techniques • Drug-induced esophagitis ○ Endoscopy, biopsy • Infectious esophagitis Imaging in Gastrointestinal Disorders: Diagnoses • Eosinophilic esophagitis (Left) Graphic shows a small type 1 (sliding) hiatal hernia ſt linked with foreshortening of the esophagus, ulceration of the mucosa, and a tapered stricture of distal esophagus. (Right) Spot film from an esophagram shows a small hiatal hernia with gastric folds ſt extending above the diaphragm. The esophagus appears shortened, presumably due to spasm of its longitudinal muscles. A stricture is present at the gastroesophageal (GE) junction, and persistent collections of barium indicate mucosal ulceration. (Left) Prone film from an esophagram shows a tight stricture ſt just above the GE junction with upstream dilation of the esophagus. The herniated stomach is pulled taut as a result of the foreshortening of the esophagus, a common and important sign of reflux esophagitis. -

Appendix B: Muscles of the Speech Production Mechanism
Appendix B: Muscles of the Speech Production Mechanism I. MUSCLES OF RESPIRATION A. MUSCLES OF INHALATION (muscles that enlarge the thoracic cavity) 1. Diaphragm Attachments: The diaphragm originates in a number of places: the lower tip of the sternum; the first 3 or 4 lumbar vertebrae and the lower borders and inner surfaces of the cartilages of ribs 7 - 12. All fibers insert into a central tendon (aponeurosis of the diaphragm). Function: Contraction of the diaphragm draws the central tendon down and forward, which enlarges the thoracic cavity vertically. It can also elevate to some extent the lower ribs. The diaphragm separates the thoracic and the abdominal cavities. 2. External Intercostals Attachments: The external intercostals run from the lip on the lower border of each rib inferiorly and medially to the upper border of the rib immediately below. Function: These muscles may have several functions. They serve to strengthen the thoracic wall so that it doesn't bulge between the ribs. They provide a checking action to counteract relaxation pressure. Because of the direction of attachment of their fibers, the external intercostals can raise the thoracic cage for inhalation. 3. Pectoralis Major Attachments: This muscle attaches on the anterior surface of the medial half of the clavicle, the sternum and costal cartilages 1-6 or 7. All fibers come together and insert at the greater tubercle of the humerus. Function: Pectoralis major is primarily an abductor of the arm. It can, however, serve as a supplemental (or compensatory) muscle of inhalation, raising the rib cage and sternum. (In other words, breathing by raising and lowering the arms!) It is mentioned here chiefly because it is encountered in the dissection. -
Appendicitis US Protocol
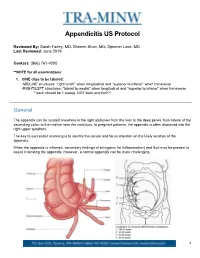
Appendicitis US Protocol Reviewed By: Sarah Farley, MD; Shireen Khan, MD; Spencer Lake, MD Last Reviewed: June 2019 Contact: (866) 761-4200 **NOTE for all examinations: 1. CINE clips to be labeled: -MIDLINE structures: “right to left” when longitudinal and “superior to inferior” when transverse -RIGHT/LEFT structures: “lateral to medial” when longitudinal and “superior to inferior” when transverse **each should be 1 sweep, NOT back and forth** General The appendix can be located anywhere in the right abdomen from the liver to the deep pelvis, from lateral of the ascending colon to the midline near the umbilicus. In pregnant patients, the appendix is often displaced into the right upper quadrant. The key to successful scanning is to identify the cecum and focus attention on the likely location of the appendix. When the appendix is inflamed, secondary findings of echogenic fat (inflammation) and fluid may be present to assist in locating the appendix. However, a normal appendix can be more challenging. 1 Strategies for finding the appendix include: 1. Review prior CT abdomen/pelvis or appendix US to see where appendix has been previously. 2. Scan in area of greatest pain (indicated by focal tenderness by 1 finger, not general pain). Label as such. 3. Localize cecum. 4. Localize ileocecal valve, if possible. Equipment: 1. Linear high frequency transducer is required, as this will best demonstrate anatomy of appendix. 2. In larger or obese patients, a curved lower frequency transducer may be used to obtain an overview and localize the cecum first. THEN, switch to the linear probe. a. When you locate the appendix, turn ON harmonics to better visualize the walls and appendiceal lumen together. -

Left Side Appendix with Appendicitis
Annals of Surgical Education ISSN: 2692-7926 Case Report Left Side Appendix with Appendicitis Bhushan STV1*, Nadaf SC1 and Anil B2 1Department of Surgery, KLE Centenary Charitable Hospital, India 2Department of Surgery, Jawaharlal Nehru Medical College, India Abstract Acute appendicitis is one of the common surgical emergencies in surgical practice. Appendicitis is basically a clinical entity and for all practical purposes appendicitis is diagnosed by good history taking, good clinical examination and needs only a few investigations to confirm. The management of an acute appendicitis is Appendicetomy under suitable anaesthesia. Whenever there are atypical clinical picture and the diagnosis is uncertain which may require special investigations including CT Scan as it was done in our case. Keywords: Appendicitis; Left sided appendix; CT scan Introduction deep seated tenderness was present in both the iliac fossae. There was no guarding or rigidity with normal bowel sounds. Other systems of Appendicitis is a common surgical condition in clinical practice, CVS, RS, and CNS were normal. Clinically he was diagnosed to have this condition is seen by General Practitioners who are the first contact Recurrent Appendicitis and was managed on the conservative lines doctors and also some patients come to surgical specialist in hospitals. with IV fluids, IV antibiotic (Taxim 1 gram IV BD, Metrogyl 500 mg Many of the practitioners who offer non-operative management in the IV BD with injection omez 40 mg IV OD along with analgesics of form of IV fluids, antibiotics and analgesics for 2 days to 3 days, often tramadol 50 mg SOS). the patients will get better, and then surgery is usually postponed till the patient gets next attack. -
![Barrett Oesophagus"[All Fields] OR "Barrett Esophagus"[Mesh Terms] OR ("Barrett"[All Fields] and "Esophagus"[All Fields]) OR "Barrett Esophagus"[All Fields])](https://docslib.b-cdn.net/cover/4619/barrett-oesophagus-all-fields-or-barrett-esophagus-mesh-terms-or-barrett-all-fields-and-esophagus-all-fields-or-barrett-esophagus-all-fields-2804619.webp)
Barrett Oesophagus"[All Fields] OR "Barrett Esophagus"[Mesh Terms] OR ("Barrett"[All Fields] and "Esophagus"[All Fields]) OR "Barrett Esophagus"[All Fields])
Appendix One – Search Strategies for BE Guidelines 1 "barrett oesophagus"[All Fields] OR "barrett esophagus"[MeSH Terms] OR ("barrett"[All Fields] AND "esophagus"[All Fields]) OR "barrett esophagus"[All Fields]) 2 epithelial[All Fields] OR ("epithelium"[MeSH Terms] OR "epithelium"[All Fields]) 3 "intestinal mucosa"[MeSH Terms] OR ("intestinal"[All Fields] AND "mucosa"[All Fields]) OR "intestinal mucosa"[All Fields]) 4 columnar[All Fields] OR "columnar lined"[All Fields]) 5 "goblet cells"[MeSH Terms] OR ("goblet"[All Fields] AND "cells"[All Fields]) OR "goblet cells"[All Fields] OR ("goblet"[All Fields] AND "cell"[All Fields]) OR "goblet cell"[All Fields]) 6 "Metaplasia"[Mesh:noexp] OR metaplasia[tw])) OR "esophagus/pathology"[Mesh Terms]) OR (dysplastic[All Fields] OR dysplasia[All Fields] OR "high grade dysplasia"[All Fields]) 7 (precancer[tw] OR pre-cancer[tw])) OR ("pre malignancy"[All Fields] OR ("precancerous conditions"[MeSH Terms] OR ("precancerous"[All Fields] AND "conditions"[All Fields]) OR "precancerous conditions"[All Fields] OR "premalignant"[All Fields]) 8 "disease progression"[MeSH Terms] OR ("disease"[All Fields] AND "progression"[All Fields]) OR "disease progression"[All Fields]) 9 ("adenocarcinoma"[MeSH Terms] OR "adenocarcinoma"[All Fields]) 10 Combine results of sets 2-9 using OR 11 ("oesophagus"[All Fields] OR "esophagus"[MeSH Terms] OR "esophagus"[All Fields) 12 Combine results of 10 with 11 using AND 13 Combine results of set 1 with set 12 using OR 14 Combine results of 13 with ("animals"[MeSH Terms] AND "humans"[MeSH Terms]) 15 Exclude animals by combining results of 14 with “animals”[MeSH Terms] using NOT 16 Limit 13 to English[lang] As of May 23, 2014, the total number of citations retrieved using this search was 15,342. -
Caring for Myself After Laparoscopic Appendectomy
Caring for myself after Laparoscopic Appendectomy What is Laparoscopy Appendectomy? © NIDDK Laparoscopy appendectomy is a surgery to treat appendicitis – infection of the appendix. During laparoscopic surgery, surgeons use several smaller incisions and special surgical tools that they feed through the incisions to remove your appendix. Laparoscopic surgery leads to fewer complications, such as hospital-related infections, and has a shorter recovery time. How will care for myself after the surgery? How will I care for my incision? • You may shower your incisions once home. • Gently wash incisions and pat dry. Leave open to the air and dry. • Avoid powders or creams. • Do not take tub baths or hot tubs. • Do not swim until the incisions are completely healed. • Wear loose comfortable clothing. Tight fitting clothing may irritate the skin around your incision sites. • If steri strips are present, these will fall off in about 1-2 weeks. Do not pull them off earlier. How will I manage my pain at home? The best strategy for controlling your pain after surgery is around the clock pain control with Tylenol (acetaminophen) and Motrin (ibuprofen or Advil). “Around the clock” means taking medications on a set schedule day and night. Alternating these medications allows you to maximize your pain control. In addition to Tylenol and Motrin, you can use heating pads or ice packs on your incisions to help reduce your pain. Minimally Invasive Surgery - 1 - How will I alternate over-the-counter pain medication? You will take a dose of pain medication every three hours: • Start by taking 650 mg of Tylenol (2 pills of 325 mg) • 3 hours later take 600 mg of Motrin (3 pills of 200 mg) • 3 hours later take 650 mg of Tylenol • 3 hours after that take 600 mg of Motrin. -

Axis Scientific Human Digestive System (1/2 Size)
Axis Scientific Human Digestive System (1/2 Size) A-105865 48. Body of Pancreas 27. Transverse Colon 02. Hard Palate 47. Pancreatic Notch 07. Nasopharynx 05. Tooth 01. Lower Lip F. Large Intestine 06. Tongue 21. Jejunum A. Oral Cavity 09. Pharyngeal Tonsil 03. Soft Palate 08. Opening to Auditory Tube 28. E. Small Intestine 04. Uvula 11. Palatine Tonsil Descending Colon 40. Gallbladder 37. Round Ligament of Liver 22. Ileum 38. Quadrate Lobe 44. Proper Hepatic Artery 42. Common Hepatic Duct 45. Hepatic Portal Vein C. Esophagus 15. Fundus of Stomach 30. Rectum 29. Sigmoid Colon 13. Cardia 26. Ascending Colon 39. Caudate Lobe 24. Ileocecal Valve 35. Left Lobe of 16. Body of 34. Falciform Liver Stomach 41. Cystic Duct Ligament 36. Right Lobe of Liver G. Liver 31. Anal Canal 14. Pylorus D. Stomach 33. External 18. Duodenum Anal Sphincter Muscle 17. Pyloric Antrum 46. Head of Pancreas 23. Cecum 51. Accessory Pancreatic Duct 49. Tail of 50. Pancreatic 25. Vermiform 20. Minor Duodenal Papilla H. Pancreas Duct Pancreas Appendix 19. Major Duodenal Papilla 32. Internal Anal Sphincter Muscle 01. Lower Lip 20. Minor Duodenal Papilla 39. Caudate Lobe 02. Hard Palate 21. Jejunum 40. Gallbladder 03. Soft Palate 22. Ileum 41. Cystic Duct 42. Common Hepatic Duct 04. Uvula 23. Cecum 43. Common Bile Duct 05. Tooth 24. Ileocecal Valve 44. Proper Hepatic Artery 06. Tongue 25. Vermiform Appendix 45. Hepatic Portal Vein 07. Nasopharynx 26. Ascending Colon 46. Head of Pancreas 08. Opening to Auditory Tube 27. Transverse Colon 47. Pancreatic Notch 09. Pharyngeal Tonsil 28. -
Gallbladder-Appendicular Fistula
Gastro Med Res Gastroenterology Copyright © Mikheev IO CRIMSON PUBLISHERS C Wings to the Research Medicine & Research ISSN 2637-7632 Case Report Rare Complication of Gallstone Disease:Gallbladder -Appendicular Fistula: Clinical Case Report Yareshko NO, Mikheev IO*, Shabanov NA, Barska KS and Kanaki AV Ukraine *Corresponding author: Mikheev IO, Ukraine Submission: February 02, 2019; Published: February 07, 2019 Introduction malignant tumor of the gallbladder, pancreas, chronic pancreatitis. Gallstone disease is one of the most common diseases detected, Established more accurate clinical and anamnestic characteristics according to the literature, in 10-15% of the population [1-5]. According to the Center for Medical Statistics of the Ministry of of biliary tract fistulas: gallstone disease in history, weight loss, increase in the number of patients with Gallstone disease. Among jaundice, recurrent chills, bouts of pain up to three to four times a Health of Ukraine, in recent years there has been a significant rare complications cholelithiasis are isolated external biliary year, discomfort in the right hypochondrium [3,4]. The peculiarity of the clinical course of biliodigestive fistulas is intermittent symptom biliary system, as well as loss of body weight, signs of dyspepsy, and of severe cholangitis due to the reflux of intestinal contents in the fistula, internal or cholecystodigestive fistulas, torakobiliary and syndrome, cholelithiasis small bowel obstruction, but also other bronchobiliary fistulas, cholecystocholedoheal fistula or Mirizzi abundant liquid stool. Given the prevalence of gallstones and the danger of this, although rare, but it’s serious complication, such as types of bile fistula and micro or “large” choledocholithiasis, the formation of biliodigestive fistula, we give the following clinical “wrinkled” gallbladder, calcification of the gallbladder [6].