Parenteral Nutrition and Lipids
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Novel Lipid Screening Platform That Provides a Complete Solution for Lipidomics Research
A Novel Lipid Screening Platform that Provides a Complete Solution for Lipidomics Research The Lipidyzer™ Platform, powered by Metabolon® Baljit K Ubhi1, Alex Conner1, Eva Duchoslav3, Annie Evans1, Richard Robinson1, Paul RS Baker4 and Steve Watkins1 1SCIEX, CA, USA, 2Metabolon, USA, 3SCIEX, Ontario, Canada and 4SCIEX, MA, USA INTRODUCTION MATERIALS AND METHODS A major challenge in lipid analysis is the many isobaric Applying the kit for simplified sample extraction and preparation, interferences present in highly complex samples that confound a serum matrix was used following the protocols provided. A identification and accurate quantitation. This problem, coupled QTRAP® System with SelexION® DMS Technology (SCIEX) with complicated sample preparation techniques and data was used for targeted profiling of over a thousand lipid species analysis, highlights the need for a complete solution that from 13 different lipid classes (Figure 2) allowing for addresses these difficulties and provides a simplified method for comprehensive coverage. Two methods were used covering analysis. A novel lipidomics platform was developed that thirteen lipid classes using a flow injection analysis (FIA); one includes simplified sample preparation, automated methods, and injection with SelexION® Technology ON and another with the streamlined data processing techniques that enable facile, SelexION® Technology turned OFF. The lipid molecular species quantitative lipid analysis. Herein, serum samples were analyzed were measured using MRM and positive/negative switching. quantitatively using a unique internal standard labeling protocol, Positive ion mode detected the following lipid classes – a novel selectivity tool (differential mobility spectrometry; DMS) SM/DAG/CE/CER/TAG. Negative ion mode detected the and novel lipid data analysis software. -

Blood Fats Explained
Blood Fats Explained HEART UK – The Cholesterol Charity providing expert support, education and influence 2 | Fats in the blood At risk of cardiovascular disease? | 3 Fats in the blood At risk of cardiovascular disease? Fats that circulate in the blood are called lipids. Very low density lipoproteins (VLDL) transport Cardiovascular disease (CVD) is the medical Blood pressure is a measure of the resistance Cholesterol and triglycerides are both lipids. mainly triglycerides made by the liver to where name for circulatory diseases such as coronary to the flow of blood around your body. It is They have essential roles in the body. In excess they are either used to fuel our muscles or stored heart disease (CHD), stroke, mini stroke (transient measured in millimetres of mercury (mmHg). Your they are harmful. for later use. ischaemic attack or TIA), angina and peripheral doctor or nurse will measure both your systolic vascular disease (PVD). You are more likely to (upper figure) and diastolic (lower figure) blood Cholesterol is needed to build cell walls and Low density lipoproteins (LDL) carry most of the develop CVD the more risk factors you have. pressure. About a third of adults have high blood to make hormones and vitamin D. Some of our cholesterol in our body from the liver to the cells pressure. If untreated it increases the risk of cholesterol comes from the food we eat; but most that need it. The cholesterol that is carried on LDLs There are two types of risk factors: heart attack and stroke. High blood pressure is is made in the liver. -

Fatty Acids: Essential…Therapeutic
Volume 3, No.2 May/June 2000 A CONCISE UPDATE OF IMPORTANT ISSUES CONCERNING NATURAL HEALTH INGREDIENTS Written and Edited By: Thomas G. Guilliams Ph.D. FATTY ACIDS: Essential...Therapeutic Few things have been as confusing to both patient and health care provider as the issue of fats and oils. Of all the essential nutrients required for optimal health, fatty acids have not only been forgotten they have been considered hazardous. Health has somehow been equated with “low-fat” or “fat-free” for so long, to suggest that fats could be essential or even therapeutic is to risk credibility. We hope to give a view of fats that is both balanced and scientific. This review will cover the basics of most fats that will be encountered in dietary or supplemental protocols. Recommendations to view essential fatty acids in a similar fashion as essential vitamins and minerals will be combined with therapeutic protocols for conditions ranging from cardiovascular disease, skin conditions, diabetes, nerve related disorders, retinal disorders and more. A complete restoration of health cannot be accomplished until there is a restoration of fatty acid nutritional information among health care professionals and their patients. Fats- What are they? Dietary fats come to us from a variety of sources, but primarily in the form of triglycerides. That is, three fatty acid molecules connected by a glycerol backbone (see fatty acid primer page 3 for diagram). These fatty acids are then used as energy by our cells or modified into phospholipids to be used as cell or organelle membranes. Some fatty acids are used in lipoprotein molecules to shuttle cholesterol and fats to and from cells, and fats may also be stored for later use. -

Essential Fatty Acid Formulas — — — Liquids
To contact Designs for Health, please call us at (800) 847-8302, or visit us on the web at at (800)847-8302,or visit usontheweb please call Health, usat Designs for contact To These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cureor prevent any disease. treat, These products arenotintended todiagnose, Administration. and Drug These statements havenotbeen evaluatedbytheFood Product Comparison Chart OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ Ultra Ultra Lemon Drop Synergy TG1000 Hi-Po Ultra Marine Liquid with D3, K1 & K2 DHA Smoothie Unique omega-3-6-7-9 High potency DHA/EPA Great for children and fatty acid formula High potency EPA/DHA formula with flexible Highest potency High potency EPA/ Added D3, K1, K2 for Maintenance and High potency DHA the elderly who prefer offers balanced doses in a single softgel for dosing; ideal for EPA/DHA for most DHA for aggressive cardiovascular & bone general omega-3 formula for therapeutic not to take pills, higher of EPA, DHA, GLA, optimal compliance of children, the elderly & aggressive applications applications and immune support dosing DHA applications dosing is easy with palmitoleic acid, and therapeutic dosing those who prefer not to liquids oleic acid swallow pills Serving Size 2 Softgels 1 Softgel 2 Softgels 2 Softgels 2 Softgels 2 Softgels 1 Softgel 11 g (2 tsp.) 5ml (1 tsp.) EPA (n-3) 270 mg 662 mg 1000 mg 600 mg 600 mg 320 mg 110 mg 1100 mg 725 mg DHA (n-3) 180 mg 250 mg 500 mg 400 mg 400 mg 200 mg 500 mg 720 mg 450 mg Other EFAs 645 mg 88 mg — 200 mg 200 mg 80 mg — 230 mg 180 mg Vitamin D3 — — — — 1000 IU — — — — Vitamin K1/K2 — — — — 500 mcg/25 mcg — — — — www.designsforhealth.com Lipase Yes Yes Yes Yes Yes Yes Yes — — For EveryPatient Essential FattyAcidFormulas SPECIAL FORMULAS The Impact of Fatty Acids Fatty acids have a number of fundamental benefits for human health. -

Polyunsaturated Fatty Acids and Their Potential Therapeutic Role in Cardiovascular System Disorders—A Review
nutrients Review Polyunsaturated Fatty Acids and Their Potential Therapeutic Role in Cardiovascular System Disorders—A Review Ewa Sokoła-Wysocza ´nska 1, Tomasz Wysocza ´nski 2, Jolanta Wagner 2,3, Katarzyna Czyz˙ 4,*, Robert Bodkowski 4, Stanisław Lochy ´nski 3,5 and Bozena˙ Patkowska-Sokoła 4 1 The Lumina Cordis Foundation, Szymanowskiego Street 2/a, 51-609 Wroclaw, Poland; [email protected] 2 FLC Pharma Ltd., Wroclaw Technology Park Muchoborska Street 18, 54-424 Wroclaw, Poland; [email protected] (T.W.); jolanta.pekala@flcpharma.com (J.W.) 3 Department of Bioorganic Chemistry, Faculty of Chemistry, University of Technology, Wybrzeze Wyspianskiego Street 27, 50-370 Wroclaw, Poland; [email protected] 4 Institute of Animal Breeding, Faculty of Biology and Animal Sciences, Wroclaw University of Environmental and Life Sciences, Chelmonskiego Street 38c, 50-001 Wroclaw, Poland; [email protected] (R.B.); [email protected] (B.P.-S.) 5 Institute of Cosmetology, Wroclaw College of Physiotherapy, Kosciuszki 4 Street, 50-038 Wroclaw, Poland * Correspondence: [email protected]; Tel.: +48-71-320-5781 Received: 23 August 2018; Accepted: 19 October 2018; Published: 21 October 2018 Abstract: Cardiovascular diseases are described as the leading cause of morbidity and mortality in modern societies. Therefore, the importance of cardiovascular diseases prevention is widely reflected in the increasing number of reports on the topic among the key scientific research efforts of the recent period. The importance of essential fatty acids (EFAs) has been recognized in the fields of cardiac science and cardiac medicine, with the significant effects of various fatty acids having been confirmed by experimental studies. -

Fats and Fatty Acid in Human Nutrition
ISSN 0254-4725 91 FAO Fats and fatty acids FOOD AND NUTRITION PAPER in human nutrition Report of an expert consultation 91 Fats and fatty acids in human nutrition − Report of an expert consultation Knowledge of the role of fatty acids in determining health and nutritional well-being has expanded dramatically in the past 15 years. In November 2008, an international consultation of experts was convened to consider recent scientific developments, particularly with respect to the role of fatty acids in neonatal and infant growth and development, health maintenance, the prevention of cardiovascular disease, diabetes, cancers and age-related functional decline. This report will be a useful reference for nutrition scientists, medical researchers, designers of public health interventions and food producers. ISBN 978-92-5-106733-8 ISSN 0254-4725 9 7 8 9 2 5 1 0 6 7 3 3 8 Food and Agriculture I1953E/1/11.10 Organization of FAO the United Nations FAO Fats and fatty acids FOOD AND NUTRITION in human nutrition PAPER Report of an expert consultation 91 10 − 14 November 2008 Geneva FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS Rome, 2010 The designations employed and the presentation of material in this information product do not imply the expression of any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations (FAO) concerning the legal or development status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or products of manufacturers, whether or not these have been patented, does not imply that these have been endorsed or recommended by FAO in preference to others of a similar nature that are not mentioned. -

Seasonal Growth and Lipid Storage of the Circumgiobal, Subantarctic Copepod, Neocalanus Tonsus (Brady)
Deep-Sea Research, Vol. 36, No. 9, pp, 1309-1326, 1989. 0198-0149/89$3.00 + 0.00 Printed in Great Britain. ~) 1989 PergamonPress pie. Seasonal growth and lipid storage of the circumgiobal, subantarctic copepod, Neocalanus tonsus (Brady) MARK D. OHMAN,* JANET M. BRADFORDt and JOHN B. JILLETr~ (Received 20 January 1988; in revised form 14 April 1989; accepted 24 April 1989) Abstraet--Neocalanus tonsus (Brady) was sampled between October 1984 and September 1985 in the upper 1000 m of the water column off southeastern New Zealand. The apparent spring growth increment of copepodid stage V (CV) differed depending upon the constituent con- sidered: dry mass increased 208 Ixg, carbon 162 Ixg, wax esters 143 Itg, but nitrogen only 5 ltg. Sterols and phospholipids remained relatively constant over this interval. Wax esters were consistently the dominant lipid class present in CV's, increasing seasonally from 57 to 90% of total lipids. From spring to winter, total lipid content of CV's increased from 22 to 49% of dry mass. Nitrogen declined from 10.9 to 5.4% of CV dry mass as storage compounds (wax esters) increased in importance relative to structural compounds. Egg lipids were 66% phospholipids. Upon first appearance of males and females in deep water in winter, lipid content and composition did not differ from co-occurring CV's, confirming the importance of lipids rather than particulate food as an energy source for deep winter reproduction of this species. Despite contrasting life histories, N. tonsus and subarctic Pacific Neocalanus plumchrus CV's share high lipid content, a predominance of wax esters over triacylglycerols as storage lipids, and similar wax ester fatty acid and fatty alcohol composition. -

Fatty Acids: Structures and Introductory Article Properties Article Contents
Fatty Acids: Structures and Introductory article Properties Article Contents . Introduction Arild C Rustan, University of Oslo, Oslo, Norway . Overview of Fatty Acid Structure . Major Fatty Acids Christian A Drevon, University of Oslo, Oslo, Norway . Metabolism of Fatty Acids . Properties of Fatty Acids Fatty acids play a key role in metabolism: as a metabolic fuel, as a necessary component of . Requirements for and Uses of Fatty Acids in Human all membranes, and as a gene regulator. In addition, fatty acids have a number of industrial Nutrition uses. Uses of Fatty Acids in the Pharmaceutical/Personal Hygiene Industries Introduction doi: 10.1038/npg.els.0003894 Fatty acids, both free and as part of complex lipids, play a number of key roles in metabolism – major metabolic fuel (storage and transport of energy), as essential components subsequent one the b carbon. The letter n is also often used of all membranes, and as gene regulators (Table 1). In ad- instead of the Greek o to indicate the position of the double dition, dietary lipids provide polyunsaturated fatty acids bond closest to the methyl end. The systematic nomencla- (PUFAs) that are precursors of powerful locally acting ture for fatty acids may also indicate the location of double metabolites, i.e. the eicosanoids. As part of complex lipids, bonds with reference to the carboxyl group (D). Figure 2 fatty acids are also important for thermal and electrical outlines the structures of different types of naturally insulation, and for mechanical protection. Moreover, free occurring fatty acids. fatty acids and their salts may function as detergents and soaps owing to their amphipathic properties and the for- Saturated fatty acids mation of micelles. -
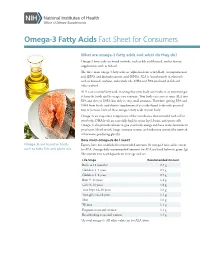
Omega-3 Fatty Acids Fact Sheet for Consumers
Omega-3 Fatty Acids Fact Sheet for Consumers What are omega-3 fatty acids and what do they do? Omega-3 fatty acids are found in foods, such as fish and flaxseed, and in dietary supplements, such as fish oil. The three main omega-3 fatty acids are alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). ALA is found mainly in plant oils such as flaxseed, soybean, and canola oils. DHA and EPA are found in fish and other seafood. ALA is an essential fatty acid, meaning that your body can’t make it, so you must get it from the foods and beverages you consume. Your body can convert some ALA into EPA and then to DHA, but only in very small amounts. Therefore, getting EPA and DHA from foods (and dietary supplements if you take them) is the only practical way to increase levels of these omega-3 fatty acids in your body. Omega-3s are important components of the membranes that surround each cell in your body. DHA levels are especially high in retina (eye), brain, and sperm cells. Omega-3s also provide calories to give your body energy and have many functions in your heart, blood vessels, lungs, immune system, and endocrine system (the network of hormone-producing glands). How much omega-3s do I need? Omega-3s are found in foods Experts have not established recommended amounts for omega-3 fatty acids, except such as fatty fish and plant oils. for ALA. Average daily recommended amounts for ALA are listed below in grams (g). -

Lipid–Protein and Protein–Protein Interactions in the Pulmonary Surfactant System and Their Role in Lung Homeostasis
International Journal of Molecular Sciences Review Lipid–Protein and Protein–Protein Interactions in the Pulmonary Surfactant System and Their Role in Lung Homeostasis Olga Cañadas 1,2,Bárbara Olmeda 1,2, Alejandro Alonso 1,2 and Jesús Pérez-Gil 1,2,* 1 Departament of Biochemistry and Molecular Biology, Faculty of Biology, Complutense University, 28040 Madrid, Spain; [email protected] (O.C.); [email protected] (B.O.); [email protected] (A.A.) 2 Research Institut “Hospital Doce de Octubre (imasdoce)”, 28040 Madrid, Spain * Correspondence: [email protected]; Tel.: +34-913944994 Received: 9 May 2020; Accepted: 22 May 2020; Published: 25 May 2020 Abstract: Pulmonary surfactant is a lipid/protein complex synthesized by the alveolar epithelium and secreted into the airspaces, where it coats and protects the large respiratory air–liquid interface. Surfactant, assembled as a complex network of membranous structures, integrates elements in charge of reducing surface tension to a minimum along the breathing cycle, thus maintaining a large surface open to gas exchange and also protecting the lung and the body from the entrance of a myriad of potentially pathogenic entities. Different molecules in the surfactant establish a multivalent crosstalk with the epithelium, the immune system and the lung microbiota, constituting a crucial platform to sustain homeostasis, under health and disease. This review summarizes some of the most important molecules and interactions within lung surfactant and how multiple lipid–protein and protein–protein interactions contribute to the proper maintenance of an operative respiratory surface. Keywords: pulmonary surfactant film; surfactant metabolism; surface tension; respiratory air–liquid interface; inflammation; antimicrobial activity; apoptosis; efferocytosis; tissue repair 1. -

Nutrition Bytes
UCLA Nutrition Bytes Title Theories Presented in The Zone Permalink https://escholarship.org/uc/item/9pg2j7wk Journal Nutrition Bytes, 3(1) ISSN 1548-4327 Author Chang, Jeannie Publication Date 1997 Peer reviewed eScholarship.org Powered by the California Digital Library University of California "Easy -to -follow" diet plans appear each year to convince overweight Americans that there is finally a way to lose weight permanently. Barry Sears and Bill Lawren’s book, The Zone, is no exception; in fact, Sears’ book cover advertises that it is "a dietary road map to lose weight permanently, reset your genetic code, prevent disease, achieve maximum physical performance, [and] enhance mental productivity." But is this realistic? Can a diet really accomplish all of those tasks? After numerous searches through several databases, only two journal articles analyzing this diet plan surfaced, both warning readers about the misinformation contained in the book. There are definitely problems with Sears’ diet; for example, his daily caloric intake recommendation is dangerously low. Tufts University Diet and Nutrition Letter stated that they believed "[Sears was] confusing the near -euphoria he promises from following the Zone diet with lightheadedness from hunger" (3). Dr. Zamenhof, Associate Professor of Biological Ch emistry at UCLA said that it was probably due to an increased release of endorphins, enkephalins, and catecholamines. In addition, the information he provides regarding carbohydrate and fat metabolism, as well as insulin and glucagon secretion, are wrong. However, Sears also says that there is a direct relationship between insulin and glucagon with the synthesis of "good" eicosanoids (prostaglandin E1 and prostaglandin I2 and "bad" eicosanoids (prostaglandin E2, thromboxanes, and leukotrienes). -

Soluble Surfactant and Nanoparticle Effects on Lipid Monolayer Assembly and Stability
Soluble Surfactant and Nanoparticle Effects on Lipid Monolayer Assembly and Stability Dissertation Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Matthew D. Nilsen, B.S., M.Sc. Graduate Program in Chemical Engineering The Ohio State University 2010 Dissertation Committee: Dr. James F. Rathman, Advisor Dr. L. James Lee Dr. Isamu Kusaka c Copyright by Matthew D. Nilsen 2010 Abstract The study of self-assembly dynamics that lead to ultra-thin films at an interface remains a very active research topic because of the ability to generate interesting and useful structures that can perform specific tasks such as aiding in magnetic separa- tions, acting as two-dimensional biosensors and the modification of surfaces without changing their morphology. In some cases this is critical to surface functionality. This area is also important because it may ultimately yield simple screening techniques for novel surfactants and nanoparticle species before they are introduced onto the market, as is already happening. In the work presented here we studied the assembly dynamics of the insoluble lipid DPPC, common to most mammalian cell lines, in the presence of soluble surfactant and nanoparticle species. Preliminarily, we investigated the anomalous behavior of soluble surfactants at the air/water interface as an exten- sion to work done previously and then used these results in an attempt to explain the behavior of the combined surfactant/lipid monolayer under dynamic and static conditions. Separately, we performed nanoparticle dynamics studies for a commer- cially available product and for particles created in-house before performing similar statics/dynamics work on the combined nanoparticle/lipid monolayer.