Polyunsaturated Fatty Acids and Their Potential Therapeutic Role in Cardiovascular System Disorders—A Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Role of Short Chain Fatty Acids in Appetite Regulation and Energy Homeostasis
OPEN International Journal of Obesity (2015) 39, 1331–1338 © 2015 Macmillan Publishers Limited All rights reserved 0307-0565/15 www.nature.com/ijo REVIEW The role of short chain fatty acids in appetite regulation and energy homeostasis CS Byrne1, ES Chambers1, DJ Morrison2 and G Frost1 Over the last 20 years there has been an increasing interest in the influence of the gastrointestinal tract on appetite regulation. Much of the focus has been on the neuronal and hormonal relationship between the gastrointestinal tract and the brain. There is now mounting evidence that the colonic microbiota and their metabolic activity have a significant role in energy homeostasis. The supply of substrate to the colonic microbiota has a major impact on the microbial population and the metabolites they produce, particularly short chain fatty acids (SCFAs). SCFAs are produced when non-digestible carbohydrates, namely dietary fibres and resistant starch, undergo fermentation by the colonic microbiota. Both the consumption of fermentable carbohydrates and the administration of SCFAs have been reported to result in a wide range of health benefits including improvements in body composition, glucose homeostasis, blood lipid profiles and reduced body weight and colon cancer risk. However, published studies tend to report the effects that fermentable carbohydrates and SCFAs have on specific tissues and metabolic processes, and fail to explain how these local effects translate into systemic effects and the mitigation of disease risk. Moreover, studies tend to investigate SCFAs collectively and neglect to report the effects associated with individual SCFAs. Here, we bring together the recent evidence and suggest an overarching model for the effects of SCFAs on one of their beneficial aspects: appetite regulation and energy homeostasis. -

Alpha-Linolenic Acid COMMON NAME: ALA Omega-3
Supplements to help manage total cholesterol, LDL and HDL Alpha-Linolenic Acid COMMON NAME: ALA omega-3 SCIENTIFIC NAME: ALA, 18:3 n-3 RECOMMENDED WITH CAUTION LEVELS OF EVIDENCE 1 2 Recommended: Recommended with Caution: Several well-designed studies in humans Preliminary studies suggest some benefit. have shown positive benefit. Our team is Future trials are needed before we can confident about its therapeutic potential. make a stronger recommendation. 3 4 Not Recommended - Evidence: Not Recommended - High Risk: Our team does not recommend this Our team recommends against using this product because clinical trials to date product because clinical trials to date suggest little or no benefit. suggest substantial risk greater than the benefit. Evaluated Benefits Reduces total cholesterol, LDL cholesterol, and triglycerides Supported by P&G HeartHealth-RecommendedWithCaution.indd 1 6/27/2017 9:41:39 AM Source Dietary alpha-linolenic acid is found primarily in vegetable oils, such as flaxseed (linseed) oil and canola (rapeseed) oil. Walnuts are the only edible nuts with significant amounts of alpha-linolenic acid. Alpha-linolenic acid is found in smaller amounts in green leafy vegetables and chocolate. ALA is an essential fatty acid that must be consumed for you to have any in your body. Indications/Population Lowering of LDL cholesterol/hyperlipidemia and metabolic syndrome Mechanism of Action It may increase insulin sensitivity directly, or decrease hepatic fat storage. Some (2–15%) is convert- ed to eicosapentaenoic acid (EPA), and less (<2%) to docosahexaenoic acid (DHA). The effects of ALA on serum lipids were, for the most part, not consistent with that reported for the very long-chain omega-3 fatty acids, EPA and DHA. -

Fatty Acids: Essential…Therapeutic
Volume 3, No.2 May/June 2000 A CONCISE UPDATE OF IMPORTANT ISSUES CONCERNING NATURAL HEALTH INGREDIENTS Written and Edited By: Thomas G. Guilliams Ph.D. FATTY ACIDS: Essential...Therapeutic Few things have been as confusing to both patient and health care provider as the issue of fats and oils. Of all the essential nutrients required for optimal health, fatty acids have not only been forgotten they have been considered hazardous. Health has somehow been equated with “low-fat” or “fat-free” for so long, to suggest that fats could be essential or even therapeutic is to risk credibility. We hope to give a view of fats that is both balanced and scientific. This review will cover the basics of most fats that will be encountered in dietary or supplemental protocols. Recommendations to view essential fatty acids in a similar fashion as essential vitamins and minerals will be combined with therapeutic protocols for conditions ranging from cardiovascular disease, skin conditions, diabetes, nerve related disorders, retinal disorders and more. A complete restoration of health cannot be accomplished until there is a restoration of fatty acid nutritional information among health care professionals and their patients. Fats- What are they? Dietary fats come to us from a variety of sources, but primarily in the form of triglycerides. That is, three fatty acid molecules connected by a glycerol backbone (see fatty acid primer page 3 for diagram). These fatty acids are then used as energy by our cells or modified into phospholipids to be used as cell or organelle membranes. Some fatty acids are used in lipoprotein molecules to shuttle cholesterol and fats to and from cells, and fats may also be stored for later use. -

Essential Fatty Acid Formulas — — — Liquids
To contact Designs for Health, please call us at (800) 847-8302, or visit us on the web at at (800)847-8302,or visit usontheweb please call Health, usat Designs for contact To These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cureor prevent any disease. treat, These products arenotintended todiagnose, Administration. and Drug These statements havenotbeen evaluatedbytheFood Product Comparison Chart OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ Ultra Ultra Lemon Drop Synergy TG1000 Hi-Po Ultra Marine Liquid with D3, K1 & K2 DHA Smoothie Unique omega-3-6-7-9 High potency DHA/EPA Great for children and fatty acid formula High potency EPA/DHA formula with flexible Highest potency High potency EPA/ Added D3, K1, K2 for Maintenance and High potency DHA the elderly who prefer offers balanced doses in a single softgel for dosing; ideal for EPA/DHA for most DHA for aggressive cardiovascular & bone general omega-3 formula for therapeutic not to take pills, higher of EPA, DHA, GLA, optimal compliance of children, the elderly & aggressive applications applications and immune support dosing DHA applications dosing is easy with palmitoleic acid, and therapeutic dosing those who prefer not to liquids oleic acid swallow pills Serving Size 2 Softgels 1 Softgel 2 Softgels 2 Softgels 2 Softgels 2 Softgels 1 Softgel 11 g (2 tsp.) 5ml (1 tsp.) EPA (n-3) 270 mg 662 mg 1000 mg 600 mg 600 mg 320 mg 110 mg 1100 mg 725 mg DHA (n-3) 180 mg 250 mg 500 mg 400 mg 400 mg 200 mg 500 mg 720 mg 450 mg Other EFAs 645 mg 88 mg — 200 mg 200 mg 80 mg — 230 mg 180 mg Vitamin D3 — — — — 1000 IU — — — — Vitamin K1/K2 — — — — 500 mcg/25 mcg — — — — www.designsforhealth.com Lipase Yes Yes Yes Yes Yes Yes Yes — — For EveryPatient Essential FattyAcidFormulas SPECIAL FORMULAS The Impact of Fatty Acids Fatty acids have a number of fundamental benefits for human health. -

Fatty Acid Biosynthesis
BI/CH 422/622 ANABOLISM OUTLINE: Photosynthesis Carbon Assimilation – Calvin Cycle Carbohydrate Biosynthesis in Animals Gluconeogenesis Glycogen Synthesis Pentose-Phosphate Pathway Regulation of Carbohydrate Metabolism Anaplerotic reactions Biosynthesis of Fatty Acids and Lipids Fatty Acids contrasts Diversification of fatty acids location & transport Eicosanoids Synthesis Prostaglandins and Thromboxane acetyl-CoA carboxylase Triacylglycerides fatty acid synthase ACP priming Membrane lipids 4 steps Glycerophospholipids Control of fatty acid metabolism Sphingolipids Isoprene lipids: Cholesterol ANABOLISM II: Biosynthesis of Fatty Acids & Lipids 1 ANABOLISM II: Biosynthesis of Fatty Acids & Lipids 1. Biosynthesis of fatty acids 2. Regulation of fatty acid degradation and synthesis 3. Assembly of fatty acids into triacylglycerol and phospholipids 4. Metabolism of isoprenes a. Ketone bodies and Isoprene biosynthesis b. Isoprene polymerization i. Cholesterol ii. Steroids & other molecules iii. Regulation iv. Role of cholesterol in human disease ANABOLISM II: Biosynthesis of Fatty Acids & Lipids Lipid Fat Biosynthesis Catabolism Fatty Acid Fatty Acid Degradation Synthesis Ketone body Isoprene Utilization Biosynthesis 2 Catabolism Fatty Acid Biosynthesis Anabolism • Contrast with Sugars – Lipids have have hydro-carbons not carbo-hydrates – more reduced=more energy – Long-term storage vs short-term storage – Lipids are essential for structure in ALL organisms: membrane phospholipids • Catabolism of fatty acids –produces acetyl-CoA –produces reducing -

Fruits of the Pitahaya Hylocereus Undatus and H. Ocamponis
Journal of Applied Botany and Food Quality 93, 197 - 203 (2020), DOI:10.5073/JABFQ.2020.093.024 1Instituto de Horticultura, Departamento de Fitotecnia. Universidad Autónoma Chapingo, Estado de Mexico 2Instituto de Alimentos, Departmento de Ingenieria Agroindustrial. Universidad Autónoma Chapingo, Estado de Mexico Fruits of the pitahaya Hylocereus undatus and H. ocamponis: nutritional components and antioxidants Lyzbeth Hernández-Ramos1, María del Rosario García-Mateos1*, Ana María Castillo-González1, Carmen Ybarra-Moncada2, Raúl Nieto-Ángel1 (Submitted: May 2, 2020; Accepted: September 15, 2020) Summary epicarp of bracts. In addition, it is important to point out that “pitaya” The pitahaya (Hylocereus spp.) is a cactus native to America. and “pitahaya” have been used incorrectly as synonyms (IBRAHIM Despite the great diversity of species located in Mexico, there are et al., 2018; LE BELLEC et al., 2006). “Pitaya” corresponds to the few studies on the nutritional and nutraceutical value of its exotic genus Stenocereus (QUIROZ-GONZÁLEZ et al., 2018), while “pitahaya” fruits, ancestrally consumed in the Mayan culture. An evaluation was corresponds to the genus Hylocereus (WU et al., 2006). Research on made regarding the physical-chemical characteristics, the nutritional pitahaya was done in this study. components and the antioxidants of the fruits of H. ocamponis The fruit of H. ocamponis (Salm-Dyck) Britton & Rose, known as (mesocarp or red pulp) and H. undatus (white pulp), species of great pitahaya solferina (red epicarp, red, pink or purple mesocarp) is a native commercial importance. The pulp of the fruits presented nutritional species of Mexico (GARCÍA-RUBIO et al., 2015), little documented, and nutraceutical differences between both species. -
Chapter 11: Lipids
ChapterChapter 11:11: LipidsLipids VoetVoet && Voet:Voet: PagesPages 380-394380-394 Lecture 11 Biochemistry 2000 Slide 1 LipidsLipids Lipids are distinguished by their high solubility in non polar solvents and low solubility in H2O ● Diverse group of compounds including Fats, Oils, Waxes, some vitamins and hormones and most non-protein components of membranes Lipids are (another) amphipathic molecules that can be: (A) Major components of biological membranes ● membranes define the basic unit of life (cell) and subcellular compartments (eucaryotes) ● includes cholesterol (B) Major form of stored energy in biological systems Adipocytes: ● lipids are largely reduced compounds; complete oxidation of lipids Fat storage cells generates lots of energy (ie. more than from sugars) (C) Hormones ● signal transduction (communication) between cells Lecture 11 Biochemistry 2000 Slide 2 OverviewOverview ofof BiologicalBiological LipidsLipids Fatty acids: principal building blocks of complex lipids Waxes: esters of fatty acids (heat sensitive) Triacylglycerols: membrane precursors, energy storage Glycerophospholipids: membrane components Sphingolipids: brain lipids, membrane components Steroids: cholesterol, bile salts, steroid hormones Terpenes: like turpentine Lecture 11 Biochemistry 2000 Slide 3 FattyFatty AcidsAcids BuildingBuilding blocksblocks ofof lipidslipids Composed of a carboxylic acid “head group” and a long hydrocarbon “tail” – tail generally contains an even number of carbon atoms Hydrocarbon tail can be saturated or unsaturated – unsaturated -

Fats and Fatty Acid in Human Nutrition
ISSN 0254-4725 91 FAO Fats and fatty acids FOOD AND NUTRITION PAPER in human nutrition Report of an expert consultation 91 Fats and fatty acids in human nutrition − Report of an expert consultation Knowledge of the role of fatty acids in determining health and nutritional well-being has expanded dramatically in the past 15 years. In November 2008, an international consultation of experts was convened to consider recent scientific developments, particularly with respect to the role of fatty acids in neonatal and infant growth and development, health maintenance, the prevention of cardiovascular disease, diabetes, cancers and age-related functional decline. This report will be a useful reference for nutrition scientists, medical researchers, designers of public health interventions and food producers. ISBN 978-92-5-106733-8 ISSN 0254-4725 9 7 8 9 2 5 1 0 6 7 3 3 8 Food and Agriculture I1953E/1/11.10 Organization of FAO the United Nations FAO Fats and fatty acids FOOD AND NUTRITION in human nutrition PAPER Report of an expert consultation 91 10 − 14 November 2008 Geneva FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS Rome, 2010 The designations employed and the presentation of material in this information product do not imply the expression of any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations (FAO) concerning the legal or development status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or products of manufacturers, whether or not these have been patented, does not imply that these have been endorsed or recommended by FAO in preference to others of a similar nature that are not mentioned. -

Fatty Acids: Structures and Introductory Article Properties Article Contents
Fatty Acids: Structures and Introductory article Properties Article Contents . Introduction Arild C Rustan, University of Oslo, Oslo, Norway . Overview of Fatty Acid Structure . Major Fatty Acids Christian A Drevon, University of Oslo, Oslo, Norway . Metabolism of Fatty Acids . Properties of Fatty Acids Fatty acids play a key role in metabolism: as a metabolic fuel, as a necessary component of . Requirements for and Uses of Fatty Acids in Human all membranes, and as a gene regulator. In addition, fatty acids have a number of industrial Nutrition uses. Uses of Fatty Acids in the Pharmaceutical/Personal Hygiene Industries Introduction doi: 10.1038/npg.els.0003894 Fatty acids, both free and as part of complex lipids, play a number of key roles in metabolism – major metabolic fuel (storage and transport of energy), as essential components subsequent one the b carbon. The letter n is also often used of all membranes, and as gene regulators (Table 1). In ad- instead of the Greek o to indicate the position of the double dition, dietary lipids provide polyunsaturated fatty acids bond closest to the methyl end. The systematic nomencla- (PUFAs) that are precursors of powerful locally acting ture for fatty acids may also indicate the location of double metabolites, i.e. the eicosanoids. As part of complex lipids, bonds with reference to the carboxyl group (D). Figure 2 fatty acids are also important for thermal and electrical outlines the structures of different types of naturally insulation, and for mechanical protection. Moreover, free occurring fatty acids. fatty acids and their salts may function as detergents and soaps owing to their amphipathic properties and the for- Saturated fatty acids mation of micelles. -
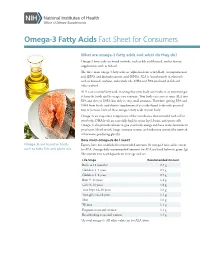
Omega-3 Fatty Acids Fact Sheet for Consumers
Omega-3 Fatty Acids Fact Sheet for Consumers What are omega-3 fatty acids and what do they do? Omega-3 fatty acids are found in foods, such as fish and flaxseed, and in dietary supplements, such as fish oil. The three main omega-3 fatty acids are alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). ALA is found mainly in plant oils such as flaxseed, soybean, and canola oils. DHA and EPA are found in fish and other seafood. ALA is an essential fatty acid, meaning that your body can’t make it, so you must get it from the foods and beverages you consume. Your body can convert some ALA into EPA and then to DHA, but only in very small amounts. Therefore, getting EPA and DHA from foods (and dietary supplements if you take them) is the only practical way to increase levels of these omega-3 fatty acids in your body. Omega-3s are important components of the membranes that surround each cell in your body. DHA levels are especially high in retina (eye), brain, and sperm cells. Omega-3s also provide calories to give your body energy and have many functions in your heart, blood vessels, lungs, immune system, and endocrine system (the network of hormone-producing glands). How much omega-3s do I need? Omega-3s are found in foods Experts have not established recommended amounts for omega-3 fatty acids, except such as fatty fish and plant oils. for ALA. Average daily recommended amounts for ALA are listed below in grams (g). -

Fat and Fatty Acid Content of Selected Foods Containing Trans-Fatty Acids
Fat and Fatty Acid Content of Selected Foods Containing Trans-Fatty Acids Special Purpose Table No. 1 NOTE: The samples analyzed for this table were collected between 1989 and 1993. As the formulations for these products may have changed, caution should be exercised when using these values. Prepared by: Jacob Exler, Linda Lemar, and Julie Smith U.S. Department of Agriculture Agricultural Research Service Beltsville Human Nutrition Research Center Nutrient Data Laboratory 10300 Baltimore Ave. B-005, Rm. 107, BARC-West Beltsville, MD 20705 Tel. 301-504-0630 FAX: 301-504-0632 This table provides analytical data on selected foods containing trans-fatty acids. All of the data presented were obtained under USDA contract. The samples were analyzed by capillary gas-liquid chromatography, and the studies were monitored for quality control. More detailed information on the analytical methodology and quality control can be obtained from the authors at the above address. Codes indicating the source of the data, descriptions of food items, and listings of the fat added as declared on the food labels are given in file below. Codes for sources of data are given for each item. Generic descriptions are provided for all food items reported. The items are arranged by major food category that correspond to the sections of Agriculture Handbook No. 8. A list of the categories is given below. For a given food description, all items bearing the same alphabetic brand designation are the same brand name item. The letter "h" in the fat added field indicates that the fat was either hydrogenated or partially hydrogenated. -

Nutrition Bytes
UCLA Nutrition Bytes Title Theories Presented in The Zone Permalink https://escholarship.org/uc/item/9pg2j7wk Journal Nutrition Bytes, 3(1) ISSN 1548-4327 Author Chang, Jeannie Publication Date 1997 Peer reviewed eScholarship.org Powered by the California Digital Library University of California "Easy -to -follow" diet plans appear each year to convince overweight Americans that there is finally a way to lose weight permanently. Barry Sears and Bill Lawren’s book, The Zone, is no exception; in fact, Sears’ book cover advertises that it is "a dietary road map to lose weight permanently, reset your genetic code, prevent disease, achieve maximum physical performance, [and] enhance mental productivity." But is this realistic? Can a diet really accomplish all of those tasks? After numerous searches through several databases, only two journal articles analyzing this diet plan surfaced, both warning readers about the misinformation contained in the book. There are definitely problems with Sears’ diet; for example, his daily caloric intake recommendation is dangerously low. Tufts University Diet and Nutrition Letter stated that they believed "[Sears was] confusing the near -euphoria he promises from following the Zone diet with lightheadedness from hunger" (3). Dr. Zamenhof, Associate Professor of Biological Ch emistry at UCLA said that it was probably due to an increased release of endorphins, enkephalins, and catecholamines. In addition, the information he provides regarding carbohydrate and fat metabolism, as well as insulin and glucagon secretion, are wrong. However, Sears also says that there is a direct relationship between insulin and glucagon with the synthesis of "good" eicosanoids (prostaglandin E1 and prostaglandin I2 and "bad" eicosanoids (prostaglandin E2, thromboxanes, and leukotrienes).