Nutrition Bytes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Role of 15-Lipoxygenase/15-Hydroxyeicosatetraenoic Acid in Hypoxia-Induced Pulmonary Hypertension
J Physiol Sci (2012) 62:163–172 DOI 10.1007/s12576-012-0196-9 REVIEW Role of 15-lipoxygenase/15-hydroxyeicosatetraenoic acid in hypoxia-induced pulmonary hypertension Daling Zhu • Yajuan Ran Received: 29 September 2011 / Accepted: 25 January 2012 / Published online: 14 February 2012 Ó The Physiological Society of Japan and Springer 2012 Abstract Pulmonary arterial hypertension (PAH) is a Introduction rare disease with a complex aetiology characterized by elevated pulmonary artery resistance, which leads to right Pulmonary hypertension (PH) is a severe and frequently heart ventricular afterload and ultimately progressing to fatal disease characterized by elevated mean pulmonary right ventricular failure and often death. In addition to arterial (PA) pressure greater than 25 mmHg at rest or other factors, metabolites of arachidonic acid cascade play greater than 30 mmHg with exercise [1], and which con- an important role in the pulmonary vasculature, and dis- tributes to the morbidity and mortality of adult and pedi- ruption of signaling pathways of arachidonic acid plays a atric patients with various lung and heart diseases. central role in the pathogenesis of PAH. 15-Lipoxygenase According to the Venice Classification of Pulmonary (15-LO) is upregulated in pulmonary artery endothelial Hypertension in 2003, PH is currently classified into five cells and smooth muscle cells of PAH patients, and its categories as listed in Table 1. Importantly, many of these metabolite 15-hydroxyeicosatetraenoic acid (15-HETE) in diseases or conditions are associated with persistent or particular seems to play a central role in the contractile intermittent hypoxia, either globally or regionally, within machinery, and in the initiation and propagation of cell confined areas of the lung [2]. -

Fatty Acids: Essential…Therapeutic
Volume 3, No.2 May/June 2000 A CONCISE UPDATE OF IMPORTANT ISSUES CONCERNING NATURAL HEALTH INGREDIENTS Written and Edited By: Thomas G. Guilliams Ph.D. FATTY ACIDS: Essential...Therapeutic Few things have been as confusing to both patient and health care provider as the issue of fats and oils. Of all the essential nutrients required for optimal health, fatty acids have not only been forgotten they have been considered hazardous. Health has somehow been equated with “low-fat” or “fat-free” for so long, to suggest that fats could be essential or even therapeutic is to risk credibility. We hope to give a view of fats that is both balanced and scientific. This review will cover the basics of most fats that will be encountered in dietary or supplemental protocols. Recommendations to view essential fatty acids in a similar fashion as essential vitamins and minerals will be combined with therapeutic protocols for conditions ranging from cardiovascular disease, skin conditions, diabetes, nerve related disorders, retinal disorders and more. A complete restoration of health cannot be accomplished until there is a restoration of fatty acid nutritional information among health care professionals and their patients. Fats- What are they? Dietary fats come to us from a variety of sources, but primarily in the form of triglycerides. That is, three fatty acid molecules connected by a glycerol backbone (see fatty acid primer page 3 for diagram). These fatty acids are then used as energy by our cells or modified into phospholipids to be used as cell or organelle membranes. Some fatty acids are used in lipoprotein molecules to shuttle cholesterol and fats to and from cells, and fats may also be stored for later use. -

Essential Fatty Acid Formulas — — — Liquids
To contact Designs for Health, please call us at (800) 847-8302, or visit us on the web at at (800)847-8302,or visit usontheweb please call Health, usat Designs for contact To These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cureor prevent any disease. treat, These products arenotintended todiagnose, Administration. and Drug These statements havenotbeen evaluatedbytheFood Product Comparison Chart OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ OmegAvail™ Ultra Ultra Lemon Drop Synergy TG1000 Hi-Po Ultra Marine Liquid with D3, K1 & K2 DHA Smoothie Unique omega-3-6-7-9 High potency DHA/EPA Great for children and fatty acid formula High potency EPA/DHA formula with flexible Highest potency High potency EPA/ Added D3, K1, K2 for Maintenance and High potency DHA the elderly who prefer offers balanced doses in a single softgel for dosing; ideal for EPA/DHA for most DHA for aggressive cardiovascular & bone general omega-3 formula for therapeutic not to take pills, higher of EPA, DHA, GLA, optimal compliance of children, the elderly & aggressive applications applications and immune support dosing DHA applications dosing is easy with palmitoleic acid, and therapeutic dosing those who prefer not to liquids oleic acid swallow pills Serving Size 2 Softgels 1 Softgel 2 Softgels 2 Softgels 2 Softgels 2 Softgels 1 Softgel 11 g (2 tsp.) 5ml (1 tsp.) EPA (n-3) 270 mg 662 mg 1000 mg 600 mg 600 mg 320 mg 110 mg 1100 mg 725 mg DHA (n-3) 180 mg 250 mg 500 mg 400 mg 400 mg 200 mg 500 mg 720 mg 450 mg Other EFAs 645 mg 88 mg — 200 mg 200 mg 80 mg — 230 mg 180 mg Vitamin D3 — — — — 1000 IU — — — — Vitamin K1/K2 — — — — 500 mcg/25 mcg — — — — www.designsforhealth.com Lipase Yes Yes Yes Yes Yes Yes Yes — — For EveryPatient Essential FattyAcidFormulas SPECIAL FORMULAS The Impact of Fatty Acids Fatty acids have a number of fundamental benefits for human health. -

University of California, San Diego
UNIVERSITY OF CALIFORNIA, SAN DIEGO A Lipidomic Perspective on Inflammatory Macrophage Eicosanoid Signaling A Thesis submitted in partial satisfaction of the requirements for the degree Doctor of Philosophy in Chemistry by Paul Christopher Norris Committee in charge: Professor Edward A. Dennis, Chair Professor Pieter C. Dorrestein Professor Partho Ghosh Professor Christopher K. Glass Professor Michael J. Sailor 2013 The Dissertation of Paul Christopher Norris is approved, and it is acceptable in quality and form for publication on microfilm and electronically: Chair University of California, San Diego 2013 iii DEDICATION To my parents, Darrell and Kathy, for always allowing me to think (and choose) for myself. iv TABLE OF CONTENTS Signature page ............................................................................................................................ iii Dedication .................................................................................................................................. iv Table of contents ......................................................................................................................... v List of symbols and abbreviations ........................................................................................... viii List of figures ............................................................................................................................. xi List of tables ............................................................................................................................ -

The Relationship Between Specialized Pro-Resolving Lipid Mediators, Morbid Obesity and Weight Loss After Bariatric Surgery
www.nature.com/scientificreports OPEN The relationship between specialized pro‑resolving lipid mediators, morbid obesity and weight loss after bariatric surgery Fabian Schulte1,2,7, Abdul Aziz Asbeutah3,6,7, Peter N. Benotti4, G. Craig Wood4, Christopher Still4, Bruce R. Bistrian5, Markus Hardt1,2 & Francine K. Welty3* Obesity and diabetes are associated with chronic infammation. Specialized pro‑resolving lipid mediators (SPMs)—resolvins (Rv), protectins (PD) and maresins (MaR)—actively resolve infammation. Bariatric surgery achieves remission of diabetes, but mechanisms are unclear. We measured SPMs and proinfammatory eicosanoid levels using liquid chromatography‑tandem mass spectrometry in 29 morbidly obese subjects (13 with diabetes) and 15 nondiabetic, mildly obese subjects. Compared to the mildly obese, the morbidly obese had higher levels of SPMs—RvD3, RvD4 and PD1—and white blood cells (WBC) and platelets. Post‑surgery, SPM and platelet levels decreased in morbidly obese nondiabetic subjects but not in diabetic subjects, suggesting continued infammation. Despite similar weight reductions 1 year after surgery (44.6% vs. 46.6%), 8 diabetes remitters had signifcant reductions in WBC and platelet counts whereas fve non‑remitters did not. Remitters had a 58.2% decrease (p = 0.03) in 14‑HDHA, a maresin pathway marker; non‑remitters had an 875.7% increase in 14‑HDHA but a 36.9% decrease in MaR1 to a median of 0. In conclusion, higher levels of RvD3, PD1 and their pathway marker, 17‑HDHA, are markers of leukocyte activation and infammation in morbid obesity and diabetes and diminish with weight loss in nondiabetic but not diabetic subjects, possibly representing sustained infammation in the latter. -

Polyunsaturated Fatty Acids and Their Potential Therapeutic Role in Cardiovascular System Disorders—A Review
nutrients Review Polyunsaturated Fatty Acids and Their Potential Therapeutic Role in Cardiovascular System Disorders—A Review Ewa Sokoła-Wysocza ´nska 1, Tomasz Wysocza ´nski 2, Jolanta Wagner 2,3, Katarzyna Czyz˙ 4,*, Robert Bodkowski 4, Stanisław Lochy ´nski 3,5 and Bozena˙ Patkowska-Sokoła 4 1 The Lumina Cordis Foundation, Szymanowskiego Street 2/a, 51-609 Wroclaw, Poland; [email protected] 2 FLC Pharma Ltd., Wroclaw Technology Park Muchoborska Street 18, 54-424 Wroclaw, Poland; [email protected] (T.W.); jolanta.pekala@flcpharma.com (J.W.) 3 Department of Bioorganic Chemistry, Faculty of Chemistry, University of Technology, Wybrzeze Wyspianskiego Street 27, 50-370 Wroclaw, Poland; [email protected] 4 Institute of Animal Breeding, Faculty of Biology and Animal Sciences, Wroclaw University of Environmental and Life Sciences, Chelmonskiego Street 38c, 50-001 Wroclaw, Poland; [email protected] (R.B.); [email protected] (B.P.-S.) 5 Institute of Cosmetology, Wroclaw College of Physiotherapy, Kosciuszki 4 Street, 50-038 Wroclaw, Poland * Correspondence: [email protected]; Tel.: +48-71-320-5781 Received: 23 August 2018; Accepted: 19 October 2018; Published: 21 October 2018 Abstract: Cardiovascular diseases are described as the leading cause of morbidity and mortality in modern societies. Therefore, the importance of cardiovascular diseases prevention is widely reflected in the increasing number of reports on the topic among the key scientific research efforts of the recent period. The importance of essential fatty acids (EFAs) has been recognized in the fields of cardiac science and cardiac medicine, with the significant effects of various fatty acids having been confirmed by experimental studies. -

Fats and Fatty Acid in Human Nutrition
ISSN 0254-4725 91 FAO Fats and fatty acids FOOD AND NUTRITION PAPER in human nutrition Report of an expert consultation 91 Fats and fatty acids in human nutrition − Report of an expert consultation Knowledge of the role of fatty acids in determining health and nutritional well-being has expanded dramatically in the past 15 years. In November 2008, an international consultation of experts was convened to consider recent scientific developments, particularly with respect to the role of fatty acids in neonatal and infant growth and development, health maintenance, the prevention of cardiovascular disease, diabetes, cancers and age-related functional decline. This report will be a useful reference for nutrition scientists, medical researchers, designers of public health interventions and food producers. ISBN 978-92-5-106733-8 ISSN 0254-4725 9 7 8 9 2 5 1 0 6 7 3 3 8 Food and Agriculture I1953E/1/11.10 Organization of FAO the United Nations FAO Fats and fatty acids FOOD AND NUTRITION in human nutrition PAPER Report of an expert consultation 91 10 − 14 November 2008 Geneva FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS Rome, 2010 The designations employed and the presentation of material in this information product do not imply the expression of any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations (FAO) concerning the legal or development status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or products of manufacturers, whether or not these have been patented, does not imply that these have been endorsed or recommended by FAO in preference to others of a similar nature that are not mentioned. -

Fatty Acids: Structures and Introductory Article Properties Article Contents
Fatty Acids: Structures and Introductory article Properties Article Contents . Introduction Arild C Rustan, University of Oslo, Oslo, Norway . Overview of Fatty Acid Structure . Major Fatty Acids Christian A Drevon, University of Oslo, Oslo, Norway . Metabolism of Fatty Acids . Properties of Fatty Acids Fatty acids play a key role in metabolism: as a metabolic fuel, as a necessary component of . Requirements for and Uses of Fatty Acids in Human all membranes, and as a gene regulator. In addition, fatty acids have a number of industrial Nutrition uses. Uses of Fatty Acids in the Pharmaceutical/Personal Hygiene Industries Introduction doi: 10.1038/npg.els.0003894 Fatty acids, both free and as part of complex lipids, play a number of key roles in metabolism – major metabolic fuel (storage and transport of energy), as essential components subsequent one the b carbon. The letter n is also often used of all membranes, and as gene regulators (Table 1). In ad- instead of the Greek o to indicate the position of the double dition, dietary lipids provide polyunsaturated fatty acids bond closest to the methyl end. The systematic nomencla- (PUFAs) that are precursors of powerful locally acting ture for fatty acids may also indicate the location of double metabolites, i.e. the eicosanoids. As part of complex lipids, bonds with reference to the carboxyl group (D). Figure 2 fatty acids are also important for thermal and electrical outlines the structures of different types of naturally insulation, and for mechanical protection. Moreover, free occurring fatty acids. fatty acids and their salts may function as detergents and soaps owing to their amphipathic properties and the for- Saturated fatty acids mation of micelles. -
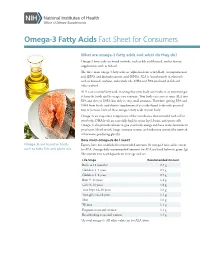
Omega-3 Fatty Acids Fact Sheet for Consumers
Omega-3 Fatty Acids Fact Sheet for Consumers What are omega-3 fatty acids and what do they do? Omega-3 fatty acids are found in foods, such as fish and flaxseed, and in dietary supplements, such as fish oil. The three main omega-3 fatty acids are alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). ALA is found mainly in plant oils such as flaxseed, soybean, and canola oils. DHA and EPA are found in fish and other seafood. ALA is an essential fatty acid, meaning that your body can’t make it, so you must get it from the foods and beverages you consume. Your body can convert some ALA into EPA and then to DHA, but only in very small amounts. Therefore, getting EPA and DHA from foods (and dietary supplements if you take them) is the only practical way to increase levels of these omega-3 fatty acids in your body. Omega-3s are important components of the membranes that surround each cell in your body. DHA levels are especially high in retina (eye), brain, and sperm cells. Omega-3s also provide calories to give your body energy and have many functions in your heart, blood vessels, lungs, immune system, and endocrine system (the network of hormone-producing glands). How much omega-3s do I need? Omega-3s are found in foods Experts have not established recommended amounts for omega-3 fatty acids, except such as fatty fish and plant oils. for ALA. Average daily recommended amounts for ALA are listed below in grams (g). -

Phospholipase A2 Regulates Eicosanoid Class Switching During Inflammasome Activation
Phospholipase A2 regulates eicosanoid class switching during inflammasome activation Paul C. Norrisa, David Gosselinb, Donna Reichartb, Christopher K. Glassb, and Edward A. Dennisa,1 Departments of aChemistry/Biochemistry and Pharmacology, and bCellular and Molecular Medicine, University of California, San Diego, La Jolla, CA 92093 Edited by Michael A. Marletta, The Scripps Research Institute, La Jolla, CA, and approved July 30, 2014 (received for review March 13, 2014) Initiation and resolution of inflammation are considered to be to initiate pathogenic killing, subsequent “class switching” to lipoxin tightly connected processes. Lipoxins (LX) are proresolution lipid (LX) formation by “reprogrammed” neutrophils inhibits additional mediators that inhibit phlogistic neutrophil recruitment and pro- neutrophil recruitment during self-resolving inflammatory resolu- mote wound-healing macrophage recruitment in humans via tion (9). The direct link between inflammatory commitment and potent and specific signaling through the LXA4 receptor (ALX). resolution mediated by eicosanoid signaling in macrophages One model of lipoxin biosynthesis involves sequential metabolism remains unclear from short-term vs. long-term priming, but the of arachidonic acid by two cell types expressing a combined trans- complete temporal changes and important interconnections cellular metabolon. It is currently unclear how lipoxins are effi- within the entire eicosadome are now demonstrated. ciently formed from precursors or if they are directly generated after receptor-mediated inflammatory commitment. Here, we pro- Results vide evidence for a pathway by which lipoxins are generated in We first primed immortalized macrophage-like cells (RAW264.7) macrophages as a consequence of sequential activation of toll-like with the TLR4 agonist Kdo2 lipid A (KLA) for various times and receptor 4 (TLR4), a receptor for endotoxin, and P2X7, a purinergic examined the effects on subsequent purinergic stimulated COX receptor for extracellular ATP. -

Serum N-6 Fatty Acids Are Positively Associated with Growth in 6-To-10-Year Old Ugandan Children Regardless of HIV Status—A Cross-Sectional Study
nutrients Article Serum n-6 Fatty Acids are Positively Associated with Growth in 6-to-10-Year Old Ugandan Children Regardless of HIV Status—A Cross-Sectional Study Raghav Jain 1 , Amara E. Ezeamama 2, Alla Sikorskii 2, William Yakah 1 , Sarah Zalwango 3, Philippa Musoke 4, Michael J. Boivin 5,6 and Jenifer I. Fenton 1,* 1 Department of Food Science and Human Nutrition, Michigan State University, East Lansing, MI 48824, USA; [email protected] (R.J.); [email protected] (W.Y.) 2 Department of Psychiatry, Michigan State University, East Lansing, MI 48824, USA; [email protected] (A.E.E.); [email protected] (A.S.) 3 Directorate of Public Health and Environment, Kampala Capital City Authority, Kampala 00256, Uganda; [email protected] 4 Makerere University-Johns Hopkins University Research Collaboration, Kampala 00256, Uganda; [email protected] 5 Departments of Psychiatry, Neurology & Ophthalmology, Michigan State University, East Lansing, MI 48824, USA; [email protected] 6 Department of Psychiatry, University of Michigan, Ann Arbor, MI 48109, USA * Correspondence: [email protected]; Tel.: +1-517-353-3342; Fax: +1-517-353-8963 Received: 8 April 2019; Accepted: 30 May 2019; Published: 4 June 2019 Abstract: Fatty acids (FAs) are crucial in child growth and development. In Uganda, antiretroviral therapy (ART) has drastically reduced perinatal human immunodeficiency virus (HIV) infection of infants, however, the interplay of FAs, ART, and HIV in relation to child growth is not well understood. To investigate this, serum was collected from 240 children between 6–10 years old in Uganda and analyzed for FAs using gas-chromatography mass-spectrometry. -

Food-Intake Normalization of Dysregulated Fatty Acids in Women with Anorexia Nervosa
nutrients Article Food-Intake Normalization of Dysregulated Fatty Acids in Women with Anorexia Nervosa Nhien Nguyen 1, Michelle Dow 2, Blake Woodside 3, J. Bruce German 4, Oswald Quehenberger 5 and Pei-an Betty Shih 1,* 1 Department of Psychiatry, School of Medicine University of California, San Diego, La Jolla, CA 92037, USA; [email protected] 2 Division of Medical Genetics, Department of Medicine, University of California, San Diego, La Jolla, CA 92093, USA; [email protected] 3 Department of Psychiatry, University of Toronto, Toronto, ON M5T 2S8, Canada; [email protected] 4 Department of Food Science & Technology, University of California, Davis, Davis, CA 95616, USA; [email protected] 5 Department of Pharmacology, University of California, San Diego, San Diego, CA 92093, USA; [email protected] * Correspondence: [email protected]; Tel.: +858-534-0828 Received: 3 August 2019; Accepted: 8 September 2019; Published: 13 September 2019 Abstract: Anorexia nervosa (AN) is a psychiatric disorder affected by psychological, environmental, and biological factors. Individuals with AN avoid high-fat, high-calorie diets and have shown abnormal metabolism of fatty acids (FAs), which are essential for brain and cognitive/neuropsychiatric health. To clarify the relationship between FAs and AN, fasting and postprandial plasma FAs in AN patients and age-matched control women were analyzed via mass-spectrometry. Clinical phenotypes were assessed using Becker Anxiety Inventory and Becker Depression Inventory. AN patients and controls exhibited different FA signatures at both fasting and postprandial timepoints. Lauric acid, eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA), and alpha-linoleic acid (ALA) were higher in AN than in controls (lauric acid: 15,081.6 14,970.2 vs.