2015 National Lipid Association
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

National Lipid Association Annual Summary of Clinical Lipidology 2015
Journal of Clinical Lipidology (2014) 8, S1-S36 Original Contribution National Lipid Association Annual Summary of Clinical Lipidology 2015 Harold E. Bays, MD, FTOS, FACC, FACE, FNLA*, Peter H. Jones, MD, FACP, FNLA, W. Virgil Brown, MD, FNLA, Terry A. Jacobson, MD, FACP, FNLA Louisville Metabolic and Atherosclerosis Research Center, Louisville, KY, USA (Dr Bays); Baylor College of Medicine, Houston, TX, USA (Dr Jones); Emory University School of Medicine, Atlanta, GA, USA (Dr Brown); and Department of Medicine, Emory University, Atlanta, GA, USA (Dr Jacobson) KEYWORDS: Abstract: The National Lipid Association (NLA) Annual Summary of Clinical Lipidology 2015 is a Clinical Lipidology; summary of principles important to the patient-centered evaluation, management, and care of patients Dyslipidemia; with dyslipidemia. This summary is intended to be a ‘‘living document,’’ with future annual updates National Lipid based on emerging science, clinical considerations, and new NLA Position and Consensus Statements. Association; The goal is to provide clinicians an ongoing resource that translates the latest advances in medical Annual Summary; science toward the evaluation and treatment of patients with dyslipidemia. The 2015 NLA Annual Cholesterol; Summary of Clinical Lipidology was founded on the principles of evidence-based medicine and is Recommendations; generally consistent with established national and international lipid guidelines. Topics include a Guidelines general discussion of the 2014 NLA Recommendations for Patient-Centered Management of Dyslipidemia, genetics, secondary causes of dyslipidemia, biomarkers and ‘‘advanced lipid testing,’’ medical nutrition, physical activity, obesity, pharmacotherapy, statin safety, lipid-altering drug interactions, lipoprotein apheresis, dyslipidemia in children and adolescence, dyslipidemia in older individuals, race/ethnicity, and women, health information technology and electronic medical records, as well as investigational lipid-altering drugs in development. -

Blood Fats Explained
Blood Fats Explained HEART UK – The Cholesterol Charity providing expert support, education and influence 2 | Fats in the blood At risk of cardiovascular disease? | 3 Fats in the blood At risk of cardiovascular disease? Fats that circulate in the blood are called lipids. Very low density lipoproteins (VLDL) transport Cardiovascular disease (CVD) is the medical Blood pressure is a measure of the resistance Cholesterol and triglycerides are both lipids. mainly triglycerides made by the liver to where name for circulatory diseases such as coronary to the flow of blood around your body. It is They have essential roles in the body. In excess they are either used to fuel our muscles or stored heart disease (CHD), stroke, mini stroke (transient measured in millimetres of mercury (mmHg). Your they are harmful. for later use. ischaemic attack or TIA), angina and peripheral doctor or nurse will measure both your systolic vascular disease (PVD). You are more likely to (upper figure) and diastolic (lower figure) blood Cholesterol is needed to build cell walls and Low density lipoproteins (LDL) carry most of the develop CVD the more risk factors you have. pressure. About a third of adults have high blood to make hormones and vitamin D. Some of our cholesterol in our body from the liver to the cells pressure. If untreated it increases the risk of cholesterol comes from the food we eat; but most that need it. The cholesterol that is carried on LDLs There are two types of risk factors: heart attack and stroke. High blood pressure is is made in the liver. -

Geeta Sikand, MS
Geeta Sikand, MA, RDN, FAND, CDE, CLS, FNLA Geeta Sikand is an Associate Clinical Professor of Medicine in Cardiology at the University of California, Irvine School of Medicine. Registered Dietitian Nutritionist, Clinical Lipid Specialist, Certified Diabetes Educator, Fellow of the National Lipid Association and Fellow of the Academy of Nutrition and Dietetics. Ms Sikand is Director of Nutrition at University of California Irvine Preventive Cardiology Program. Ms Sikand is the recipient of the 2016 Lifetime Achievement Award from the Academy of Nutrition and Dietetics Member Interest Group, the 2013 Distinguished Service Award from the Dietitians’ in Health Care Communities Practice Group. For her research on the effectiveness of medical nutrition therapy in dyslipidemia, Geeta was the 2001 recipient of the Academy of Nutrition & Dietetics prestigious "Mary Huddleson Award” and the 1997 Excellence in Research Award from the California Academy of Nutrition and Dietetics. Ms Sikand is Chair, Medical Nutrition Therapy Effectiveness Expert Workgroup of the Academy of Nutrition & Dietetics and served as Expert Member of the Disorders of Lipid Metabolism Expert Panel. Ms Sikand has served on the Board of Directors of the American Heart Association and as Vice President of Public Policy for California Dietetic Association. As President of California Dietetic Association: Orange District and Chair of Southern California Legislative Steering Committee Ms Sikand organized the first ever onsite Congressional visit with Congressman Ron Packard to seek his support for the Medicare medical nutrition therapy legislation which passed in 1996. Ms Sikand is a member of the Pacific Lipid Association (PLA) and has served on the National Lipid Association (NLA) Expert Panel “Recommendations for Patient Centered Management of Dyslipidemia” published in December 2015. -

Genetic Testing for Familial Hypercholesterolemia AHS – M2137
Corporate Medical Policy Genetic Testing for Familial Hypercholesterolemia AHS – M2137 File Name: genetic_testing_for_familial_hypercholesterolemia Origination: 01/01/2019 Last CAP Review: 07/2021 Next CAP Review: 07/2022 Last Review: 07/2021 Description of Procedure or Service Definitions Familial hypercholesterolemia (FH) is a genetic condition that results in premature atherosclerotic cardiovascular disease due to lifelong exposure to elevated low-density lipoprotein cholesterol (LDL-C) levels (Sturm et al., 2018). FH encompasses multiple clinical phenotypes associated with distinct molecular etiologies. The most common is an autosomal dominant disorder caused by mutations in one of three genes, low-density lipoprotein receptor (LDLR), apolipoprotein B-100 (APOB), and proprotein convertase subtilisin-like kexin type 9 (PCSK9) (Ahmad et al., 2016; Goldberg et al., 2011). Rare autosomal recessive disease results from mutation in low-density lipoprotein receptor adaptor protein (LDLRAP) (Garcia et al., 2001). Related Policies Cardiovascular Disease Risk Assessment AHS – G2050 ***Note: This Medical Policy is complex and technical. For questions concerning the technical language and/or specific clinical indications for its use, please consult your physician. Policy BCBSNC will provide coverage for genetic testing for familial hypercholesterolemia when it is determined the medical criteria or reimbursement guidelines below are met. Benefits Application This medical policy relates only to the services or supplies described herein. Please refer to the Member's Benefit Booklet for availability of benefits. Member's benefits may vary according to benefit design; therefore member benefit language should be reviewed before applying the terms of this medical policy. When Genetic Testing for Familial Hypercholesterolemia is covered 1. Genetic testing to establish a molecular diagnosis of Familial Hypercholesterolemia is considered medically necessary when BOTH of the following criteria are met: A. -

Lipodystrophy Due to Adipose Tissue Specific Insulin Receptor
Page 1 of 50 Diabetes Lipodystrophy Due to Adipose Tissue Specific Insulin Receptor Knockout Results in Progressive NAFLD Samir Softic1,2,#, Jeremie Boucher1,3,#, Marie H. Solheim1,4, Shiho Fujisaka1, Max-Felix Haering1, Erica P. Homan1, Jonathon Winnay1, Antonio R. Perez-Atayde5, and C. Ronald Kahn1. 1 Section on Integrative Physiology and Metabolism, Joslin Diabetes Center and Department of Medicine, Harvard Medical School, Boston, MA 2 Division of Gastroenterology, Hepatology and Nutrition, Boston Children’s Hospital, Boston, MA 3 Cardiovascular and Metabolic Diseases iMed, AstraZeneca R&D, 431 83 Mölndal, Sweden (current address) 4 KG Jebsen Center for Diabetes Research, Department of Clinical Science, University of Bergen, Bergen, Norway 5 Department of Pathology, Boston Children’s Hospital, and Harvard Medical School, Boston, MA # These authors contributed equally to this work. Corresponding author: C. Ronald Kahn, MD Joslin Diabetes Center One Joslin Place Boston, MA 02215 Phone: (617)732-2635 Fax:(617)732-2487 E-mail: [email protected] Keywords: Insulin receptors, IGF-1 receptors, lipodystrophy, diabetes, dyslipidemia, fatty liver, liver tumor, NAFLD, NASH. Running title: Lipodystrophic mice develop progressive NAFLD 1 Diabetes Publish Ahead of Print, published online May 10, 2016 Diabetes Page 2 of 50 SUMMARY Ectopic lipid accumulation in the liver is an almost universal feature of human and rodent models of generalized lipodystrophy and also is a common feature of type 2 diabetes, obesity and metabolic syndrome. Here we explore the progression of fatty liver disease using a mouse model of lipodystrophy created by a fat-specific knockout of the insulin receptor (F-IRKO) or both IR and insulin-like growth factor-1 receptor (F- IR/IGF1RKO). -
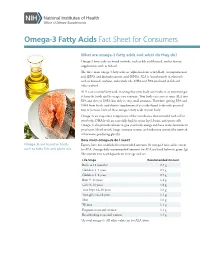
Omega-3 Fatty Acids Fact Sheet for Consumers
Omega-3 Fatty Acids Fact Sheet for Consumers What are omega-3 fatty acids and what do they do? Omega-3 fatty acids are found in foods, such as fish and flaxseed, and in dietary supplements, such as fish oil. The three main omega-3 fatty acids are alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). ALA is found mainly in plant oils such as flaxseed, soybean, and canola oils. DHA and EPA are found in fish and other seafood. ALA is an essential fatty acid, meaning that your body can’t make it, so you must get it from the foods and beverages you consume. Your body can convert some ALA into EPA and then to DHA, but only in very small amounts. Therefore, getting EPA and DHA from foods (and dietary supplements if you take them) is the only practical way to increase levels of these omega-3 fatty acids in your body. Omega-3s are important components of the membranes that surround each cell in your body. DHA levels are especially high in retina (eye), brain, and sperm cells. Omega-3s also provide calories to give your body energy and have many functions in your heart, blood vessels, lungs, immune system, and endocrine system (the network of hormone-producing glands). How much omega-3s do I need? Omega-3s are found in foods Experts have not established recommended amounts for omega-3 fatty acids, except such as fatty fish and plant oils. for ALA. Average daily recommended amounts for ALA are listed below in grams (g). -

Pathophysiology of Adipocyte Defects and Dyslipidemia in HIV Lipodystrophy: New Evidence from Metabolic and Molecular Studies
American Journal of Infectious Diseases 2 (3): 167-172, 2006 ISSN 1553-6203 © 2006 Science Publications Pathophysiology of Adipocyte Defects and Dyslipidemia in HIV Lipodystrophy: New Evidence from Metabolic and Molecular Studies 1,6Ashok Balasubramanyam, 1,6Rajagopal V. Sekhar, 2,3Farook Jahoor 4Henry J. Pownall and 5Dorothy Lewis 1Translational Metabolism Unit, Division of Diabetes, Endocrinology and Metabolism, 2Department of Pediatrics, 3Children’s Nutrition Research Center 4Section of Atherosclerosis and Lipoprotein Metabolism, 5Department of Immunology Baylor College of Medicine; 6Endocrine Service, Ben Taub General Hospital, Houston, Texas Abstract: Despite a burgeoning mass of descriptive information regarding the epidemiology, clinical features, body composition changes, hormonal alterations and dyslipidemic patterns in patients with HIV lipodystrophy syndrome (HLS), the specific biochemical pathways that are dysregulated in the condition and the molecular mechanisms that lead to their dysfunction, remain relatively unexplored. In this paper, we review studies that detail the metabolic basis of the dyslipidemia - specifically, the hypertriglyceridemia - that is the serologic hallmark of HLS and present new data relevant to mechanisms of dyslipidemia in the postprandial state. We also describe preliminary experiments showing that in addition to the well-known effects of highly-active antiretroviral drugs, the functional disruption of adipocytes and preadipocytes by factors intrinsic to HIV-infected immunocytes may play a role in the pathogenesis of HLS. Key words: Triglycerides, cholesterol, lipoprotein lipase, lipolysis, lymphocyte INTRODUCTION Metabolic basis of HLS - studies in the fasting and fed state: Whole body kinetic studies have Characteristics of dyslipidemia and its relationship demonstrated defects in specific lipid metabolic [19-21] to lipodystrophy: A characteristic dyslipidemic pattern pathways in HLS patients in both the fasting and observed in the majority of patients with HLS is fed (25) states. -

Lipoprotein Lipase: a General Review Moacir Couto De Andrade Júnior1,2*
Review Article iMedPub Journals Insights in Enzyme Research 2018 www.imedpub.com Vol.2 No.1:3 ISSN 2573-4466 DOI: 10.21767/2573-4466.100013 Lipoprotein Lipase: A General Review Moacir Couto de Andrade Júnior1,2* 1Post-Graduation Department, Nilton Lins University, Manaus, Amazonas, Brazil 2Department of Food Technology, Instituto Nacional de Pesquisas da Amazônia (INPA), Manaus, Amazonas, Brazil *Corresponding author: MC Andrade Jr, Post-Graduation Department, Nilton Lins University, Manaus, Amazonas, Brazil, Tel: +55 (92) 3633-8028; E-mail: [email protected] Rec date: March 07, 2018; Acc date: April 10, 2018; Pub date: April 17, 2018 Copyright: © 2018 Andrade Jr MC. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Citation: Andrade Jr MC (2018) Lipoprotein Lipase: A General Review. Insights Enzyme Res Vol.2 No.1:3 Abstract Lipoprotein Lipase: Historical Hallmarks, Enzymatic Activity, Characterization, and Carbohydrates (e.g., glucose) and lipids (e.g., free fatty acids or FFAs) are the most important sources of energy Present Relevance in Human for most organisms, including humans. Lipoprotein lipase (LPL) is an extracellular enzyme (EC 3.1.1.34) that is Pathophysiology and Therapeutics essential in lipoprotein metabolism. LPL is a glycoprotein that is synthesized and secreted in several tissues (e.g., Macheboeuf, in 1929, first described chemical procedures adipose tissue, skeletal muscle, cardiac muscle, and for the isolation of a plasma protein fraction that was very rich macrophages). At the luminal surface of the vascular in lipids but readily soluble in water, such as a lipoprotein [1]. -

Other Types of Primary Hyperlipoproteinemia
82 Journal of Atherosclerosis and Thrombosis Vol.21, No.2 Committee Report 10 Other Types of Primary Hyperlipoproteinemia (Hyperlipidemia) Executive Summary of the Japan Atherosclerosis Society (JAS) Guidelines for the Diagnosis and Prevention of Atherosclerotic Cardiovascular Diseases in Japan ― 2012 Version Tamio Teramoto, Jun Sasaki, Shun Ishibashi, Sadatoshi Birou, Hiroyuki Daida, Seitaro Dohi, Genshi Egusa, Takafumi Hiro, Kazuhiko Hirobe, Mami Iida, Shinji Kihara, Makoto Kinoshita, Chizuko Maruyama, Takao Ohta, Tomonori Okamura, Shizuya Yamashita, Masayuki Yokode and Koutaro Yokote Committee for Epidemiology and Clinical Management of Atherosclerosis 1. Primary Hyperlipoproteinemias (Hyperlipidemias) enhanced hepatic apolipoprotein (apo) B-100 synthe- Other Than Familial Hypercholesterolemia sis, decreased LPL activity, increased very-low-density There are various types of primary hyperlipopro- lipoprotein (VLDL) secretion from the liver and the teinemias (hyperlipidemias) other than familial hyper- accumulation of visceral fat as factors for the develop- cholesterolemia (FH). These types are clinically ment of symptoms and has been reported to be related important and classified according to their associated to abnormalities of the LPL and APOC-Ⅱ genes or pathophysiology and genetic abnormalities (Table 1)1). APOA-Ⅰ/C-Ⅲ/A-Ⅳ gene cluster. However, none of Familial lipoprotein lipase (LPL) deficiency manifests these findings have been proven to be definitive. It has as severe hyperchylomicronemia and may present with also been suggested that FCHL is caused by a poly- eruptive cutaneous xanthomas or acute pancreatitis, genic background that tends to induce hyperlipopro- although it does not necessarily accompany atheroscle- teinemia due to environmental factors, such as over- rotic cardiovascular disease (CVD). On the other nutrition and a low level of physical activity. -

National Lipid Association Annual Summary of Clinical Lipidology 2016
Journal of Clinical Lipidology (2016) 10, S1-S43 National Lipid Association Annual Summary of Clinical Lipidology 2016 Harold E. Bays, MD, FNLA*, Peter H. Jones, MD, FNLA, Carl E. Orringer, MD, FNLA, W. Virgil Brown, MD, FNLA, Terry A. Jacobson, MD, FNLA Louisville Metabolic and Atherosclerosis Research Center, Louisville, KY, USA (Dr Bays); Baylor College of Medicine, Houston, TX, USA (Dr Jones); University of Miami Leonard M. Miller School of Medicine, Miami, FL (Dr Orringer); Emory University School of Medicine, Atlanta, GA, USA (Dr Brown); and Department of Medicine, Emory University, Atlanta, GA, USA (Dr Jacobson) KEYWORDS: Abstract: The National Lipid Association (NLA) Annual Summary of Clinical Lipidology is a yearly Clinical Lipidology; updated summary of principles important to the patient-centered evaluation, management, and care Dyslipidemia; of patients with dyslipidemia. This summary is intended to be a ‘‘living document,’’ with future annual National Lipid updates based on emerging science, clinical considerations, and new NLA Position, Consensus, and Association; Scientific Statements, thus providing an ongoing resource that applies the latest in medical science to- Annual Summary; wards the clinical management of patients with dyslipidemia. Topics include the NLA Recommenda- Cholesterol; tions for Patient-Centered Management of Dyslipidemia, genetics, Familial Hypercholesterolemia, Recommendations; secondary causes of dyslipidemia, biomarkers and advanced lipid testing, nutrition, physical activity, Guidelines obesity, adiposopathy, metabolic syndrome, diabetes mellitus, lipid pharmacotherapy, lipid-altering drug interactions, lipoprotein apheresis, dyslipidemia management and treatment based upon age (chil- dren, adolescents, and older individuals), dyslipidemia considerations based upon race, ethnicity and gender, dyslipidemia and human immune virus infection, dyslipidemia and immune disorders, adher- ence strategies and collaborative care, and lipid-altering drugs in development. -

Familial Partial Lipodystrophy
Familial Partial Lipodystrophy Purvisha Patel; Ralph Starkey, MD; Michele Maroon, MD The lipodystrophies are rare disorders character- ized by insulin resistance and the absence or loss of body fat. The 4 subtypes of lipodystrophy are characterized by onset and distribution. Partial lipodystrophy is rare, with loss of fat from the extremities and excess fat accumulation in the face and neck; recognizing this phenotype and subsequent referral for endocrinologic care may improve outcome and reduce mortality. ipodystrophies are rare disorders characterized by insulin resistance and the absence or L loss of body fat.1 Classification of the 4 main subtypes of lipodystrophy is based on onset (congenital/familial vs acquired/sporadic) and dis- Figure not available online tribution (total/generalized vs partial). Congenital total lipodystrophy (also known as Berardinelli syndrome, Seip syndrome) is a rare autosomal- recessive disorder marked by an almost complete lack of adipose tissue from birth. Familial partial lipodystrophy (also known as Kobberling-Dunnigan syndrome) involves loss of subcutaneous fat from the extremities and accumulation of excess fat in the face and neck and to a lesser extent in the hands and feet. Acquired total lipodystrophy (also known as lipoatrophy, Lawrence-Seip syndrome) presents with generalized loss of fat beginning in childhood. Acquired partial lipodystrophy (also known as progressive lipodystrophy, partial lipoat- Figure 1. Accentuation of fat pads in the face and neck. rophy, Barraquer-Simons syndrome) is character- ized by loss of fat only from the upper extremities, face, and trunk.2 tional uterine bleeding (gravida 2, para 1, AB 1) Case Report necessitating total hysterectomy. On physical A 39-year-old white woman presented with the examination, accentuation of fat pads in the face complaint of thickened brown skin on the neck and and neck (Figure 1), central obesity, and prominent medial thighs. -
Evaluation and Management of Dyslipidemia in Patients Treated with Lorlatinib
Guidelines Evaluation and Management of Dyslipidemia in Patients Treated with Lorlatinib Normand Blais 1,* , Jean-Philippe Adam 2 , John Nguyen 2 and Jean C. Grégoire 3 1 Service d’Hématologie-Oncologie, Département de Médicine, Centre Hospitalier de l’Université de Montréal (CHUM), Montréal, QC H2X 3E4, Canada 2 Département de Pharmacie, Centre Hospitalier de l’Université de Montréal (CHUM), Université de Montréal, Montréal, QC H2X 3E4, Canada; [email protected] (J.-P.A.); [email protected] (J.N.) 3 Département de Cardiologie, Institut de Cardiologie de Montréal, Montréal, QC H2X 3E4, Canada; [email protected] * Correspondence: [email protected]; Tel.: +1-514-890-8000 (ext. 25381); Fax: +1-514-412-7572 Received: 22 December 2020; Accepted: 23 December 2020; Published: 4 January 2021 Abstract: The use of lorlatinib, an anaplastic lymphoma kinase (ALK) inhibitor for the treatment of ALK-positive metastatic non-small cell lung cancer, is associated with dyslipidemia in over 80% of patients. Clinical trial protocols for the management of lorlatinib-associated dyslipidemia differ from clinical practice guidelines for the management of dyslipidemia to prevent cardiovascular disease, in that they are based on total cholesterol and triglyceride levels rather than on the low-density lipoprotein cholesterol and non-high-density lipoprotein cholesterol levels that form the basis of current cardiovascular guideline recommendations. In order to simplify and harmonize the management of cardiovascular risk in patients with lorlatinib, an advisory committee consisting of a medical oncologist, a cardiologist, and two pharmacists with expertise in cardiology and oncology aimed to develop a simplified algorithm, adapted from the Canadian Cardiovascular Society dyslipidemia recommendations.