Gerold L. Schiebler, MD
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Re-Writing the Script : Representations of Transgender Creativity In
Kate Norbury Re-writing the Script: Representations of Transgender Creativity in Contemporary Young Adult Fiction and Television Abstract: The transgender, gender-atypical or intersex protagonist challeng- es normative assumptions and expectations about gender, identity and sexu- ality. This article argues that contemporary transgender-themed young adult fiction and television uses the theme of creativity or the creative achievement script to override previously negative representations of adolescent transgender subjectivities. I consider three English-language novels and one television series for young adults and use script theory to analyse these four texts. Cris Beam’s I Am J (2011) and Kirstin Cronn-Mills’ Beautiful Music for Ugly Children (2012), both originally published in the United States, depict female to male transitions. Alyssa Brugman’s Alex As Well (2013), originally published in Australia, foregrounds the experience of an inter- sex teenager, Alex, raised as a boy, but who, at the age of fourteen, decides she is female. Glee introduced the transgender character Unique in 2012, and in 2014 she continued to be a central member of the New Directions choir. The Swedish graphic novel, Elias Ericson’s Åror (Oars, 2013), includes two transgender characters who enact the creative achievement script and fall in love with each other. Ericson’s graphic novel goes further than the English-language texts to date. Collectively, these transgender, gender-atypical or intersex protagonists and central characters assert their creativity and individual agency. The transgender character’s particular cre- ativity ultimately secures a positive sense of self. This more recent selection of texts which date from 2011 validate young adult transgender experience and model diversity and acceptance. -
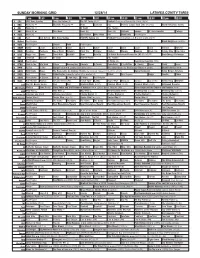
Sunday Morning Grid 12/28/14 Latimes.Com/Tv Times
SUNDAY MORNING GRID 12/28/14 LATIMES.COM/TV TIMES 7 am 7:30 8 am 8:30 9 am 9:30 10 am 10:30 11 am 11:30 12 pm 12:30 2 CBS CBS News Sunday Face the Nation (N) The NFL Today (N) Å Football Chargers at Kansas City Chiefs. (N) Å 4 NBC News (N) Å Meet the Press (N) Å News 1st Look Paid Premier League Goal Zone (N) (TVG) World/Adventure Sports 5 CW News (N) Å In Touch Paid Program 7 ABC News (N) Å This Week News (N) News (N) Outback Explore St. Jude Hospital College 9 KCAL News (N) Joel Osteen Mike Webb Paid Woodlands Paid Program 11 FOX Paid Joel Osteen Fox News Sunday FOX NFL Sunday (N) Football Philadelphia Eagles at New York Giants. (N) Å 13 MyNet Paid Program Black Knight ›› (2001) 18 KSCI Paid Program Church Faith Paid Program 22 KWHY Como Local Jesucristo Local Local Gebel Local Local Local Local Transfor. Transfor. 24 KVCR Painting Dewberry Joy of Paint Wyland’s Paint This Painting Kitchen Mexico Cooking Chefs Life Simply Ming Ciao Italia 28 KCET Raggs Play. Space Travel-Kids Biz Kid$ News Asia Biz Ed Slott’s Retirement Rescue for 2014! (TVG) Å BrainChange-Perlmutter 30 ION Jeremiah Youssef In Touch Hour Of Power Paid Program 34 KMEX Paid Program Al Punto (N) República Deportiva (TVG) 40 KTBN Walk in the Win Walk Prince Redemption Liberate In Touch PowerPoint It Is Written B. Conley Super Christ Jesse 46 KFTR Tu Dia Tu Dia Happy Feet ››› (2006) Elijah Wood. -

German Jews in the United States: a Guide to Archival Collections
GERMAN HISTORICAL INSTITUTE,WASHINGTON,DC REFERENCE GUIDE 24 GERMAN JEWS IN THE UNITED STATES: AGUIDE TO ARCHIVAL COLLECTIONS Contents INTRODUCTION &ACKNOWLEDGMENTS 1 ABOUT THE EDITOR 6 ARCHIVAL COLLECTIONS (arranged alphabetically by state and then city) ALABAMA Montgomery 1. Alabama Department of Archives and History ................................ 7 ARIZONA Phoenix 2. Arizona Jewish Historical Society ........................................................ 8 ARKANSAS Little Rock 3. Arkansas History Commission and State Archives .......................... 9 CALIFORNIA Berkeley 4. University of California, Berkeley: Bancroft Library, Archives .................................................................................................. 10 5. Judah L. Mages Museum: Western Jewish History Center ........... 14 Beverly Hills 6. Acad. of Motion Picture Arts and Sciences: Margaret Herrick Library, Special Coll. ............................................................................ 16 Davis 7. University of California at Davis: Shields Library, Special Collections and Archives ..................................................................... 16 Long Beach 8. California State Library, Long Beach: Special Collections ............. 17 Los Angeles 9. John F. Kennedy Memorial Library: Special Collections ...............18 10. UCLA Film and Television Archive .................................................. 18 11. USC: Doheny Memorial Library, Lion Feuchtwanger Archive ................................................................................................... -

Pure Magazine
PURE MAGAZINOctobeEr 2017 Jack O’Rourke Talks Music, Electric Picnic, Father John Misty and more… The Evolution Of A Modern Gentleman Jimmy Star chats with Hollywood actor... Sean Kanan Sony’s VR capabilities establishes them as serious contenders in the Virtual Reality headset war! Eli Lieb Talks Music, Creating & Happiness… Featured Artist Dionne Warwick Marilyn Manson Cheap Trick Otherkin Eileen Shapiro chats with award winning artist Emma Langford about her Debut + much more EalbumM, tour neMws plus mAore - T urLn to pAage 16 >N> GFORD @PureMzine Pure M Magazine ISSUE 22 Mesmerising WWW.PUREMZINE.COM forty seven Editor in Chief Trevor Padraig [email protected] and a half Editorial Paddy Dunne [email protected] minutes... Sarah Swinburne [email protected] Shane O’ Rielly [email protected] Marilyn Manson Heaven Upside Down Contributors Dave Simpson Eileen Shapiro Jimmy Star Garrett Browne lt-rock icon Marilyn Manson is back “Say10” showcases a captivatingly creepy Danielle Holian brandishing a brand new album coalescence of hauntingly hushed verses and Simone Smith entitled Heaven Upside Down. fantastically fierce choruses next as it Irvin Gamede ATackling themes such as sex, romance, saunters unsettlingly towards the violence and politics, the highly-anticipated comparatively cool and catchy “Kill4Me”. Front Cover - Ken Coleman sequel to 2015’s The Pale Emperor features This is succeeded by the seductively ten typically tumultuous tracks for fans to psychedelic “Saturnalia”, the dreamy yet www.artofkencoleman.com feast upon. energetic delivery of which ensures it stays It’s introduced through the sinister static entrancing until “Je$u$ Cri$i$” arrives to of “Revelation #12” before a brilliantly rivet with its raucous refrain and rebellious bracing riff begins to blare out beneath a instrumentation. -

Vicks Vaporub Shows Its Speed
Vicks VapoRub Professor Ron Eccles shows its speed Dr David Hull VICKS VAPORUB SHOWS ITS SPEED Vicks VapoRub (VVR) has been commercially available for over 100 years, as a remedy for congested nasal passages. A study led by Professor Ron Eccles and Dr David Hull has now demonstrated the speed of its effect in common cold sufferers. To begin, what attracted you to this area Dr David Hull: We continue to explore the in the treatment of upper respiratory tract of research? attributes of all products, young and old. infections such as the common cold and Diseases in collaboration with researchers As ideas, and sometimes new methods flu. Since science came to understand the MEASURING HOW RAPIDLY at the Common Cold and Nasal Research Professor Ron Eccles: During my modular emerge, we strive to bring this to bear by receptor biochemistry of these substances, Centre at Cardiff University, focussed on zoology undergraduate course at Liverpool gathering an improved understanding of the exploration of their effects has been the speed of action of VVR, compared to University, I chose to do a module in their effects. We knew that VapoRub was more easily explained. Also as we now VICKS VAPORUB EXERTS ITS a petrolatum control using a group of 50 pharmacology. I found the investigation fast-acting (just open the jar and you can feel have a receptor-based pharmacology for common-cold sufferers. Cold and flu sufferers of how drugs work in humans an amazing an effect), but we had not tried to quantify aromatic oils to work with, we can better PHARMACOLOGY report that one of the main desires for any and exciting area of study and decided that before and we did not know if the feeling plan experiments such as this one in the medication is a feeling of rapid relief from to switch my undergraduate studies to extended from just cooling to an actual expectation of an interesting and valuable Researchers at the Common Cold and Nasal Research Centre at Cardiff nasal congestion, as this symptom interferes pharmacology. -

Group Weight Loss and Multiple Screening
This is a preprint of an accepted article scheduled to appear in the Bulletin of the History of Medicine, vol. 92, no. 3 (Fall 2018). It has been copyedited but not paginated. Further edits are possible. Please check back for final article publication details. Group Weight Loss and Multiple Screening: A Tale of Two Heart Disease Programs in Postwar American Public Health NICOLAS RASMUSSEN SUMMARY: In the late 1940s, amid elevated concern about heart disease and new funding to fight it, multiple screening emerged alongside group psychotherapy for weight loss as two innovative responses of the American public health community. I describe the early trajectory and fate in the 1950s of both programs as shaped by the ongoing political controversy about national health insurance. Group weight loss became the main de facto American response to a perceived obesity-driven heart disease crisis. The episode casts light on the larger picture of how postwar American public health gravitated toward interventions centered on individual behavior and may offer lessons for obesity interventions today. KEYWORDS: obesity, public health, history, Paul Dudley White, David Rutstein, Louis Israel Dublin, Framingham study, epidemiology, group therapy 1 This is a preprint of an accepted article scheduled to appear in the Bulletin of the History of Medicine, vol. 92, no. 3 (Fall 2018). It has been copyedited but not paginated. Further edits are possible. Please check back for final article publication details. The dramatic expansion of biomedicine in the postwar United States has long attracted the attention of historians. With many in Congress wishing to show concern for the nation’s health, without running afoul of organized medicine’s fierce opposition to President Truman’s 1948 health reform initiative, generous federal research funding to conquer disease in the future emerged as a bipartisan project that substituted for funding to fight illness in the present. -

Paul Dudley White (1886-1973)
182 Cox, Heald, Murday coronary fistulas is preferentially performed at their distal, low pressure end because this ..... .... reduces the risk of compromising flow in the feeding artery. However, coronary fistulas often terminate in more than one distal con- nection and successful distal ligation can prove Heart: first published as 10.1136/hrt.76.2.182 on 1 August 1996. Downloaded from U difficult. This case supports the value of TOE for the perioperative evaluation of coronary .... fistulas-6 and illustrates how this technique may be used to identify cases that require proximal ligation. 1 Hobbs RE, Millit HD, Raghavan PV, Moodie DS, Sheldon WC. Coronary artery fistulae: a 10-year review. Cleveland Clinic Quarterly 1982;49:191-7. 2 Wilde P, Watt I. Congenital coronary artery fistulae: six new cases with a collective review. Clin Radiol 1980;31: 301-11. 3 Liberthson RR, Sagar K, Berkoben JP, Weintraub RM, Levine FH. Congenital coronary arteriovenous fistula. Report of 13 patients, review of the literature and delin- eation of management. Circulation 1979;59:849-54. 4 Giannoccaro PJ, Sochowski RA, Morton BC, Chan KL. Complementary role of transoesophageal echocardiogra- phy to coronary angiography in the assessment of Figure 2 Perioperative transoesophageal echocardiogram ofthe tortuous coronary fistu coronary artery anomalies. BrHeartJ 1993;70:70-4. Colourflow Doppler demonstrates the presence ofresidualflow in thefistula despite initi 5 Calafiore PA, Raymond R, Schiavone WA, Rosenkranz distal surgical ligation. ER. Precise evaluation of a complex coronary arterio- venous fistula: the utility of transoesophageal color Doppler. JAm Soc Echocardiogr 1989;2:337-41. because, although they are often asympto- 6 Stevenson JG, Sorensen GK, Stamm SJ, McCloskey JP, matic, such fistulas may lead to late Hall DG, Rittenhouse EA. -

Trinity Support Asked for WSSF to Help Needy Students Abroad
TRI , , ft t Volume XLV HARTFORD, CONN., DECEMBER 17, 1947 Number 10 Trinity Support Asked for WSSF Boosters Club to Trinity Basketeers Overwhelm Sponsor Pre-Xmas To Help Needy Students Abroad Williams in Home Debut, 58-36 I Dance This Evening Kitchen Describes Large Crowd Expected I I Ron Watson High Scorer Conditions; Drive Debaters Defeat At Festivities; Pipes Stassen Interviewed As Ephmen Succumb I Begins in January Haverford in Octet to Entertain By "Tdpod" Reporter At State Armory Speaking in Wednesday's Chapel This evening at 8:30 an informal By Bill Wetter service, Mr. Wilmer J. Kitchen asked Opening Battle pre-Christmas dance will be held in At Yale Meeting 1 I Trinity's support in a drive to give Cook Lounge and Hamlin Dining Hall An estimated crowd of 1600 watched Taking the negative side of the On Monday afternoon, December 8, 400,000 students abroad direly needed to help get the vacation off to a flying Trinity bounce back from its defeat question "Should the United States food, clothes, shelter, and hospitaliza start. The dance will be sponsored by about one hundred collegiate and pro- by M.I.T. earlier in the week, to romp Adopt Universal Military Training?", tion. Mr. Kitchen, Executive Secre the increasingly active Boosters Club. fessional newspaper reporters gath over the Ephmen of Williams to the I the Trinity debating team of David tary of the Wedel Student Service Music will be by Ed Lally, his piano e1·ed at the "Yale Daily News" build tune of 58 to 36, at the State Armory Rivkin and Samuel Goldstein opened Fund, said that due to crop failures and his orchestra, and refreshments last Saturday night. -

History of the American Heart Association
History of the American Heart Association Our Lifesaving History Before the American Heart Association existed, people with heart disease were thought to be doomed to complete bed rest — or destined to imminent death. But a handful of pioneering physicians and social workers believed it didn’t have to be that way. They conducted studies to learn more about heart disease, America’s No. 1 killer. Then, on June 10, 1924, they met in Chicago to form the American Heart Association — believing that scientific research could lead the way to better treatment, prevention and ultimately a cure. The early American Heart Association enlisted help from hundreds, then thousands, of physicians and scientists. “We were living in a time of almost unbelievable ignorance about heart disease,” said Paul Dudley White, one of six cardiologists who founded the organization. In 1948, the association reorganized, transforming from a professional scientific society to a nationwide voluntary health organization composed of science and lay volunteers and supported by professional staff. Since then, the AHA has grown rapidly in size and influence — nationally and internationally — into an organization of more than 33 million volunteers and supporters dedicated to improving heart health and reducing deaths from cardiovascular diseases and stroke. Here is a timeline of American Heart Association milestones in more than 90 years of lifesaving history: 1915 Looking for Answers: Nearly a decade before the formal creation of the American Heart Association, physicians and social workers convene to find more answers about the mysteries of heart disease. 1924 American Heart Association is Founded: Six cardiologists form the American Heart Association as a professional society for doctors. -

Changemakers: Biographies of African Americans in San Francisco Who Made a Difference
The University of San Francisco USF Scholarship: a digital repository @ Gleeson Library | Geschke Center Leo T. McCarthy Center for Public Service and McCarthy Center Student Scholarship the Common Good 2020 Changemakers: Biographies of African Americans in San Francisco Who Made a Difference David Donahue Follow this and additional works at: https://repository.usfca.edu/mccarthy_stu Part of the History Commons CHANGEMAKERS AFRICAN AMERICANS IN SAN FRANCISCO WHO MADE A DIFFERENCE Biographies inspired by San Francisco’s Ella Hill Hutch Community Center murals researched, written, and edited by the University of San Francisco’s Martín-Baró Scholars and Esther Madríz Diversity Scholars CHANGEMAKERS: AFRICAN AMERICANS IN SAN FRANCISCO WHO MADE A DIFFERENCE © 2020 First edition, second printing University of San Francisco 2130 Fulton Street San Francisco, CA 94117 Published with the generous support of the Walter and Elise Haas Fund, Engage San Francisco, The Leo T. McCarthy Center for Public Service and the Common Good, The University of San Francisco College of Arts and Sciences, University of San Francisco Student Housing and Residential Education The front cover features a 1992 portrait of Ella Hill Hutch, painted by Eugene E. White The Inspiration Murals were painted in 1999 by Josef Norris, curated by Leonard ‘Lefty’ Gordon and Wendy Nelder, and supported by the San Francisco Arts Commission and the Mayor’s Offi ce Neighborhood Beautifi cation Project Grateful acknowledgment is made to the many contributors who made this book possible. Please see the back pages for more acknowledgments. The opinions expressed herein represent the voices of students at the University of San Francisco and do not necessarily refl ect the opinions of the University or our sponsors. -

Omega Auctions Ltd Catalogue 28 Apr 2020
Omega Auctions Ltd Catalogue 28 Apr 2020 1 REGA PLANAR 3 TURNTABLE. A Rega Planar 3 8 ASSORTED INDIE/PUNK MEMORABILIA. turntable with Pro-Ject Phono box. £200.00 - Approximately 140 items to include: a Morrissey £300.00 Suedehead cassette tape (TCPOP 1618), a ticket 2 TECHNICS. Five items to include a Technics for Joe Strummer & Mescaleros at M.E.N. in Graphic Equalizer SH-8038, a Technics Stereo 2000, The Beta Band The Three E.P.'s set of 3 Cassette Deck RS-BX707, a Technics CD Player symbol window stickers, Lou Reed Fan Club SL-PG500A CD Player, a Columbia phonograph promotional sticker, Rock 'N' Roll Comics: R.E.M., player and a Sharp CP-304 speaker. £50.00 - Freak Brothers comic, a Mercenary Skank 1982 £80.00 A4 poster, a set of Kevin Cummins Archive 1: Liverpool postcards, some promo photographs to 3 ROKSAN XERXES TURNTABLE. A Roksan include: The Wedding Present, Teenage Fanclub, Xerxes turntable with Artemis tonearm. Includes The Grids, Flaming Lips, Lemonheads, all composite parts as issued, in original Therapy?The Wildhearts, The Playn Jayn, Ween, packaging and box. £500.00 - £800.00 72 repro Stone Roses/Inspiral Carpets 4 TECHNICS SU-8099K. A Technics Stereo photographs, a Global Underground promo pack Integrated Amplifier with cables. From the (luggage tag, sweets, soap, keyring bottle opener collection of former 10CC manager and music etc.), a Michael Jackson standee, a Universal industry veteran Ric Dixon - this is possibly a Studios Bates Motel promo shower cap, a prototype or one off model, with no information on Radiohead 'Meeting People Is Easy 10 Min Clip this specific serial number available. -

Vicks® Launches New Nature Fusion™ Line
VICKS® LAUNCHES NEW NATURE FUSION™ LINE Nature Fusion cough, cold and flu products offer the powerful symptom relief, plus real honey for taste Cincinnati, OH, August 11, 2011 – Procter & Gamble’s (NYSE: PG) Vicks brand announced today that it is launching Nature Fusion, a new line of over-the-counter cold, cough and flu relief products that combine powerful symptom relief with real honey for flavor. What inspired Vicks Nature Fusion? Research shows that consumers increasingly desire more natural and less artificial ingredients in their over-the- counter medications, so Vicks is answering the call with Nature Fusion, which joins the powerful science of symptom relief with the best of nature. Beginning with the original Vicks products launched in 1894 which contained Eucalyptus oils from Australia and menthol from Japan, Vicks has a long history of using ingredients inspired by nature. Now, Vicks is continuing this tradition by blending real honey for flavor in new Vicks Nature Fusion. “For more than 120 years, Vicks has helped people feel better by providing proven treatments to deliver effective relief from cold, cough and flu symptoms,” says Andy Cipra, Vicks Brand Manager. “Today, with the launch of Nature Fusion, Vicks is proud to offer the same powerful medicine now flavored with real honey.” Honey has often been favored as a flavor, but lately it has been getting even more buzz as consumers increasingly seek natural ingredients in the products they use. The addition of honey provides aesthetic properties such as flavor, sweetness and thickness. Nature Fusion is also free from alcohol and gluten.