Queensland Ambulance Service Isolated Practice Area Paramedic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Efficacy of Recommended Drugs Against Soil Transmitted Helminths
RESEARCH Efficacy of recommended drugs against soil transmitted BMJ: first published as 10.1136/bmj.j4307 on 25 September 2017. Downloaded from helminths: systematic review and network meta-analysis Wendelin Moser,1,2 Christian Schindler,2,3 Jennifer Keiser1,2 1Department of Medical ABSTRACT 43.4% (23.5% to 63.3%; P=0.049) and the cure rates Parasitology and Infection OBJECTIVE fell from 38.6% (26.2% to 52.7%) to 16.4 (7.7% to Biology, Swiss Tropical and To evaluate efficacies of anthelmintic drugs against 31.3%; P=0.027). Public Health Institute, PO Box, CH-4002 Basel, Switzerland soil transmitted helminths in terms of cure rates and CONCLUSIONS 2University of Basel, Basel, egg reduction rates. All four currently recommended drugs show Switzerland DESIGN limitations in their efficacy profile. While only 3 Department of Epidemiology Systematic review and network meta-analysis. albendazole showed good efficacy against hookworm and Public Health, Swiss Tropical and Public Health DATA SOURCES infection, all drugs had low efficacy againstT trichiura. Institute, PO Box, CH-4002 PubMed, ISI Web of Science, Embase, ScienceDirect, The decrease in efficacy of albendazole againstT Basel, Switzerland the Cochrane Central Register of Clinical Trials, and the trichiura over the past two decades is of concern. The Correspondence to: J Keiser findings indicate the need for strengthening efforts to [email protected] World Health Organization library database from 1960 until 31 December 2016. develop new drug treatments, with a particular focus Additional material is published on drugs against T trichiura. online only. To view please visit STUDY SELECTION the journal online. -

Outcome of Different Therapeutic Interventions in Mild COVID-19 Patients in a Single OPD Clinic of West Bengal: a Retrospective Study
medRxiv preprint doi: https://doi.org/10.1101/2021.03.08.21252883; this version posted March 12, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-ND 4.0 International license . Title page Outcome of Different Therapeutic Interventions in Mild COVID-19 Patients in a Single OPD Clinic of West Bengal: A Retrospective study Running Title: Mild COVID-19 and the Buffet of Treatments: A case series Sayak Roy1, Shambo Samrat Samajdar2, Santanu K Tripathi3, Shatavisa Mukherjee4, Kingshuk Bhattacharjee5 1. Consultant Physician, Dept. of Internal Medicine, Medica Superspeciality Hospital, Kolkata; ORCID ID: https://orcid.org/0000-0002-6185-9375 2. Senior Resident, Dept of Clinical & Experimental Pharmacology, School of Tropical Medicine, Kolkata. 3. Dean (Academics) and Head, Dept of Pharmacology, Netaji Subhash Medical College & Hospital, Bihta, Patna 4. PhD Research Scholar, Dept of Clinical & Experimental Pharmacology, School of Tropical Medicine, Kolkata. ORCID ID: https://orcid.org/0000-0001-9524-1525 5. Independent Biostatistician, Kolkata Corresponding Author: Dr. Sayak Roy 609, G.T.Road, Battala, Serampore, Hooghly, WB, India; PIN – 712201 Email: [email protected] Words: 1906 Tables: 2 References: 20 Informed Consent and Institutional ethical clearance: Taken Conflicts of interest: None Funding: None Acknowledgement: None Data availability: Available on request with the corresponding author NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. 1 medRxiv preprint doi: https://doi.org/10.1101/2021.03.08.21252883; this version posted March 12, 2021. -

O SIEMSGLUSS IBERICA, S.A
SIEMSGLUSS IBERICA, S.A. Product list G Memantine HCI Propylparaben Sodium Pharma APls Gemfibrozil Mepiramina Maleato R Gentian Powder Methoxsalen Ramipril Gentian Violet Methyl Nicotinate Ranitidin HCI Glibenclamide Methylprednisolone Base Rapamycin (Slrollrnus) Glimepiride Metimazole Resorcin A e Gluthatione reduced Metronidazol Resveratrol (Veri-Te®) 11 Alpha Hydroxyprogesterone Caffein Anhydrous Cyproterone Acetate Guaiacol Glyceril Ether Mexiletine HcI Rifampicin 17 Alpha Estradiol Calcipotriol Mieonazole Nitrate o H Roxythromycin Acetyl Salicylic Acid Canrenone Miltefosine Desonide Micronized Hydroquinone AcetylSpiramycin Cantharidin Minocycline HcI Dexamethasone BaseMicro Hyaluronic Acid Sodium Salt s Adapalene Captopril Minoxidil Seenidazol Dexamethasone Isonicotinate Miero Hydrochlorthiazide Amidopyrine Carbamazepine Mometasone Furoato Silver Sulfadiazine Dexamethasone Sodium Phosphate Hydrocortisone Acetate Micro Amikacin Sulphate Carbidopa Montelukast Sodium Simvastatine Dexketoprofen Trometamol Hydrocortisone BaseMicro Amiloride Carisoprodol Sodium Cefonicide Dextrometorphan Bromhidrate Hydroxyzine HcI N Amitriptyline HCI Carvedilol $pironolactone Micro Dextrose (Glucosa) Anhydrous N Aeetyl Glueosamine Amoxlcillin Na + Clavulonate K Cefaclor Monohidrate Sulpiride Diacethyl Naproxen Powder Ibuprofen Amoxicillin Na + Clavulonate K(5:1) Cefadroxil Compaeted Dielofenae Sodium Neutral Pellets Idebenone T Amoxicillin Trihydrate Compacted Cefalexine Monohydrate Powder Difenhydramire Nisin Taerollmus Monohydrate Imiquimod Amoxlcillln -

Exploring the Activity of an Inhibitory Neurosteroid at GABAA Receptors
1 Exploring the activity of an inhibitory neurosteroid at GABAA receptors Sandra Seljeset A thesis submitted to University College London for the Degree of Doctor of Philosophy November 2016 Department of Neuroscience, Physiology and Pharmacology University College London Gower Street WC1E 6BT 2 Declaration I, Sandra Seljeset, confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I can confirm that this has been indicated in the thesis. 3 Abstract The GABAA receptor is the main mediator of inhibitory neurotransmission in the central nervous system. Its activity is regulated by various endogenous molecules that act either by directly modulating the receptor or by affecting the presynaptic release of GABA. Neurosteroids are an important class of endogenous modulators, and can either potentiate or inhibit GABAA receptor function. Whereas the binding site and physiological roles of the potentiating neurosteroids are well characterised, less is known about the role of inhibitory neurosteroids in modulating GABAA receptors. Using hippocampal cultures and recombinant GABAA receptors expressed in HEK cells, the binding and functional profile of the inhibitory neurosteroid pregnenolone sulphate (PS) were studied using whole-cell patch-clamp recordings. In HEK cells, PS inhibited steady-state GABA currents more than peak currents. Receptor subtype selectivity was minimal, except that the ρ1 receptor was largely insensitive. PS showed state-dependence but little voltage-sensitivity and did not compete with the open-channel blocker picrotoxinin for binding, suggesting that the channel pore is an unlikely binding site. By using ρ1-α1/β2/γ2L receptor chimeras and point mutations, the binding site for PS was probed. -

268 Part 522—Implantation Or Injectable Dosage Form
§ 520.2645 21 CFR Ch. I (4–1–18 Edition) (ii) Indications for use. For the control 522.82 Aminopropazine. of American foulbrood (Paenibacillus 522.84 Beta-aminopropionitrile. larvae). 522.88 Amoxicillin. 522.90 Ampicillin injectable dosage forms. (iii) Limitations. The drug should be 522.90a Ampicillin trihydrate suspension. fed early in the spring or fall and con- 522.90b Ampicillin trihydrate powder for in- sumed by the bees before the main jection. honey flow begins, to avoid contamina- 522.90c Ampicillin sodium. tion of production honey. Complete 522.144 Arsenamide. treatments at least 4 weeks before 522.147 Atipamezole. main honey flow. 522.150 Azaperone. 522.161 Betamethasone. [40 FR 13838, Mar. 27, 1975, as amended at 50 522.163 Betamethasone dipropionate and FR 49841, Dec. 5, 1985; 59 FR 14365, Mar. 28, betamethasone sodium phosphate aque- 1994; 62 FR 39443, July 23, 1997; 68 FR 24879, ous suspension. May 9, 2003; 70 FR 69439, Nov. 16, 2005; 73 FR 522.167 Betamethasone sodium phosphate 76946, Dec. 18, 2008; 75 FR 76259, Dec. 8, 2010; and betamethasone acetate. 76 FR 59024, Sept. 23, 2011; 77 FR 29217, May 522.204 Boldenone. 17, 2012; 79 FR 37620, July 2, 2014; 79 FR 53136, 522.224 Bupivacaine. Sept. 8, 2014; 79 FR 64116, Oct. 28, 2014; 80 FR 522.230 Buprenorphine. 34278, June 16, 2015; 81 FR 48702, July 26, 2016] 522.234 Butamisole. 522.246 Butorphanol. § 520.2645 Tylvalosin. 522.275 N-Butylscopolammonium. 522.300 Carfentanil. (a) Specifications. Granules containing 522.304 Carprofen. 62.5 percent tylvalosin (w/w) as 522.311 Cefovecin. -

RIEMSER Group International Product List
RIEMSER Group International Product List Product Active substance Presentation Indication Product Category Channel EMB Fatol Ethambutol • POI 1g/10ml Treatment of several forms and stages of Anti-infectives Rx dihydrochloride • TAB 100mg tuberculosis • FCT 400, 500 mg Eremfat Rifampicin • GRA 1.2g/60ml Anti-infectives Rx • POI 300, 600mg Tuberculosis therapy , combination treatment of • FCT 150, 300, 450, 600 leprosy, prophylaxis for meningococcal meningitis, treatment of infections caused by nontuberculous mycobacteria Isozid Isoniazid • TAB 50, 100, 200 mg During Chemotherapy, -prophylaxis and - Anti-infectives Rx • POI 500mg prevention for / of tuberculosis Isozidcomp Isoniazid / pyridoxine • TAB 100mg / 20mg Chemotherapy, -prophylaxis and -prevention for / Anti-infectives Rx • FCT 200mg /40 mg, 300mg/60mg of Tuberculosis PAS-Fatol Sodium aminosalicylate • POI 13.49g Chemotherapy for tuberculosis, caused by Anti-infectives Rx dihydrate mycobacterium tuberculosis and mycobacterium bovis. Peteha Protionamide • FCT 250mg Treatment of tuberculosis, leprosy and diseases Anti-infectives Rx caused by so-called ubiquitours (atypical) mycobacteria Pyrafat Pyrazinamide • FCT 500mg Combination therapy for all types of tuberculosis, Anti-infectives Rx • TAB 500mg caused by mycobacterium tuberculosis, mycobacterium africanum, or mycobacterium microtti. Terizidon Terizidone • CAP 250mg Treatment of tuberculosis caused by Anti-infectives Rx mycobacterium tuberculosis Vancomycin Enterocaps Vancomycin • CAP 250 mg Treatment of certain types of bowel -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Review Article a BRIEF REVIEW on the MODE of ACTION of ANTINEMATODAL DRUGS
Acta Veterinaria-Beograd 2017, 67 (2), 137-152 UDK: 615.284.03 DOI: 10.1515/acve-2017-0013 Review article A BRIEF REVIEW ON THE MODE OF ACTION OF ANTINEMATODAL DRUGS ABONGWA Melanie, MARTIN Richard J., ROBERTSON Alan P.* Department of Biomedical Sciences, College of Veterinary Medicine, Iowa State University, Ames, IA 50011, USA (Received 01 May, Accepted 24 May 2017) Anthelmintics are some of the most widely used drugs in veterinary medicine. Here we review the mechanism of action of these compounds on nematode parasites. Included are the older classes of compounds; the benzimidazoles, cholinergic agonists and macrocyclic lactones. We also consider newer anthelmintics, including emodepside, derquantel and tribendimidine. In the absence of vaccines for most parasite species, control of nematode parasites will continue to rely on anthelmintic drugs. As a consequence, vigilance in detecting drug resistance in parasite populations is required. Since resistance development appears almost inevitable, there is a continued and pressing need to fully understand the mode of action of these compounds. It is also necessary to identify new drug targets and drugs for the continued effective control of nematode parasites. Key words: anthelmintic, parasite, benzimidazoles, avermectins, cholinergic, emodepside, derquantel INTRODUCTION Anthelmintics are drugs that are used to treat infections caused by parasitic worms (helminths) [1]. There are three major groups of helminths namely: nematodes (roundworms), trematodes (fl ukes) and cestodes (tapeworms). These groups of helminths are divided into two phyla; nematodes (roundworms) and platyhelminths (trematodes and cestodes) [2]. Anthelmintics either kill worms or cause their expulsion from the body, without causing any signifi cant damage to the host [3]. -

WSAVA List of Essential Medicines for Cats and Dogs
The World Small Animal Veterinary Association (WSAVA) List of Essential Medicines for Cats and Dogs Version 1; January 20th, 2020 Members of the WSAVA Therapeutic Guidelines Group (TGG) Steagall PV, Pelligand L, Page SW, Bourgeois M, Weese S, Manigot G, Dublin D, Ferreira JP, Guardabassi L © 2020 WSAVA All Rights Reserved Contents Background ................................................................................................................................... 2 Definition ...................................................................................................................................... 2 Using the List of Essential Medicines ............................................................................................ 2 Criteria for selection of essential medicines ................................................................................. 3 Anaesthetic, analgesic, sedative and emergency drugs ............................................................... 4 Antimicrobial drugs ....................................................................................................................... 7 Antibacterial and antiprotozoal drugs ....................................................................................... 7 Systemic administration ........................................................................................................ 7 Topical administration ........................................................................................................... 9 Antifungal drugs ..................................................................................................................... -
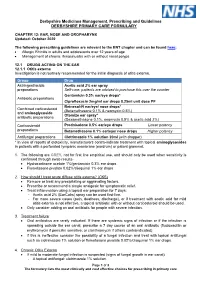
EAR, NOSE and OROPHARYNX Updated: October 2020
Derbyshire Medicines Management, Prescribing and Guidelines DERBYSHIRE PRIMARY CARE FORMULARY CHAPTER 12: EAR, NOSE AND OROPHARYNX Updated: October 2020 The following prescribing guidelines are relevant to the ENT chapter and can be found here: • Allergic Rhinitis in adults and adolescents over 12 years of age • Management of chronic rhinosinusitis with or without nasal polyps 12.1 DRUGS ACTING ON THE EAR 12.1.1 Otitis externa Investigation is not routinely recommended for the initial diagnosis of otitis externa. Group Drug Astringent/acidic Acetic acid 2% ear spray preparations Self-care: patients are advised to purchase this over the counter Gentamicin 0.3% ear/eye drops* Antibiotic preparations Ciprofloxacin 2mg/ml ear drops 0.25ml unit dose PF Betnesol-N ear/eye/ nose drops* Combined corticosteroid (Betamethasone 0.1% & neomycin 0.5%) and aminoglycoside Otomize ear spray* antibiotic preparations (Dexamethasone 0.1%, neomycin 0.5% & acetic acid 2%) Corticosteroid Prednisolone 0.5% ear/eye drops Lower potency preparations Betamethasone 0.1% ear/eye/ nose drops Higher potency Antifungal preparations Clotrimazole 1% solution 20ml (with dropper) * In view of reports of ototoxicity, manufacturers contra-indicate treatment with topical aminoglycosides in patients with a perforated tympanic membrane (eardrum) or patent grommet. 1. The following are GREY, not for first line empirical use, and should only be used when sensitivity is confirmed through swab results- • Hydrocortisone acetate 1%/gentamicin 0.3% ear drops • Flumetasone pivalate 0.02%/clioquinol 1% ear drops 2. How should I treat acute diffuse otitis externa? (CKS) • Remove or treat any precipitating or aggravating factors. • Prescribe or recommend a simple analgesic for symptomatic relief. -

A Pilot Study of the Safety and Initial Efficacy of Ivermectin for The
ALCOHOLISM:CLINICAL AND EXPERIMENTAL RESEARCH Vol. 40, No. 6 June 2016 A Pilot Study of the Safety and Initial Efficacy of Ivermectin for the Treatment of Alcohol Use Disorder Daniel J. O. Roche, Megan M. Yardley, Katy F. Lunny, Stan G. Louie, Daryl L. Davies, Karen Miotto, and Lara A. Ray Background: Ivermectin (IVM) is an antiparasitic agent that has been shown to reduce alcohol intake in mice, suggesting IVM as a potential treatment for alcohol use disorder (AUD). However, the safety profile of IVM administered in combination with an intoxicating dose of alcohol has not been characterized in humans. Methods: This pilot project sought to provide the first clinical evidence that IVM could be reposi- tioned as an AUD pharmacotherapy by examining (i) the safety of combining IVM (30 mg oral , once a day [QD]) with an intoxicating dose of intravenous alcohol (0.08 g/dl) and (ii) the effects of IVM on alcohol cue-induced craving and subjective response to alcohol. Eleven individuals with AUD partici- pated in a randomized, placebo-controlled, crossover study in which they received the study medica- tion, participated in a cue exposure paradigm followed by intravenous alcohol administration, and remained in an inpatient unit overnight for observation. Results: IVM treatment, versus placebo, did not increase the number or severity of adverse effects during alcohol administration or throughout the visit. However, IVM did not reduce cue-induced crav- ing nor did it significantly affect subjective response to alcohol. Conclusions: These results suggest that IVM (30 mg oral, QD) is safe in combination with an intoxi- cating dose of alcohol, but do not provide evidence that this dose of IVM is effective in reducing alcohol craving or its reinforcing effects. -

Ivermectin and Human Immunity Protocol ID
Cover Sheet Clinicaltrials.gov ID NCT03459794 Protocol Ivermectin and human immunity ID#STUDY00005069 Adrian Adrian PI: Primary Contact: Wolstenholme Wolstenholme Submission Initial Study Type: IRB Brooke Harwell Parent Protocol: Coordinator: Review Category: Approved 9/27/2017 Date: Expiration 7/11/2018 Date: Print: STUDY00005069 - Ivermectin and human immunity https://ovpr-click-prod.ovpr.uga.edu/uga-ovpr/ResourceAdministration/P... Date: Monday, November 26, 2018 12:06:50 PM View: SF: Basic Information UGA v2 Section 1 - Basic Information 1. * Title of Study: If the study is/will be funded, the IRB recommends The effects of ivermectin on the normal human matching the title in the funding proposal. immune system 2. * Short Title: This can match the long title or be shortened if your Ivermectin and human immunity project uses an acronym or nickname; however, all system generated lists, searches, and documents (including approval letters) will show the short title. 3. Only UGA faculty and selected staff members (senior Principal Investigator (faculty or senior staff) are eligible to serve as PI. See the policy for staff only - see help): more information: http://research.uga.edu/documents Adrian Wolstenholme /eligibility 4. * Does the Principal Investigator have a See the policy for more information: https://research.uga.edu/docs/policies financial interest related to this /compliance research? Yes No /hso/PP_Financial%20Conflicts%20of%20Interests.pdf 5. If you are not sure if your project needs IRB * Are you requesting determination if review, choose "Yes" in the first question. A form will your project meets the definition of open and provide prompts to guide you through an initial assessment to see if your project needs IRB Yes No human subjects research? review.