Addressing the Issue of Missing Heritability: the Importance of Apoptosis in Hereditary Breast and Ovarian Cancer and Functional Assessment of Tp53i3-S252*
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
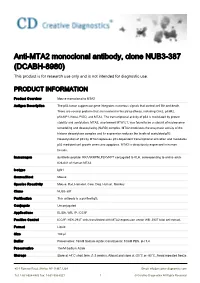
Anti-MTA2 Monoclonal Antibody, Clone NUB3-387 (DCABH-8980) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-MTA2 monoclonal antibody, clone NUB3-387 (DCABH-8980) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Mouse monoclonal to MTA2 Antigen Description The p53 tumor suppressor gene integrates numerous signals that control cell life and death. There are several proteins that are involved in the p53 pathway, including Chk2, p53R2, p53AIP1, Noxa, PIDD, and MTA2. The transcriptional activity of p53 is modulated by protein stability and acetylation. MTA2, also termed MTA1L1, was found to be a subunit of nucleosome remodeling and deacetylating (NuRD) complex. MTA2 modulates the enzymatic activity of the histone deacetylase complex and its expression reduces the levels of acetylated p53. Deacetylation of p53 by MTA2 represses p53 dependent transcriptional activation and modulates p53 mediated cell growth arrest and apoptosis. MTA2 is ubiquitously expressed in human tissues. Immunogen Synthetic peptide: RRAARRPNLPLKVKPT conjugated to KLH, corresponding to amino acids 626-641 of Human MTA2 Isotype IgG1 Source/Host Mouse Species Reactivity Mouse, Rat, Hamster, Cow, Dog, Human, Monkey Clone NUB3-387 Purification This antibody is a purified IgG. Conjugate Unconjugated Applications ELISA, WB, IP, ICC/IF Positive Control ICC/IF: HEK-293T cells transfected with MTA2 expression vector WB: 293T total cell extract. Format Liquid Size 100 μl Buffer Preservative: 15mM Sodium Azide; Constituents: 10mM PBS, pH 7.4 Preservative 15mM Sodium Azide Storage Store at +4°C short term (1-2 weeks). Aliquot and store at -20°C or -80°C. Avoid repeated freeze 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved / thaw cycles. -

Whole Exome Sequencing in Families at High Risk for Hodgkin Lymphoma: Identification of a Predisposing Mutation in the KDR Gene
Hodgkin Lymphoma SUPPLEMENTARY APPENDIX Whole exome sequencing in families at high risk for Hodgkin lymphoma: identification of a predisposing mutation in the KDR gene Melissa Rotunno, 1 Mary L. McMaster, 1 Joseph Boland, 2 Sara Bass, 2 Xijun Zhang, 2 Laurie Burdett, 2 Belynda Hicks, 2 Sarangan Ravichandran, 3 Brian T. Luke, 3 Meredith Yeager, 2 Laura Fontaine, 4 Paula L. Hyland, 1 Alisa M. Goldstein, 1 NCI DCEG Cancer Sequencing Working Group, NCI DCEG Cancer Genomics Research Laboratory, Stephen J. Chanock, 5 Neil E. Caporaso, 1 Margaret A. Tucker, 6 and Lynn R. Goldin 1 1Genetic Epidemiology Branch, Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD; 2Cancer Genomics Research Laboratory, Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD; 3Ad - vanced Biomedical Computing Center, Leidos Biomedical Research Inc.; Frederick National Laboratory for Cancer Research, Frederick, MD; 4Westat, Inc., Rockville MD; 5Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD; and 6Human Genetics Program, Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD, USA ©2016 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol.2015.135475 Received: August 19, 2015. Accepted: January 7, 2016. Pre-published: June 13, 2016. Correspondence: [email protected] Supplemental Author Information: NCI DCEG Cancer Sequencing Working Group: Mark H. Greene, Allan Hildesheim, Nan Hu, Maria Theresa Landi, Jennifer Loud, Phuong Mai, Lisa Mirabello, Lindsay Morton, Dilys Parry, Anand Pathak, Douglas R. Stewart, Philip R. Taylor, Geoffrey S. Tobias, Xiaohong R. Yang, Guoqin Yu NCI DCEG Cancer Genomics Research Laboratory: Salma Chowdhury, Michael Cullen, Casey Dagnall, Herbert Higson, Amy A. -

Regulation of Apoptosis by P53-Inducible Transmembrane Protein Containing Sushi Domain
1193-1200.qxd 24/9/2010 08:07 Ì ™ÂÏ›‰·1193 ONCOLOGY REPORTS 24: 1193-1200, 2010 Regulation of apoptosis by p53-inducible transmembrane protein containing sushi domain HONGYAN CUI, HIROKI KAMINO, YASUYUKI NAKAMURA, NORIAKI KITAMURA, TAKAFUMI MIYAMOTO, DAISUKE SHINOGI, OLGA GODA, HIROFUMI ARAKARA and MANABU FUTAMURA Cancer Medicine and Biophysics Division, National Cancer Center Research Institute, 5-1-1 Tsukiji, Chuo-ku, Tokyo 104-0045, Japan Received January 14, 2010; Accepted March 30, 2010 DOI: 10.3892/or_00000972 Abstract. The tumor suppressor p53 is a transcription factor repair, apoptosis, and anti-angiogenesis (1,2). The p21/waf1 that induces the transcription of various target genes in gene is considered to be one of the most important p53 target response to DNA damage and it protects the cells from genes because it is essential for p53-dependent cell cycle malignant transformation. In this study, we performed cDNA arrest at G1. p53R2, which supplies nucleotides for DNA microarray analysis and found that the transmembrane protein synthesis, facilitates the repair of DNA damage. Several containing sushi domain (TMPS) gene, which encodes a mitochondrial proteins including BAX, Noxa, and p53- putative type I transmembrane protein, is a novel p53-target regulated apoptosis-inducing protein 1 (p53AIP1) contribute gene. TMPS contains a sushi domain in the extracellular to the release of cytochrome c from mitochondria. Other region, which is associated with protein-protein interaction. proteins such as Fas/ApoI and unc-5 homolog B (UNC5B) TMPS expression is induced by endogenous p53 under geno- are also associated with apoptosis. Brain-specific angio- toxic stress in several cancer cell lines. -
Open Full Page
Author Manuscript Published OnlineFirst on March 9, 2017; DOI: 10.1158/0008-5472.CAN-16-2339 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Title Page Title: Pancreatic cancer progression relies upon mutant p53-induced oncogenic signaling mediated by NOP14 Yongxing Du1,§, Ziwen Liu1, §, Lei You1, Pengjiao Hou2, Xiaoxia Ren1, Tao Jiao2, Wenjing Zhao1, Zongze Li1, Hong Shu1, Changzheng Liu2,*, Yupei Zhao1,* 1 Department of General Surgery, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Peking Union Medical College, Beijing 100730, PR China 2 Department of Biochemistry and Molecular Biology, State Key Laboratory of Medical Molecular Biology, Institute of Basic Medical Sciences, Chinese Academy of Medical Sciences,School of Basic Medicine, Peking Union Medical College, Beijing 100005, PR China § Authors share co-first authorship. * To whom correspondence should be addressed: Yupei Zhao, E-mail: [email protected], Fax: 86-10-65124875; Changzheng Liu, E-mail: [email protected], Fax: 86-10-65253005. Running Title: NOP14 primes mutp53-driven cancer progression Key words: Pancreatic ductal adenocarcinoma, Mutant p53, NOP14, Cancer metastasis Abbreviations: Mutp53, Mutant p53; PDAC, Pancreatic ductal adenocarcinoma; NOP14, NOP14 nucleolar protein; rRNA, ribosomal RNA; PDGFRb, Platelet-derived 1 Downloaded from cancerres.aacrjournals.org on September 26, 2021. © 2017 American Association for Cancer Research. Author Manuscript Published OnlineFirst on March 9, -

Role and Regulation of the P53-Homolog P73 in the Transformation of Normal Human Fibroblasts
Role and regulation of the p53-homolog p73 in the transformation of normal human fibroblasts Dissertation zur Erlangung des naturwissenschaftlichen Doktorgrades der Bayerischen Julius-Maximilians-Universität Würzburg vorgelegt von Lars Hofmann aus Aschaffenburg Würzburg 2007 Eingereicht am Mitglieder der Promotionskommission: Vorsitzender: Prof. Dr. Dr. Martin J. Müller Gutachter: Prof. Dr. Michael P. Schön Gutachter : Prof. Dr. Georg Krohne Tag des Promotionskolloquiums: Doktorurkunde ausgehändigt am Erklärung Hiermit erkläre ich, dass ich die vorliegende Arbeit selbständig angefertigt und keine anderen als die angegebenen Hilfsmittel und Quellen verwendet habe. Diese Arbeit wurde weder in gleicher noch in ähnlicher Form in einem anderen Prüfungsverfahren vorgelegt. Ich habe früher, außer den mit dem Zulassungsgesuch urkundlichen Graden, keine weiteren akademischen Grade erworben und zu erwerben gesucht. Würzburg, Lars Hofmann Content SUMMARY ................................................................................................................ IV ZUSAMMENFASSUNG ............................................................................................. V 1. INTRODUCTION ................................................................................................. 1 1.1. Molecular basics of cancer .......................................................................................... 1 1.2. Early research on tumorigenesis ................................................................................. 3 1.3. Developing -

Mutational Profile and Prognostic Significance of TP53 in Diffuse Large
LYMPHOID NEOPLASIA Mutational profile and prognostic significance of TP53 in diffuse large B-cell lymphoma patients treated with R-CHOP: report from an International DLBCL Rituximab-CHOP Consortium Program Study Zijun Y. Xu-Monette,1 Lin Wu,2 Carlo Visco,3 Yu Chuan Tai,2 Alexander Tzankov,4 Wei-min Liu,2 Santiago Montes-Moreno,5 Karen Dybkær,6 April Chiu,7 Attilio Orazi,8 Youli Zu,9 Govind Bhagat,10 Kristy L. Richards,11 Eric D. Hsi,12 X. Frank Zhao,13 William W. L. Choi,14 Xiaoying Zhao,15 J. Han van Krieken,16 Qin Huang,17 Jooryung Huh,18 Weiyun Ai,19 Maurilio Ponzoni,20 Andre´s J. M. Ferreri,20 Fan Zhou,21 Brad S. Kahl,22 Jane N. Winter,23 Wei Xu,24 Jianyong Li,24 Ronald S. Go,25 Yong Li,26 Miguel A. Piris,5 Michael B. Møller,27 Roberto N. Miranda,1 Lynne V. Abruzzo,1 L. Jeffrey Medeiros,1 and Ken H. Young1 1Department of Hematopathology, The University of Texas MD Anderson Cancer Center, Houston, TX; 2Roche Molecular Systems Inc, Pleasanton, CA; 3San Bortolo Hospital, Vicenza, Italy; 4University Hospital, Basel, Switzerland; 5Hospital Universitario Marques de Valdecilla, Santander, Spain; 6Aalborg Hospital, Aarhus University Hospital, Aalborg, Denmark; 7Memorial Sloan-Kettering Cancer Center, New York, NY; 8Weill Medical College of Cornell University, New York, NY; 9The Methodist Hospital, Houston, TX; 10Columbia University Medical Center and New York Presbyterian Hospital, New York, NY; 11University of North Carolina School of Medicine, Chapel Hill, NC; 12Cleveland Clinic, Cleveland, OH; 13University of Maryland School of Medicine, Baltimore, MD; 14University of Hong Kong Li Ka Shing Faculty of Medicine, Hong Kong, China; 15Zhejiang University School of Medicine, Second University Hospital, Hangzhou, China; 16Radboud University Nijmegen Medical Centre, Nijmegen, Netherlands; 17City of Hope National Medical Center, Duarte, CA; 18Asan Medical Center, Ulsan University College of Medicine, Seoul, Korea; 19University of California-San Francisco School of Medicine, San Francisco, CA; 20San Raffaele H. -

P53aip1 Regulates the Mitochondrial Apoptotic Pathway1
[CANCER RESEARCH 62, 2883–2889, May 15, 2002] p53AIP1 Regulates the Mitochondrial Apoptotic Pathway1 Koichi Matsuda, Koji Yoshida, Yoichi Taya, Kozo Nakamura, Yusuke Nakamura,2 and Hirofumi Arakawa Human Genome Center, Institute of Medical Science, University of Tokyo, Minato-ku, Tokyo 108-8639 [K. M., K. Y., Y. N., H. A.], and Department of Orthopedic Surgery, Faculty of Medicine, University of Tokyo, Bunkyo-ku, Tokyo 113-0033 [K. M., K. N.], and National Cancer Center Research Institute, Chuo-ku, Tokyo 104-0045 [Y.T.], Japan ABSTRACT family have been reported as anti- or proapoptotic players; all of them possess at least one of the four domains. We identified recently the p53AIP1 gene, a novel p53 target that Although p53-dependent apoptosis is thought to be the most im- mediates p53-dependent apoptosis. In the experiments reported here, portant feature of tumor suppression by p53, a large part of that ectopic expression of p53AIP1 induced down-regulation of mitochondrial ⌬⌿m and release of cytochrome c from mitochondria in human cells. mechanism remains to be explained. Several target genes have been Immunoprecipitation and immunostaining experiments indicated interac- isolated as attractive candidates for p53-dependent apoptosis, includ- tion between p53AIP1 and bcl-2 proteins at mitochondria. Overexpression ing bax (23), PIG3 (24, 25), Killer/DR5 (26), Fas (27, 28), Noxa (29), of bcl-2 blocked the down-regulation of mitochondrial ⌬⌿m and the PERP (30), and PUMA (31, 32). Bax, Noxa, and PUMA are mito- proapoptotic activity of p53AIP1. Our results implicate p53AIP1 as a chondrial proteins and members of the bcl-2 family, because they pivotal mediator of the p53-dependent mitochondrial apoptotic pathway. -
Identification of Differential Expression of P53 Associated Rnas at 3 Different Treatment Timepoints, and Association with Chip- Seq Identified P53 Genes
Rochester Institute of Technology RIT Scholar Works Theses 5-19-2017 Identification of Differential Expression of p53 associated RNAs at 3 Different Treatment Timepoints, and Association with ChIP- seq Identified p53 Genes. Julia Freewoman [email protected] Follow this and additional works at: https://scholarworks.rit.edu/theses Recommended Citation Freewoman, Julia, "Identification of Differential Expression of p53 associated RNAs at 3 Different Treatment Timepoints, and Association with ChIP-seq Identified p53 Genes." (2017). Thesis. Rochester Institute of Technology. Accessed from This Thesis is brought to you for free and open access by RIT Scholar Works. It has been accepted for inclusion in Theses by an authorized administrator of RIT Scholar Works. For more information, please contact [email protected]. R.I.T. Identification of Differential Expression of p53 associated RNAs at 3 Different Treatment Timepoints, and Association with ChIP-seq Identified p53 Genes. by Julia Freewoman A Thesis Submitted in Partial Fulfillment of the Requirements for the Degree of Master of Science in Bioinformatics. School of Thomas H. Gosnell School of Life Sciences Bioinformatics Program College of Science Rochester Institute of Technology Rochester, NY May 19, 2017 Thesis Committee Members: Feng Cui, Ph.D., thesis advisor Andre Hudson, Ph.D. Gary R. Skuse, Ph.D. ii Table of Contents Abstract ........................................................................................................................................... 1 I. Introduction -

The Pseudo-Caspase FLIP(L) Regulates Cell Fate Following P53 Activation
The pseudo-caspase FLIP(L) regulates cell fate following p53 activation Andrea Leesa,1, Alexander J. McIntyrea,1, Nyree T. Crawforda, Fiammetta Falconea, Christopher McCanna, Caitriona Holohana, Gerard P. Quinna, Jamie Z. Robertsa, Tamas Sesslera, Peter F. Gallaghera, Gemma M. A. Gregga, Katherine McAllistera, Kirsty M. McLaughlina, Wendy L. Allena, Laurence J. Eganb, Aideen E. Ryanb,c, Melissa J. Labonte-Wilsona, Philip D. Dunnea, Mark Wappetta, Vicky M. Coylea, Patrick G. Johnstona, Emma M. Kerra, Daniel B. Longleya,2,3, and Simon S. McDadea,2,3 aPatrick G Johnston Centre for Cancer Research, Queen’s University Belfast, Belfast, Northern Ireland BT9 7BL, United Kingdom; bDiscipline of Pharmacology & Therapeutics, Lambe Institute for Translational Research, School of Medicine, College of Medicine, Nursing and Health Sciences, National University of Ireland Galway, Galway, Ireland; and cRegenerative Medicine Institute, College of Medicine, Nursing and Health Sciences, National University of Ireland Galway, Galway, Ireland Edited by Karen H. Vousden, Francis Crick Institute, London, United Kingdom, and approved June 8, 2020 (received for review February 12, 2020) p53 is the most frequently mutated, well-studied tumor-suppressor switch from cell-cycle arrest to cell death induction remain gene, yet the molecular basis of the switch from p53-induced cell- poorly understood, although p53-mediated transcriptional up- cycle arrest to apoptosis remains poorly understood. Using a combi- regulation of PUMA has been suggested to be crucial in a nation of transcriptomics and functional genomics, we unexpectedly number of studies (10, 11). identified a nodal role for the caspase-8 paralog and only human Despite p53/TP53 being the most frequently mutated gene in pseudo-caspase, FLIP(L), in regulating this switch. -

Downregulation of SNRPG Induces Cell Cycle Arrest and Sensitizes Human Glioblastoma Cells to Temozolomide by Targeting Myc Through a P53-Dependent Signaling Pathway
Cancer Biol Med 2020. doi: 10.20892/j.issn.2095-3941.2019.0164 ORIGINAL ARTICLE Downregulation of SNRPG induces cell cycle arrest and sensitizes human glioblastoma cells to temozolomide by targeting Myc through a p53-dependent signaling pathway Yulong Lan1,2*, Jiacheng Lou2*, Jiliang Hu1, Zhikuan Yu1, Wen Lyu1, Bo Zhang1,2 1Department of Neurosurgery, Shenzhen People’s Hospital, Second Clinical Medical College of Jinan University, The First Affiliated Hospital of Southern University of Science and Technology, Shenzhen 518020, China;2 Department of Neurosurgery, The Second Affiliated Hospital of Dalian Medical University, Dalian 116023, China ABSTRACT Objective: Temozolomide (TMZ) is commonly used for glioblastoma multiforme (GBM) chemotherapy. However, drug resistance limits its therapeutic effect in GBM treatment. RNA-binding proteins (RBPs) have vital roles in posttranscriptional events. While disturbance of RBP-RNA network activity is potentially associated with cancer development, the precise mechanisms are not fully known. The SNRPG gene, encoding small nuclear ribonucleoprotein polypeptide G, was recently found to be related to cancer incidence, but its exact function has yet to be elucidated. Methods: SNRPG knockdown was achieved via short hairpin RNAs. Gene expression profiling and Western blot analyses were used to identify potential glioma cell growth signaling pathways affected by SNRPG. Xenograft tumors were examined to determine the carcinogenic effects of SNRPG on glioma tissues. Results: The SNRPG-mediated inhibitory effect on glioma cells might be due to the targeted prevention of Myc and p53. In addition, the effects of SNRPG loss on p53 levels and cell cycle progression were found to be Myc-dependent. Furthermore, SNRPG was increased in TMZ-resistant GBM cells, and downregulation of SNRPG potentially sensitized resistant cells to TMZ, suggesting that SNRPG deficiency decreases the chemoresistance of GBM cells to TMZ via the p53 signaling pathway. -

PIG3 (TP53I3) Rabbit Polyclonal Antibody – TA308561 | Origene
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for TA308561 PIG3 (TP53I3) Rabbit Polyclonal Antibody Product data: Product Type: Primary Antibodies Applications: IF, IHC, WB Recommended Dilution: ICC/IF:1:100-1:1000; IHC:1:100-1:1000; WB:1:500-1:3000 Reactivity: Human (Predicted: Bovine) Host: Rabbit Isotype: IgG Clonality: Polyclonal Immunogen: Recombinant fragment corresponding to a region within amino acids 1 and 332 of PIG3 (Uniprot ID#Q53FA7) Formulation: 0.1M Tris, 0.1M Glycine, 10% Glycerol (pH7). 0.01% Thimerosal was added as a preservative. Purification: Purified by antigen-affinity chromatography. Conjugation: Unconjugated Storage: Store at -20°C as received. Stability: Stable for 12 months from date of receipt. Predicted Protein Size: 36 kDa Gene Name: tumor protein p53 inducible protein 3 Database Link: NP_004872 Entrez Gene 9540 Human Q53FA7 This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 3 PIG3 (TP53I3) Rabbit Polyclonal Antibody – TA308561 Background: The protein encoded by this gene is similar to oxidoreductases, which are enzymes involved in cellular responses to oxidative stresses and irradiation. This gene is induced by the tumor suppressor p53 and is thought to be involved in p53-mediated cell death. It contains a p53 consensus binding site in its promoter region and a downstream pentanucleotide microsatellite sequence. P53 has been shown to transcriptionally activate this gene by interacting with the downstream pentanucleotide microsatellite sequence. -

The P53mh Algorithm and Its Application in Detecting P53-Responsive Genes
The p53MH algorithm and its application in detecting p53-responsive genes J. Hoh*†‡, S. Jin§†, T. Parrado*, J. Edington*, A. J. Levine§, and J. Ott* *Laboratories of Statistical Genetics and §Cancer Biology of The Rockefeller University, 1230 York Avenue, New York, NY 10021 Contributed by A. J. Levine, May 6, 2002 A computer algorithm, p53MH, was developed, which identifies overall binding likelihood is needed for a given gene of arbitrary putative p53 transcription factor DNA-binding sites on a genome- size. Three features have been implemented in an algorithm to wide scale with high power and versatility. With the sequences meet the above requirements: binding propensity plots, weighted from the human and mouse genomes, putative p53 DNA-binding scores, and statistical significance for most likely binding sites. elements were identified in a scan of 2,583 human genes and 1,713 This computer algorithm has been used to identify putative mouse orthologs based on the experimental data of el-Deiry et al. binding elements on a genomewide scale. The algorithm, [el-Deiry, W. S., Kern, S. E., Pietenpol, J. A., Kinzler, K. W. & p53MH, uses an optimal scoring system as an indication of the Vogelstein, B. (1992) Nat. Genet. 1, 45–49] and Funk et al. [Funk, percent similarity to the consensus. It can simultaneously screen W. D., Pak, D. T., Karas, R. H., Wright, W. E. & Shay, J. W. (1992) Mol. thousands of genes for degenerate consensus sequences in the Cell. Biol. 12, 2866–2871] (http:͞͞linkage.rockefeller.edu͞p53). The course of only a few minutes. With this, based on the available p53 DNA-binding motif consists of a 10-bp palindrome and most annotated human sequence databases, a White Page-like direc- commonly a second related palindrome linked by a spacer region.