(Raav)-Vector Elements in Ocular Gene Therapy Clinical Trials and Transgene Expression and Bioactivity Assays
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Peropsin, a Novel Visual Pigment-Like Protein Located in the Apical Microvilli of the Retinal Pigment Epithelium
Proc. Natl. Acad. Sci. USA Vol. 94, pp. 9893–9898, September 1997 Neurobiology Peropsin, a novel visual pigment-like protein located in the apical microvilli of the retinal pigment epithelium HUI SUN*, DEBRA J. GILBERT†,NEAL G. COPELAND†,NANCY A. JENKINS†, AND JEREMY NATHANS*‡§¶i *Department of Molecular Biology and Genetics, §Department of Neuroscience, ¶Department of Ophthalmology, ‡Howard Hughes Medical Institute, Johns Hopkins University School of Medicine, Baltimore, MD 21205; and †Mammalian Genetics Laboratory, Advanced BioScience Laboratories Basic Research Program, National Cancer Institute–Frederick Cancer Research and Development Center, Frederick, MD 21702 Contributed by Jeremy Nathans, June 19, 1997 ABSTRACT A visual pigment-like protein, referred to as bovine RPE binds to all-trans but not 11-cis retinal and absorbs peropsin, has been identified by large-scale sequencing of both visible and ultraviolet light (8, 9). The sequences of cDNAs derived from human ocular tissues. The corresponding retinochrome and RGR opsin form a distinct and highly mRNA was found only in the eye, where it is localized to the divergent branch within the visual pigment family (6, 10). retinal pigment epithelium (RPE). Peropsin immunoreactiv- Whether retinochrome and RGR act as signal-transducing ity, visualized by light and electron microscopy, localizes the light receptors, participate in the visual cycle as retinal isomer- protein to the apical face of the RPE, and most prominently ases, or function in both capacities, is not known. to the microvilli that surround the photoreceptor outer seg- In the vertebrate eye, the RPE lies adjacent to the photo- ments. These observations suggest that peropsin may play a receptor cells and performs a number of functions critical for role in RPE physiology either by detecting light directly or by the viability and activity of the retina (11). -

The Vertebrate Retina Contains Two Types of Photoreceptors: Rods That
JOURNAL OF NEUROCHEMISTRY | 2009 | 108 | 91–101 doi: 10.1111/j.1471-4159.2008.05739.x *Department of Anatomy, School of Medicine, Tokyo Women’s Medical University, Tokyo, Japan Genetics and Development Division, Toronto Western Research Institute, University Health Network, Department of Ophthalmology and Visual Sciences and Department of Laboratory Medicine and Pathobiology, University of Toronto, Toronto, Ontario, Canada àUniversity of Ottawa Eye Institute and Ottawa Health Research Institute, Ottawa, Ontario, Canada Abstract The retinas of staggerer mice, carrying a null mutation of Color vision is supported by retinal cone photoreceptors that, RORa, show significant down-regulation of Opn1sw, in most mammals, express two photopigments sensitive to Opn1mw, and Arr3. RORa acts in synergy with cone-rod short (S-opsin) or middle (M-opsin) wavelengths. Expression homeobox transcription factor (Crx), to activate the Opn1sw of the Opn1sw and Opn1mw genes, encoding S-opsin and promoter in vitro. Chromatin immunoprecipitation assays re- M-opsin, respectively, is under the control of nuclear veal that RORa directly binds to the Opn1sw promoter, receptors, including thyroid hormone receptor b2 (TRb2), Opn1mw locus control region, and the Arr3 promoter in vivo. retinoid X receptor c (RXRc), and RORb, a member of the Our data suggest that RORa plays a crucial role in cone retinoic acid receptor-related orphan receptor (ROR) family. development by directly regulating multiple cone genes. We now demonstrate that RORa, another member of the ROR Keywords: arrestin, cone photoreceptor, opsin, retina, family, regulates Opn1sw, Opn1mw, as well as Arr3 (cone RORa, staggerer. arrestin) in the mouse retina. RORa expression is detected in J. -
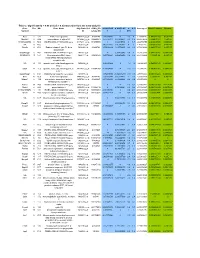
Table 2. Significant
Table 2. Significant (Q < 0.05 and |d | > 0.5) transcripts from the meta-analysis Gene Chr Mb Gene Name Affy ProbeSet cDNA_IDs d HAP/LAP d HAP/LAP d d IS Average d Ztest P values Q-value Symbol ID (study #5) 1 2 STS B2m 2 122 beta-2 microglobulin 1452428_a_at AI848245 1.75334941 4 3.2 4 3.2316485 1.07398E-09 5.69E-08 Man2b1 8 84.4 mannosidase 2, alpha B1 1416340_a_at H4049B01 3.75722111 3.87309653 2.1 1.6 2.84852656 5.32443E-07 1.58E-05 1110032A03Rik 9 50.9 RIKEN cDNA 1110032A03 gene 1417211_a_at H4035E05 4 1.66015788 4 1.7 2.82772795 2.94266E-05 0.000527 NA 9 48.5 --- 1456111_at 3.43701477 1.85785922 4 2 2.8237185 9.97969E-08 3.48E-06 Scn4b 9 45.3 Sodium channel, type IV, beta 1434008_at AI844796 3.79536664 1.63774235 3.3 2.3 2.75319499 1.48057E-08 6.21E-07 polypeptide Gadd45gip1 8 84.1 RIKEN cDNA 2310040G17 gene 1417619_at 4 3.38875643 1.4 2 2.69163229 8.84279E-06 0.0001904 BC056474 15 12.1 Mus musculus cDNA clone 1424117_at H3030A06 3.95752801 2.42838452 1.9 2.2 2.62132809 1.3344E-08 5.66E-07 MGC:67360 IMAGE:6823629, complete cds NA 4 153 guanine nucleotide binding protein, 1454696_at -3.46081884 -4 -1.3 -1.6 -2.6026947 8.58458E-05 0.0012617 beta 1 Gnb1 4 153 guanine nucleotide binding protein, 1417432_a_at H3094D02 -3.13334396 -4 -1.6 -1.7 -2.5946297 1.04542E-05 0.0002202 beta 1 Gadd45gip1 8 84.1 RAD23a homolog (S. -

Oup Radres Rrz001 289..297 ++
Journal of Radiation Research, Vol. 60, No. 3, 2019, pp. 289–297 doi: 10.1093/jrr/rrz001 Advance Access Publication: 26 February 2019 Ionizing radiation affects the composition of the proteome of extracellular vesicles released by head-and-neck cancer cells in vitro Agata Abramowicz1, Anna Wojakowska1, Lukasz Marczak2, Malgorzata Lysek-Gladysinska3, Mateusz Smolarz1, Michael D. Story4, Joanna Polanska5, Piotr Widlak1 and Monika Pietrowska1,* 1Center for Translational Research and Molecular Biology of Cancer, Maria Sklodowska–Curie Institute–Oncology Center, Gliwice Branch, ul. Wybrzeze Armii Krajowej 15, 44-101 Gliwice, Poland 2Institute of Bioorganic Chemistry, Polish Academy of Sciences, ul. Noskowskiego 12/14, 61-704 Poznan, Poland 3The Jan Kochanowski University in Kielce, Institute of Biology, Department of Cell Biology and Electron Microscopy, ul. Swietokrzyska 15, 25-406 Kielce, Poland 4University of Texas Southwestern Medical Center, Department of Radiation Oncology, Division of Molecular Radiation Biology, 5323 Harry Hines Boulevard, Dallas, TX 75390, USA 5Faculty of Automatic Control, Electronics and Computer Science, Silesian University of Technology, ul. Akademicka 16, 44-100 Gliwice, Poland *Corresponding author. Center for Translational Research and Molecular Biology of Cancer, Maria Sklodowska–Curie Institute–Oncology Center, Gliwice Branch, ul. Wybrzeze Armii Krajowej 15, 44-101 Gliwice, Poland. Tel: +0048-32-278-9627; Fax: +0048-32-278-9840; Email: [email protected] (Received 29 August 2018; revised 7 November 2018; editorial decision 8 January 2019) ABSTRACT Exosomes and other extracellular vesicles are key players in cell-to-cell communication, and it has been proposed that they are involved in different aspects of the response to ionizing radiation, including transmitting the radiation-induced bystander effect and mediating radioresistance. -

Gene Therapy Glossary of Terms
GENE THERAPY GLOSSARY OF TERMS A • Phase 3: A phase of research to describe clinical trials • Allele: one of two or more alternative forms of a gene that that gather more information about a drug’s safety and arise by mutation and are found at the same place on a effectiveness by studying different populations and chromosome. different dosages and by using the drug in combination • Adeno-Associated Virus: A single stranded DNA virus that has with other drugs. These studies typically involve more not been found to cause disease in humans. This type of virus participants.7 is the most frequently used in gene therapy.1 • Phase 4: A phase of research to describe clinical trials • Adenovirus: A member of a family of viruses that can cause occurring after FDA has approved a drug for marketing. infections in the respiratory tract, eye, and gastrointestinal They include post market requirement and commitment tract. studies that are required of or agreed to by the study • Adeno-Associated Virus Vector: Adeno viruses used as sponsor. These trials gather additional information about a vehicles for genes, whose core genetic material has been drug’s safety, efficacy, or optimal use.8 removed and replaced by the FVIII- or FIX-gene • Codon: a sequence of three nucleotides in DNA or RNA • Amino Acids: building block of a protein that gives instructions to add a specific amino acid to an • Antibody: a protein produced by immune cells called B-cells elongating protein in response to a foreign molecule; acts by binding to the • CRISPR: a family of DNA sequences that can be cleaved by molecule and often making it inactive or targeting it for specific enzymes, and therefore serve as a guide to cut out destruction and insert genes. -

Investigating Cone Photoreceptor Development Using Patient-Derived NRL Null Retinal Organoids
ARTICLE https://doi.org/10.1038/s42003-020-0808-5 OPEN Investigating cone photoreceptor development using patient-derived NRL null retinal organoids Alyssa Kallman1,11, Elizabeth E. Capowski 2,11, Jie Wang 3, Aniruddha M. Kaushik4, Alex D. Jansen2, Kimberly L. Edwards2, Liben Chen4, Cynthia A. Berlinicke3, M. Joseph Phillips2,5, Eric A. Pierce6, Jiang Qian3, ✉ ✉ Tza-Huei Wang4,7, David M. Gamm2,5,8 & Donald J. Zack 1,3,9,10 1234567890():,; Photoreceptor loss is a leading cause of blindness, but mechanisms underlying photoreceptor degeneration are not well understood. Treatment strategies would benefit from improved understanding of gene-expression patterns directing photoreceptor development, as many genes are implicated in both development and degeneration. Neural retina leucine zipper (NRL) is critical for rod photoreceptor genesis and degeneration, with NRL mutations known to cause enhanced S-cone syndrome and retinitis pigmentosa. While murine Nrl loss has been characterized, studies of human NRL can identify important insights for human retinal development and disease. We utilized iPSC organoid models of retinal development to molecularly define developmental alterations in a human model of NRL loss. Consistent with the function of NRL in rod fate specification, human retinal organoids lacking NRL develop S- opsin dominant photoreceptor populations. We report generation of two distinct S-opsin expressing populations in NRL null retinal organoids and identify MEF2C as a candidate regulator of cone development. 1 Institute of Genetic Medicine, Johns Hopkins University School of Medicine, Baltimore, USA. 2 Waisman Center, University of Wisconsin-Madison, Madison, USA. 3 Department of Ophthalmology, Wilmer Eye Institute, Johns Hopkins University School of Medicine, Baltimore, USA. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

4-6 Weeks Old Female C57BL/6 Mice Obtained from Jackson Labs Were Used for Cell Isolation
Methods Mice: 4-6 weeks old female C57BL/6 mice obtained from Jackson labs were used for cell isolation. Female Foxp3-IRES-GFP reporter mice (1), backcrossed to B6/C57 background for 10 generations, were used for the isolation of naïve CD4 and naïve CD8 cells for the RNAseq experiments. The mice were housed in pathogen-free animal facility in the La Jolla Institute for Allergy and Immunology and were used according to protocols approved by the Institutional Animal Care and use Committee. Preparation of cells: Subsets of thymocytes were isolated by cell sorting as previously described (2), after cell surface staining using CD4 (GK1.5), CD8 (53-6.7), CD3ε (145- 2C11), CD24 (M1/69) (all from Biolegend). DP cells: CD4+CD8 int/hi; CD4 SP cells: CD4CD3 hi, CD24 int/lo; CD8 SP cells: CD8 int/hi CD4 CD3 hi, CD24 int/lo (Fig S2). Peripheral subsets were isolated after pooling spleen and lymph nodes. T cells were enriched by negative isolation using Dynabeads (Dynabeads untouched mouse T cells, 11413D, Invitrogen). After surface staining for CD4 (GK1.5), CD8 (53-6.7), CD62L (MEL-14), CD25 (PC61) and CD44 (IM7), naïve CD4+CD62L hiCD25-CD44lo and naïve CD8+CD62L hiCD25-CD44lo were obtained by sorting (BD FACS Aria). Additionally, for the RNAseq experiments, CD4 and CD8 naïve cells were isolated by sorting T cells from the Foxp3- IRES-GFP mice: CD4+CD62LhiCD25–CD44lo GFP(FOXP3)– and CD8+CD62LhiCD25– CD44lo GFP(FOXP3)– (antibodies were from Biolegend). In some cases, naïve CD4 cells were cultured in vitro under Th1 or Th2 polarizing conditions (3, 4). -

Figure S1. Representative Report Generated by the Ion Torrent System Server for Each of the KCC71 Panel Analysis and Pcafusion Analysis
Figure S1. Representative report generated by the Ion Torrent system server for each of the KCC71 panel analysis and PCaFusion analysis. (A) Details of the run summary report followed by the alignment summary report for the KCC71 panel analysis sequencing. (B) Details of the run summary report for the PCaFusion panel analysis. A Figure S1. Continued. Representative report generated by the Ion Torrent system server for each of the KCC71 panel analysis and PCaFusion analysis. (A) Details of the run summary report followed by the alignment summary report for the KCC71 panel analysis sequencing. (B) Details of the run summary report for the PCaFusion panel analysis. B Figure S2. Comparative analysis of the variant frequency found by the KCC71 panel and calculated from publicly available cBioPortal datasets. For each of the 71 genes in the KCC71 panel, the frequency of variants was calculated as the variant number found in the examined cases. Datasets marked with different colors and sample numbers of prostate cancer are presented in the upper right. *Significantly high in the present study. Figure S3. Seven subnetworks extracted from each of seven public prostate cancer gene networks in TCNG (Table SVI). Blue dots represent genes that include initial seed genes (parent nodes), and parent‑child and child‑grandchild genes in the network. Graphical representation of node‑to‑node associations and subnetwork structures that differed among and were unique to each of the seven subnetworks. TCNG, The Cancer Network Galaxy. Figure S4. REVIGO tree map showing the predicted biological processes of prostate cancer in the Japanese. Each rectangle represents a biological function in terms of a Gene Ontology (GO) term, with the size adjusted to represent the P‑value of the GO term in the underlying GO term database. -

Supporting Information
Supporting Information Figure S1. The functionality of the tagged Arp6 and Swr1 was confirmed by monitoring cell growth and sensitivity to hydeoxyurea (HU). Five-fold serial dilutions of each strain were plated on YPD with or without 50 mM HU and incubated at 30°C or 37°C for 3 days. Figure S2. Localization of Arp6 and Swr1 on chromosome 3. The binding of Arp6-FLAG (top), Swr1-FLAG (middle), and Arp6-FLAG in swr1 cells (bottom) are compared. The position of Tel 3L, Tel 3R, CEN3, and the RP gene are shown under the panels. Figure S3. Localization of Arp6 and Swr1 on chromosome 4. The binding of Arp6-FLAG (top), Swr1-FLAG (middle), and Arp6-FLAG in swr1 cells (bottom) in the whole chromosome region are compared. The position of Tel 4L, Tel 4R, CEN4, SWR1, and RP genes are shown under the panels. Figure S4. Localization of Arp6 and Swr1 on the region including the SWR1 gene of chromosome 4. The binding of Arp6- FLAG (top), Swr1-FLAG (middle), and Arp6-FLAG in swr1 cells (bottom) are compared. The position and orientation of the SWR1 gene is shown. Figure S5. Localization of Arp6 and Swr1 on chromosome 5. The binding of Arp6-FLAG (top), Swr1-FLAG (middle), and Arp6-FLAG in swr1 cells (bottom) are compared. The position of Tel 5L, Tel 5R, CEN5, and the RP genes are shown under the panels. Figure S6. Preferential localization of Arp6 and Swr1 in the 5′ end of genes. Vertical bars represent the binding ratio of proteins in each locus. -

Lecture 3 Types, Biology and Salient Features of Vectors in Recombinant
NPTEL – Bio Technology – Genetic Engineering & Applications MODULE 1- LECTURE 3 TYPES, BIOLOGY AND SALIENT FEATURES OF VECTORS IN RECOMBINANT DNA TECHNOLOGY – PLASMID 1-3.1 Introduction: DNA molecule used for carrying an exogenous DNA into a host organism and facilitates stable integration and replication inside the host system is termed as Vector. Molecular cloning involves series of sequential steps which includes restriction digestion of DNA fragments both target DNA and vector, ligation of the target DNA with the vector and introduction into a host organism for multiplication. Then the fragments resulted after digestion with restriction enzymes are ligated to other DNA molecules that serve as vectors. In general, vectors should have following characteristics: • Capable of replicating inside the host. • Have compatible restriction site for insertion of DNA molecule (insert). • Capable of autonomous replication inside the host (ori site). • Smaller in size and able to incorporate larger insert size. • Have a selectable marker for screening of recombinant organism. 1-3.2 Plasmids: • Plasmids are naturally occurring extra chromosomal double-stranded circular DNA molecules which can autonomously replicate inside bacterial cells. Plasmids range in size from about 1.0 kb to over 250 kb. • Plasmids encode only few proteins required for their own replication (replication proteins) and these proteins encoding genes are located very close to the ori. All the other proteins required for replication, e.g. DNA polymerases, DNA ligase, helicase, etc., are provided by the host cell.Thus, only a small region surrounding Joint initiative of IITs and IISc – Funded by MHRD Page 28 of 84 NPTEL – Bio Technology – Genetic Engineering & Applications the ori site is required for replication. -

Molecular Biology and Applied Genetics
MOLECULAR BIOLOGY AND APPLIED GENETICS FOR Medical Laboratory Technology Students Upgraded Lecture Note Series Mohammed Awole Adem Jimma University MOLECULAR BIOLOGY AND APPLIED GENETICS For Medical Laboratory Technician Students Lecture Note Series Mohammed Awole Adem Upgraded - 2006 In collaboration with The Carter Center (EPHTI) and The Federal Democratic Republic of Ethiopia Ministry of Education and Ministry of Health Jimma University PREFACE The problem faced today in the learning and teaching of Applied Genetics and Molecular Biology for laboratory technologists in universities, colleges andhealth institutions primarily from the unavailability of textbooks that focus on the needs of Ethiopian students. This lecture note has been prepared with the primary aim of alleviating the problems encountered in the teaching of Medical Applied Genetics and Molecular Biology course and in minimizing discrepancies prevailing among the different teaching and training health institutions. It can also be used in teaching any introductory course on medical Applied Genetics and Molecular Biology and as a reference material. This lecture note is specifically designed for medical laboratory technologists, and includes only those areas of molecular cell biology and Applied Genetics relevant to degree-level understanding of modern laboratory technology. Since genetics is prerequisite course to molecular biology, the lecture note starts with Genetics i followed by Molecular Biology. It provides students with molecular background to enable them to understand and critically analyze recent advances in laboratory sciences. Finally, it contains a glossary, which summarizes important terminologies used in the text. Each chapter begins by specific learning objectives and at the end of each chapter review questions are also included.