Business Continuity Plan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Education Sector 2020
Media pack Education Sector 2020 Parenting is a lifelong sequence of tough decisions. None are more important than the decisions that have to be made about a child’s education - from pre-school to post 16 or 18 choices. KM Media Group has a number of products which offer help and advice to parents and also students, whilst celebrating exam success. These products provide an opportunity to promote education, training and childcare services to a targeted audience. s Publications are complemented by extensive online and radio packages kmfm With a network of 7 local kmfm stations and 1 DAB station, KM Media Group’s radio portfolio reaches a weekly audience of 193,000 people across Kent.* The biggest hit songs from today and the last 20 years, kmfm provides a mix of music, news and essential travel information. kmfm can offer a variety of options to advertisers including airtime, sponsorship and promotional opportunities. Depending on what you are advertising and what you are looking to achieve, kmfm can be as flexible as you need. KentOnline KentOnline has over 3.3 million unique visitors every month** and is the destination for Kent news and information. It is also a gateway to local sites via “Where I Live” and specialist sites such as KentJobs and Kent Business. With options to suit any budget, from basic banners to sponsorship opportunities, KentOnline is flexible and creative. It is a cost effective way to target messages to both parents and students alike. * RAJAR Q4 2019 (Jul 2019 -Dec 2019) ** Google Analytics (Jan-Feb 2020 Education Training & Childcare Supplement Education, Training & Childcare is a special supplement published by KM Media Group four times a year. -

Canterbury Christmas Guide 2019
ai15710668737_Canterbury Christmas cover.pdf 1 14/10/2019 16:27 2019 CANTERBURY shop dine stay skate C M Y CM MY CY CMY K Wrap up warm and discover the delights of Canterbury this Christmas Brought to you by Canterbury.co.uk #CanterburyisChristmas With: Contents Canterbury at Christmas 2019 Your Guide to What’s On, Places to Visit, Shopping, Dining and Going Out! Lighting Up Christmas 05 Festive Ice Rink Comes to Canterbury 10 Cosy Pubs with Real Fires 14/15 Small Business Saturday in Canterbury 22 City Map 26-27 What’s On in Canterbury this Christmas 28-32 Evolution Productions - exclusive pantomime interview 34-35 Canterbury’s Christmas Market and Santa’s Grotto 38-39 Mother Goose Golden Egg Competition 39 Travel and getting around 44 Christmas by the Sea 46-47 Let us help you find the best places to shop, eat, drink, visit, skate and have fun this Christmas! With festive fairs, music, crafts, dining, theatre, great shopping and so much more – the very best destination in Kent at Christmas is Canterbury! #CanterburyisChristmas @my_canterbury Guide published by Canterbury Connected BID @mycanterbury MyCanterbury Visitor Information Centre, 18 High Street, Canterbury, CT1 2RA / 01227 862 162 *Sometimes things change! We try to check all events times/dates but please check websites for most up to date information and updates. Designed and produced by www.arc-cs.com 03 CANTERBURY New Year’s Eve Tasting Dinner Celebrate the arrival of 2020 with our outstanding black-tie tasting dinner. Start the evening with a glass of Champagne in our celebrated 3 AA rosette restaurant then savour seven superb courses to the sounds of our resident pianist. -

The Experts in Specialist Lending
specialist lending specialist Annual Report and Accounts 2017 Accounts and Report Annual in experts The OneSavings Bank plc ANNUAL REPORT AND ACCOUNTS 2017 OneSavings Bank plc Annual Report and Accounts 2017 Highlights Gross new lending Net loan book Who we are +14% +23% OneSavings Bank is 2017: £2.6bn 2017: £7.3bn 2016: £2.3bn 2016: £5.9bn a specialist lender, primarily focused on 2016 2017 2016 2017 carefully selected sub-sectors of the Net interest margin Cost to income ratio mortgage market. Our specialist Stable Stable lending is supported 2017: 316bps 2017: 27% 2016: restated 316bps2 2016: 27%2 by a stable retail 2016 2017 2016 2017 savings franchise with over 150 years of heritage. Profit before tax Underlying profit before tax Full year dividend per share +3% +21% +22% 2017: £167.7m 2017: £167.7m 2017: 12.8p 2016: £163.1m1 2016: restated £138.2m2 2016: 10.5p 2016 2017 2016 2017 Fully-loaded common equity Tier 1 ratio Strengthened 2017: 13.7% 2016: 13.3% Basic EPS Underlying basic EPS +3% +23% Customer satisfaction (NPS) 2017: 51.1p 2017: 51.1p 2016: 49.4p 2016: 41.7p +3 2017: +62 2016 2017 2016 2017 2016: +59 Our investor site gives you direct access to a wide range of information about OSB: www.osb.co.uk For more information and definitions, see Key performance indicators on page 26 1. In 2016, profit before tax included net gain from exceptional items of £24.9m. 2. Prior to 2017, OSB deducted coupons on equity Perpetual Subordinated Bonds (‘PSBs’) accounted for as dividends from underlying profit before and after tax, net interest margin and cost to income ratio. -

RADIO MADE in KENT Gravesend Sheerness
RADIO MADE IN KENT Gravesend Sheerness Margate Rochester Chatham Herne Bay Ramsgate Sittingbourne FavershamWhitstable Sandwich Canterbury Maidstone Sevenoaks Deal Tonbridge Dover Tunbridge Wells Ashford Folkestone Tenterden New Romney * RAJAR Q1 2016 (Oct 2015 - Mar 2016) Countywide reaches 176,700 listeners each week* 5ReasonstoUseRadio 1 Radio talks to people 3 Radio is a ‘local friend’ 5 Radio builds at the right time and for listeners. long-term brand place. Listeners typically describe their favourite dominance. local radio station as a friend, and that Radio works in “real time” so ads can be run Because radio messages are repeated at just the time when people are most ready friendship can be used by advertisers to more often and have lower levels of to be influenced by the message. change the way local people perceive them avoidance, by the time a listener is ready to – to keep ahead of the competition. make a purchase, the retailer’s brand name 2 Radio reaches the and values are strongly established in their right local audiences. 4 Radio is the most mind. This is particularly true for brands Naturally the listeners to a local radio station flexible medium. which invest in sonic identities or jingles. are locals. But more importantly they are Business conditions can change fast and also the right kind of locals. Compared to radio is well set to meet those changes. other media, commercial radio listeners Production of commercials is quick and tend to be significantly younger. relatively low-cost. 5ReasonstoUsekmfm 1 kmfm – Radio Made in Kent. 4 kmfm entertains and informs. kmfm is the local radio station for Kent broadcasting from our Kent Providing the best news, travel, weather and what’s going on every studios 24 hours a day, 7 days a week. -

Shoreline (Retrocadia Ltd): Amended Application for a Community Radio Licence
Shoreline (Retrocadia Ltd): Amended application for a community radio licence An application from Retrocadia Ltd (“Retrocadia”) for a community radio licence was submitted in October 2015. Ofcom was unable to consider this application within the timeframe set out in our invitation document, and in July 2016 made a decision not to award a licence to Retrocadia. After considering submissions made by Retrocadia relating to the delay in considering this application and to changes to the applicant’s circumstances, Ofcom offered Retrocadia the opportunity to submit an amended version of its application for a community radio licence for fresh consideration. Retrocadia took up this offer and submitted an amended application (attached) on 21 October 2016. The application by Retrocadia is for an area in Romney Marsh in Kent, where there were no competing applications, for which a frequency has been identified, and where there is no existing locally-focussed radio service. The amended application is currently under consideration and Ofcom will make a decision in the new year. December 2016 Community radio licence application form Version 4 Shoreline (Retrocadia Ltd) - Hythe Bay and Romney Marsh, Kent Community radio application form 1. Station Name Guidance Notes What is the proposed station name? This is the name you expect to use to identify the station on air. Answer: Shoreline 2. Community to be served Guidance Notes Define the community or communities you are It is a legislative requirement that a service is proposing to serve. Drawing from various sources of intended primarily to serve one or more data (e.g. from the Office of Population, Census and communities (whether or not it also serves Survey) and in relation to your proposed coverage other members of the public) and we need to area, please determine the size of the population understand who comprises that community or concerned and the make-up of the population as a communities. -

Appendix 2 One You Kent Campaign 1. Introduction 1.1 During The
Appendix 2 One You Kent Campaign 1. Introduction 1.1 During the consultation period for the re-design of healthy lifestyle services in Kent the public commented that they were not aware of the services that were available, and were unsure of where to go if they wanted further support. 1.2 Whilst the re-design work was underway, Public Health England (PHE) launched the One You brand to promote healthier lifestyles with the intention to create a brand awareness as strong as that of Change 4 Life (over 90% brand recognition). The One You brand is supported by a series of PHE apps to support people , including apps to support giving up smoking, to encourage activity, and healthy meal planners. 1.3 The KCC Cabinet Member for Social Care and Public Health took a key decision for lifestyle services to be integrated and for the resulting service to be called One You Kent in order to take advantage of the national investment in the One You brand, and associated behavioural research. 2 The One You Campaign in Kent 2.1 As a part of a planned programme of campaign work, KCC commissioned two agencies to work on ensuring that the One You message is promoted across Kent. in line with the findings from the behavioural insights report. These two agencies have specific remits: Zest have been engaged to deliver a programme of consumer led work 2.2 iFour have been engaged to work with partners, providers, stakeholders and channels across Kent to understand how the One You message can be effectively spread, and what materials could be developed to support each of these groups to promote healthier lifestyles in a consistent way (using standardised wording and messaging). -

Distribution Rules
PERFORMING RIGHT SOCIETY LIMITED DISTRIBUTION RULES Appendices APPENDIX Standard distribution cycle Distribution Source April July October December Reconciliation BBC radio Oct – Dec Jan - Mar Apr - Jun Jul - Sept July BBC TV Sept - Dec Jan - Mar Apr - Jun Jul - Aug July BSkyB TV Sept - Dec Jan - Mar Apr - Jun Jul - Aug October All other TV Re Sept - Dec Jan - Mar Apr - Jun Jul - Aug April po (exc. music TV channels) rti All other radio ng Oct – Dec Jan - Mar Apr - Jun Jul - Sept April (and music TV channels) Pe ri od Public performance * Oct – Dec Jan - Mar Apr - Jun Jul - Sept April Online ** Oct – Dec Jan - Mar Apr - Jun Jul - Sept N/A International Jul-Dec Jan-Jun N/A (agencies) International Varies depending on affiliate society timetable N/A (affiliate societies) *Concerts using the live concert service are distributed outside the four major distributions with a target of within 60 days of the concert **It is not always possible to adhere to this timetable for some online services Broadcast sampling rates Since 2010 new TV and radio services are sampled at the following minimum rates. TV Sampling Threshold Sample Band Days 4 0-15K 10 15-30K 37 30-60K 91 60-100K 181 100-200K 365 200K+ Radio Sampling Threshold Sample Band Days 4 £0-£50K 8 £50-£100K 16 £100-£200K 32 £200-£500K 365 £750K+ At present services that existed before 2010 are still sampled at minimum rates calculated using a complex statistical formula. In practice, because of electronic reporting and the use of music recognition technology, many services have much higher sample rates, bordering on census for non-advertising plays. -
Appendix 3 By: Jessica Mookherjee, Consultant in Public Health & Wayne Gough: Public Health Commissioning Team 10Th June
Appendix 3 By: Jessica Mookherjee, Consultant in Public Health & Wayne Gough: Public Health Commissioning Team 10th June 2015 Subject: Public Health Campaigns & Press Classification: Unrestricted Summary Marketing and communications is a key element in delivering successful public health interventions. KCC Public Health recognised the need to increase delivery in this area, and have taken steps to increase the resource dedicated to campaigns in the coming year. Recent campaigns have shown promising results in creating behaviour change, and the planned approach to campaign delivery will lead to a strong programme in 2015/16, aimed at bringing about behaviour change in the key areas of priority for public health. 1. Introduction 1.1. Marketing and Communications is a key element of supporting the public to maintain or improve their health. 1.2. During 2014/15 the KCC Public Health department have recognised that delivery in this area could be improved, and have been increasing the resource dedicated to delivery. 1.3. This paper will cover some of the recent campaigns, the coverage received and the early evidence of impact, before looking at the planning for campaigns in the future. 2. Campaigns and Press in 2014/15 2.1. When developing campaigns we look to identify the problem, or the behaviour change that is needed, then look at the audiences we need to reach, and what avenues we can use to get the message across. 2.2. Where possible, national campaigns are supported, and their reach extended where needed, rather than trying to create something new. The Public Health team work partners, and our suppliers, wherever possible to ensure a co-ordinated approach to communicating messages to the public. -
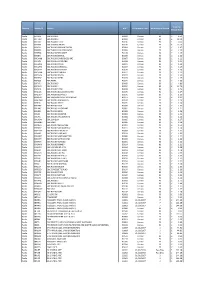
Domain Station ID Station UDC Performance Date No of Days in Period Total Per Minute Rate Radio BR ONE BBC RADIO 1 B0001 Census
Total Per Domain Station ID Station UDC Performance Date No of Days in Period Minute Rate Radio BR ONE BBC RADIO 1 B0001 Census 90 £ 4.51 Radio BR TWO BBC RADIO 2 B0002 Census 90 £ 18.00 Radio BR1EXT BBC RADIO 1XTRA B0106 Census 90 £ 0.60 Radio BR4DIG BBC SCHOOL RADIO B0109 Census 90 £ 13.70 Radio BRASIA BBC RADIO ASIAN NETWORK B0064 Census 90 £ 1.47 Radio BRBEDS BBC THREE COUNTIES RADIO B0065 Census 90 £ 1.25 Radio BRBERK BBC RADIO BERKSHIRE B0103 Census 90 £ 1.19 Radio BRBRIS BBC RADIO BRISTOL B0066 Census 90 £ 1.16 Radio BRCAMB BBC RADIO CAMBRIDGESHIRE B0067 Census 90 £ 1.22 Radio BRCLEV BBC RADIO CLEVELAND B0068 Census 90 £ 1.22 Radio BRCMRU BBC RADIO CYMRU B0011 Census 90 £ 1.24 Radio BRCORN BBC RADIO CORNWALL B0069 Census 90 £ 1.29 Radio BRCOVN BBC RADIO COVENTRY B0070 Census 90 £ 1.18 Radio BRCUMB BBC RADIO CUMBRIA B0071 Census 90 £ 1.23 Radio BRDEVN BBC RADIO DEVON B0072 Census 90 £ 1.30 Radio BRDRBY BBC RADIO DERBY B0073 Census 90 £ 1.25 Radio BRESSX BBC ESSEX B0074 Census 90 £ 1.36 Radio BRFIVE BBC RADIO 5 B0005 Census 90 £ 4.89 Radio BRFOUR BBC RADIO 4 B0004 Census 90 £ 13.70 Radio BRFOYL BBC RADIO FOYLE B0019 Census 90 £ 1.76 Radio BRGLOS BBC RADIO GLOUCESTERSHIRE B0075 Census 90 £ 1.17 Radio BRGUER BBC RADIO GUERNSEY B0076 Census 90 £ 1.13 Radio BRHRWC BBC HEREFORD AND WORCESTER B0077 Census 90 £ 1.21 Radio BRHUMB BBC RADIO HUMBERSIDE B0078 Census 90 £ 1.29 Radio BRJERS BBC RADIO JERSEY B0079 Census 90 £ 1.14 Radio BRKENT BBC RADIO KENT B0080 Census 90 £ 1.32 Radio BRLANC BBC RADIO LANCASHIRE B0081 Census 90 £ 1.21 Radio -
Radio Made in Kent
Radio Made in Kent • Kent’s local commercial radio station • Kent’s Biggest Hits • The biggest hit songs from today and the last 20 years • Top ten played artists: • Daft Punk • Bruno Mars • Justin Timberlake • Olly Murs • Pink • Saturdays • Calvin Harris Ft. Ellie Goulding • Maroon 5 • Swedish House Mafia • Ed Sheeran • Over 1,000 songs on our playlist, genuinely playing more variety • Target audience 25-44 year olds (Broad 15-54 year olds) Radio for Kent...from Kent Broadcast Areas 7 stations across Kent Ashford 107.6fm Canterbury, Whitstable & Herne Bay 106fm Medway 100.4-107.9fm Maidstone 105.6fm Shepway & White Cliffs Country 96.4-106.8fm Thanet 107.2fm West Kent 96.2-101.6fm PLUS DAB and online Estimated population 1,038,000* (Adults 15+ years) reaches 156,000 listeners a week* *RAJAR Q3 2013 Main Programmes • 0530-0900: kmfm Breakfast with Rob & Emma • Traffic & Travel / Local News / Weather • Regular big promotions • Ongoing features (£500 to be won everyday in 10 in 30) Rob & Garry Emma • 0900-1300: kmfm Mornings with Garry Wilson Emma • 1300-1600: kmfm Afternoons with Emma Adam • 1600-1900: Drivetime with Andy Walker • 1900-2200: kmfm Extra with Oli Kemp • Friday & Saturday Evenings: Ultimate Floor Fillers • Sunday afternoon: Tony Blackburn Andy Oli Tony Live and Local Seen at BIG (and small) events around the County… • Leeds Castle • Tunbridge Wells Food Festival • Assembly Hall Tunbridge Wells Opening Nights • Kent County Show • Bluewater • Breast Cancer Care Pink Ribbon Walk • Paws in the Park, Detling • Diamond Ice, Fremlin -

Iliffe Media Ltd Acquires KM Media Group
Iliffe Media Ltd acquires KM Media Group Iliffe Media Ltd has acquired the entire shareholding of Kent’s independent publisher KM Media Group Ltd. KM Media Group publishes nine paid-for and four free newspapers including the Kent Messenger Series, the current Regional Press Awards Newspaper of the Year, and the Kentish Gazette, established in 1717. The group publishes KentOnline.co.uk, with an audience of 2.4m unique monthly browsers. In addition to print and online, the group operates the kmfm radio network, reaching 164,000 listeners each week, and will soon be broadcasting on television through a joint initiative with the University of Kent. Its newspapers are among the UK’s biggest-selling weekly titles with a long established heritage dating back 300 years. The deal represents the latest stage in the expansion of Iliffe Media, following the launch of the Cambridge Independent in 2016 and the acquisition of 13 titles from Johnston Press earlier this year. KM Media Group chairman Geraldine Allinson said the deal with Iliffe would allow KM to continue to evolve and bring about much needed investment to maintain its independence and continue to serve the people of Kent with trusted news and other valued content. It also enables KM to resolve the long standing issues surrounding its closed final salary pension scheme. Geraldine, who will remain fully involved with KM Media Group, said: “The directors and I believe this deal represents the best possible outcome for our staff and customers. “Although there is some personal sadness for me and my family that our pension liabilities have led us to this position, in Iliffe we have found a publisher which shares our belief in the importance of local media. -

Countywideaug.Pdf
Gravesend Sheerness Margate Rochester Chatham Herne Bay Ramsgate Sittingbourne FavershamWhitstable Sandwich Canterbury Maidstone Sevenoaks Deal Tonbridge Dover Tunbridge Wells Ashford Folkestone Tenterden New Romney Countywide reaches 160,100 listeners each week* * RAJAR Q2 2017 (Jan - June 2017) 5ReasonstoUseRadio 1 Radio talks to people 3 Radio is a ‘local 5 Radio builds at the right time and friend’ for listeners. long-term brand place. Listeners typically describe their favourite dominance. local radio station as a friend, and that Radio works in “real time” so ads can be Because radio messages are repeated run at just the time when people are most friendship can be used by advertisers to more often and have lower levels of ready to be influenced by the message. change the way local people perceive avoidance, by the time a listener is ready to them – to keep ahead of the competition. make a purchase, the retailer’s brand name 2 Radio reaches the and values are strongly established in their right local audiences. 4 Radio is the most mind. This is particularly true for brands Naturally the listeners to a local radio flexible medium. which invest in sonic identities or jingles. station are locals. But more importantly Business conditions can change fast and they are also the right kind of locals. radio is well set to meet those changes. Compared to other media, commercial Production of commercials is quick and radio listeners tend to be significantly relatively low-cost. younger. 5ReasonstoUseRadio 1 kmfm – Radio Made in Kent. 4 kmfm entertains and informs. kmfm is the local radio station for Kent broadcasting from our Kent Providing the best news, travel, weather and what’s going on every studios 24 hours a day, 7 days a week.