Generalized Hyperpigmentation After Pyrimethamine Use
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Reticulate Hyperpigmentation of the Skin After Topical Application Of
Letters to the Editor 301 Reticulate Hyperpigmentation of the Skin After Topical Application of Benzoyl Peroxide Sir, Our two patients appeared to develop an irritant response on Benzoyl peroxide (BP) is an e¡ective and frequently used topical thetrunk afterapplication of 5% benzoyl peroxide. One medication for the treatment of acne vulgaris. It is a strong, patient applied BP to his face withnoirritation,consistentwith broad spectrum bactericidal agent that signi¢cantly decreases the ¢ndings of Hausteinetal.(3). Both patients then developed the number of Propionibacterium acnes in both the follicle and apattern of reticulate hyperpigmentation after their initial der- on surface skin (1). A common side e¡ect after usage is irritation matitis subsided. Biopsy in both cases was consistent with of the skin, usually manifested as a stinging or burning, and postin£ammatory hyperpigmentation. sometimes accompanied by erythema and scaling. Benzoyl per- Postin£ammatory hyperpigmentation develops after acute oxide is a strong irritant, but a weak allergen, rarely causing a or chronic in£ammation and trauma to the skin. The intensity contact dermatitis (2, 3). Tolerance can be achieved by gradually of the hypermelanosistendstobe more pronounced in darker- increasing the frequency of application over time. We describe skinnedindividuals. Other conditions that produce a pattern of two cases in which topical application of benzoyl peroxide reticulate hyperpigmentation include Riehl's melanosis, resulted in an unusual pattern of reticulate hyperpigmentation which is characterized by reticulate brown-black pigmenta- of the skin, most likely as a sequela of an irritant contact derma- tion of the face and neck. This is thought to be a result of a titis. -
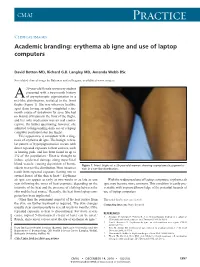
Erythema Ab Igne and Use of Laptop Computers
CMAJ Practice Clinical images Academic branding: erythema ab igne and use of laptop computers David Botten MD, Richard G.B. Langley MD, Amanda Webb BSc See related clinical image by Beleznay and colleagues, available at www.cmaj.ca 20-year-old female university student presented with a two-month history A of asymptomatic pigmentation in a net-like distribution, isolated to the front thighs (Figure 1). She was otherwise healthy, apart from having recently completed a six- month course of isotretinoin for acne. She had no history of trauma to the front of the thighs, and her only medication was an oral contra- ceptive. On further questioning, however, she admitted to longstanding daily use of a laptop computer positioned atop her thighs. This appearance is consistent with a diag- nosis of erythema ab igne. The benign, reticu- lar pattern of hyperpigmentation occurs with direct repeated exposure to heat sources, such as heating pads, and has been found in up to 3% of the population.1 Heat is thought to induce epidermal damage along superficial blood vessels, causing deposition of hemo- Figure 1: Front thighs of a 20-year-old woman showing asymptomatic pigmenta- siderin in a net-like distribution. Most instances tion in a net-like distribution. result from repeated exposure (lasting one to several hours) of the skin to heat.2,3 Erythema ab igne can appear as early as two weeks or as late as one With the widespread use of laptop computers, erythema ab year following the onset of heat exposure, depending on the igne may become more common. -

Review Cutaneous Patterns Are Often the Only Clue to a a R T I C L E Complex Underlying Vascular Pathology
pp11 - 46 ABstract Review Cutaneous patterns are often the only clue to a A R T I C L E complex underlying vascular pathology. Reticulate pattern is probably one of the most important DERMATOLOGICAL dermatological signs of venous or arterial pathology involving the cutaneous microvasculature and its MANIFESTATIONS OF VENOUS presence may be the only sign of an important underlying pathology. Vascular malformations such DISEASE. PART II: Reticulate as cutis marmorata congenita telangiectasia, benign forms of livedo reticularis, and sinister conditions eruptions such as Sneddon’s syndrome can all present with a reticulate eruption. The literature dealing with this KUROSH PARSI MBBS, MSc (Med), FACP, FACD subject is confusing and full of inaccuracies. Terms Departments of Dermatology, St. Vincent’s Hospital & such as livedo reticularis, livedo racemosa, cutis Sydney Children’s Hospital, Sydney, Australia marmorata and retiform purpura have all been used to describe the same or entirely different conditions. To our knowledge, there are no published systematic reviews of reticulate eruptions in the medical Introduction literature. he reticulate pattern is probably one of the most This article is the second in a series of papers important dermatological signs that signifies the describing the dermatological manifestations of involvement of the underlying vascular networks venous disease. Given the wide scope of phlebology T and its overlap with many other specialties, this review and the cutaneous vasculature. It is seen in benign forms was divided into multiple instalments. We dedicated of livedo reticularis and in more sinister conditions such this instalment to demystifying the reticulate as Sneddon’s syndrome. There is considerable confusion pattern. -

Phytophotodermatitis
PHYTOPHOTODERMATITIS http://www.aocd.org Phytophotodermatitis (PPD) is a cutaneous phototoxic reaction that occurs following contact with certain plants. The reaction is stimulated by skin exposure to light sensitizing botanical substances known as furanocoumarins followed by exposure to long wave ultraviolet light in sunlight. Furanocoumarins are present in plants such as, lemons, limes, mangos, parsley and many weeds. Psoralen is the active particle in furanocoumarins. Upon UVA radiation exposure from sunlight, psoralens within the skin react with molecular oxygen and form reactive oxygen species that induce destruction of skin cells and cause an inflammatory reaction. PPD is most common in the spring and summer, as psoralen concentrations are the highest and outdoor activities under the sun are increased. Exposure to plants or solutions such as lemon or lime juice, lead to bizarre patterns of distribution. Streaks may be present from brushing against a plant or haphazard lines from juice. Common presentations are on the upper lip from drinking citrus beverages, from spilled beverages, or even from wiping juice onto exposed skin to dry the hands. This is often referred to as “Margarita Rash”. The rash begins within 24 hours and can peak at 72 hours. The distribution of skin reactions is sharply limited to areas exposed to sun. Skin findings can consist of non-pruritic reactions, mild redness with or without erosions, to severe blistering. Redness can persist for weeks to months. Hyperpigmentation appears 1-2 weeks later and can last up to months. The distribution to sun exposed areas and pattern aid in diagnosis. History and a high index of suspicion is key to diagnosing PPD. -

CSI Dermatology
Meagen M. McCusker, MD [email protected] Integrated Dermatology, Enfield, CT AbbVie - Speaker Case-based scenarios, using look-alike photos, comparing the dermatologic manifestations of systemic disease to dermatologic disease. Select the clinical photo that best matches the clinical vignette. Review the skin findings that help differentiate the two cases. Review etiology/pathogenesis when understood and discuss treatments. Case 1: Scaly Serpiginous Eruption This patient was evaluated for a progressively worsening pruritic rash associated with dyspnea on exertion and 5-kg weight loss. Despite its dramatic appearance, the patient reported no itch. KOH examination is negative (But, who’s good at those anyway?) A. B. Case 1: Scaly Serpiginous Eruption This patient was evaluated for a progressively worsening pruritic rash associated with dyspnea on exertion and 5-kg weight loss. Despite its dramatic appearance, the patient reported no itch. KOH examination is negative (But, who’s good at those anyway?) A. Correct. B. Tinea Corporis Erythema Gyratum Repens Erythema Gyratum Repens Tinea corporis Rare paraneoplastic T. rubrum > T. mentagrophytes phenomenon typically > M. canis associated with lung Risk factors cancer>esophageal and breast Close contact, previous cancers. infection, Less commonly associated with occupational/recreational connective tissue disorders such exposure, contaminated as Lupus or Rheumatoid furniture or clothing, Arthritis gymnasium, locker rooms “Figurate erythema” migrates up 1-3 week incubation → to 1 cm a day centrifugal spread from point of Resolves with treatment of the invasion with central clearing malignancy This patient was diagnosed with squamous cell carcinoma of the lung. Case 2: Purpuric Eruption on the Legs & Buttocks A 12-year old boy presents with a recent history of upper respiratory tract infection, fever and malaise. -

Canine Recurrent Flank Alopecia: a Synthesis of Theory and Practice
Vlaams Diergeneeskundig Tijdschrift, 2014, 83 Review 275 Canine recurrent flank alopecia: a synthesis of theory and practice Caniene recurrente flankalopecia: synthese van theorie en praktijk 1S. Vandenabeele, 1J. Declercq, 2H. De Cock, 1S. Daminet 1Department of Medicine and Clinical Biology of Small Animals, Ghent University, Belgium 2Veterinary Pathology Services/Medvet, Antwerpen, Belgium [email protected] A BSTRACT Canine recurrent flank alopecia is a non-inflammatory, non-scarring alopecia of unknown etiology and has a visually striking clinical presentation. Although this disease entity is relatively common in the northern hemisphere, there is only scant information in the literature regarding case descriptions. The aim of this article was to review the literature and to describe clinical presentations recognized in practice, which are not always extensively documented in the literature. SAMENVATTING Caniene recurrente flankalopecia wordt klassiek gekenmerkt door een niet-inflammatoire alopecia met onbekende etiologie. Deze dermatose wordt getypeerd door unieke huidsymptomen. Alhoewel de aandoening relatief frequent voorkomt in het noordelijk halfrond en dus ook in België, is er slechts beperkte informatie over te vinden in de literatuur. Het doel van dit overzichtsartikel is om enerzijds een samenvatting te geven van de literatuur en anderzijds de verschillende klinische presentaties die herkend worden in de dagelijkse praktijk maar niet vaak beschreven worden in de literatuur, te documenteren. INTRODUCTION and the different clinical presentations that are recog- nized in practice, but which are not extensively men- Canine recurrent flank alopecia (CRFA) is a visu- tioned in the literature. ally striking disease characterized by cyclic episodes of non-inflammatory hair loss (or coat changes) that can recur annually (Miller et al., 2013a). -

UCSF Fresno, Medical Educakon Program J Heppner MD, H Lee MD
(—THIS SIDEBAR DOES NOT PRINT—) QUICK START (cont.) DESIGN GUIDE Phytophotoderma/s Resul/ng From Citrus Exposure: A Pediatric Case Series from Central California How to change the template color theme This PowerPoint 2007 template produces a 36”x48” You can easily change the color theme of your poster by going to the presentation poster. You can use it to create your research DESIGN menu, click on COLORS, and choose the color theme of your poster and save valuable time placing titles, subtitles, text, J Heppner MD, H Lee MD, P Armenian MD choice. You can also create your own color theme. and graphics. UCSF Fresno, Medical Educaon Program We provide a series of online tutorials that will guide you through the poster design process and answer your poster production questions. To view our template tutorials, go online to PosterPresentations.com and click on HELP DESK. You can also manually change the color of your background by going to Introduc>on Case Series Descripon Case Series Descripon Discussion VIEW > SLIDE MASTER. After you finish working on the master be sure to When you are ready to print your poster, go online to Lisbon Lemon (Citrus limon) Key Lime (Citrus aurantifolia) go to VIEW > NORMAL to continue working on your poster. PosterPresentations.com Psoralens belong to the furocoumarin family, and cause This is a consecutive-patient case series of five girls Few phytophotodermatitis outbreaks demonstrate phytophotodermatitis when coupled with ultraviolet aged 7-11 transferred from an outside facility for such severity in multiple pediatric patients, How to add Text Need assistance? Call us at 1.510.649.3001 light exposure. -

Importance of a Thorough Physical Examination! Muhammad Imran, M.D., Julian Magadan III, M.D., Mehrdad Maz, M.D
Kansas Journal of Medicine 2015 Physical Examination Importance of a Thorough Physical Examination! Muhammad Imran, M.D., Julian Magadan III, M.D., Mehrdad Maz, M.D. University of Kansas Medical Center Department of Internal Medicine Division of Allergy, Clinical Immunology, & Rheumatology Kansas City, KS A 73-year-old white female presented for management of her tophaceous gout, pyoderma gangrenosum, and chronic back pain. On exam, there was an incidental finding of reticular, reddish-brown, non-tender, macular, non-blanching discoloration on her entire back, with a few superficial erosions (see Figure). The patient did not know the duration of her rash. It was neither pruritic nor painful. She denied arthralgia, fever, chills, or other constitutional symptoms. She did not have a history of insect bites, recent foreign travel, falls, or trauma. She frequently used a heating pad to alleviate her chronic back pain. Complete blood count, comprehensive metabolic panel, urine analysis, and inflammatory markers were within normal limits. What is most likely diagnosis? A. Vasculitis B. Livedo Reticularis C. Erythema Ab Igne D. Cutaneous Lupus E. Actinic Keratosis 48 Kansas Journal of Medicine 2015 Physical Examination Correct Answer: C. Erythema Ab Igne Erythema ab igne (EAI), also known as ephelis ignealis or toasted skin syndrome, is an unintentional, unperceived, and self-induced condition, which occurs in individuals who persistently use topical or conventional heat to relieve localized pain or cold.1 It is characterized by chronic, localized, erythematous or hyper-pigmented, reticulated, and net-like skin patches in the affected area. It is usually asymptomatic, but burning and pruritus are reported by some patients. -

Dermatological Indications of Disease - Part II This Patient on Dialysis Is Showing: A
“Cutaneous Manifestations of Disease” ACOI - Las Vegas FR Darrow, DO, MACOI Burrell College of Osteopathic Medicine This 56 year old man has a history of headaches, jaw claudication and recent onset of blindness in his left eye. Sed rate is 110. He has: A. Ergot poisoning. B. Cholesterol emboli. C. Temporal arteritis. D. Scleroderma. E. Mucormycosis. Varicella associated. GCA complex = Cranial arteritis; Aortic arch syndrome; Fever/wasting syndrome (FUO); Polymyalgia rheumatica. This patient missed his vaccine due at age: A. 45 B. 50 C. 55 D. 60 E. 65 He must see a (an): A. neurologist. B. opthalmologist. C. cardiologist. D. gastroenterologist. E. surgeon. Medscape This 60 y/o male patient would most likely have which of the following as a pathogen? A. Pseudomonas B. Group B streptococcus* C. Listeria D. Pneumococcus E. Staphylococcus epidermidis This skin condition, erysipelas, may rarely lead to septicemia, thrombophlebitis, septic arthritis, osteomyelitis, and endocarditis. Involves the lymphatics with scarring and chronic lymphedema. *more likely pyogenes/beta hemolytic Streptococcus This patient is susceptible to: A. psoriasis. B. rheumatic fever. C. vasculitis. D. Celiac disease E. membranoproliferative glomerulonephritis. Also susceptible to PSGN and scarlet fever and reactive arthritis. Culture if MRSA suspected. This patient has antithyroid antibodies. This is: • A. alopecia areata. • B. psoriasis. • C. tinea. • D. lichen planus. • E. syphilis. Search for Hashimoto’s or Addison’s or other B8, Q2, Q3, DRB1, DR3, DR4, DR8 diseases. This patient who works in the electronics industry presents with paresthesias, abdominal pain, fingernail changes, and the below findings. He may well have poisoning from : A. lead. B. -

Erythema Ab Igne: a Rare Presentation of Toasted Skin Syndrome with the Use of a Space Heater
Open Access Case Report DOI: 10.7759/cureus.13401 Erythema Ab Igne: A Rare Presentation of Toasted Skin Syndrome With the Use of a Space Heater Zarah Haleem 1 , Judith Philip 1 , Safwan Muhammad 2 1. College of Medicine, American University of Antigua, Coolidge, ATG 2. Internal Medicine, University of Maryland Medical Center Midtown Campus, Baltimore, USA Corresponding author: Zarah Haleem, [email protected] Abstract Erythema ab igne, also known as toasted skin syndrome, is an acquired asymmetric hyperpigmented dermatosis that is caused by repeated exposure to moderate heat or infrared radiation. Hyperpigmentation is caused by the degeneration of elastic fibers and basal cells resulting in the release of melanin. Historically found in bakers and industrial workers, this condition has recently resurfaced in medical literature with the use of novel heat sources such as laptops and heated car seats. While this condition can resolve spontaneously after removal of heat exposure, delay in diagnosis and persistent exposure can lead to permanent pigmentation or progression to Merkel cell carcinoma, basal cell carcinoma, and squamous cell carcinoma. Categories: Dermatology, Internal Medicine, Oncology Keywords: erythema ab igne, space heater, toasted skin syndrome, merkel cell carcinoma, cutaneous hyperpigmentation, atypical rash, squamous cell carcinoma Introduction Toasted skin syndrome is a rare hyperpigmented dermatosis that can occur at any site with recurrent exposure to heat or an infrared source. This condition is known to be more prevalent in women than men and patients with chronic pain [1-3]. The pathophysiology does not seem to be fully understood and multiple mechanisms have been proposed, including the repeated heat exposure damaging superficial blood vessels leading to hemosiderin deposition and subsequent hyperpigmentation. -

Five Cases of Phytophotodermatitis Caused by Fig Leaves and Relevant Literature Review
JH Son, et al pISSN 1013-9087ㆍeISSN 2005-3894 Ann Dermatol Vol. 29, No. 1, 2017 https://doi.org/10.5021/ad.2017.29.1.86 CASE REPORT Five Cases of Phytophotodermatitis Caused by Fig Leaves and Relevant Literature Review Jin-Hwa Son1, Hyunju Jin1, Hyang-Suk You1, Woo-Haing Shim1, Jeong-Min Kim1, Gun-Wook Kim1, Hoon-Soo Kim1, Hyun-Chang Ko1, Moon-Bum Kim1,2, Byung-Soo Kim1,2 1Department of Dermatology, School of Medicine, Pusan National University, 2Biomedical Research Institute, Pusan National University Hospital, Busan, Korea Phytophotodermatitis is a condition caused by sequential ex- INTRODUCTION posure to photosensitizing substances present in plants fol- lowed by ultraviolet light. Several plants (e.g., limes, celery, Phytophotodermatitis is a condition caused by sequential fig, and wild parsnip) contain furocoumarin compounds exposure to certain photosensitizing substance present in (psoralens). It is important for dermatologists to be aware of plants followed by sunlight. Many common plants, includ- phytophotodermatitis because it may be misdiagnosed as ing citrus fruits, celery, and wild parsnip contain such cellulitis, tinea, or allergic contact dermatitis. We present photosensitizers (e.g., furocoumarins). five patients with a sharply defined erythematous swollen Herein, we present five cases of phytophotodermatitis af- patch with bullae on both feet. They described soaking their ter soaking feet in fig leaves decoction. feet in a fig leaves decoction to treat their underlying derma- We present two purposes of this report: the first is to bring tologic diseases. Within 24 hours, all patients had a burning attention to this type of dermatitis. It is important for der- sensation in their feet, and erythema and edema had devel- matologists to recognize phytophotodermatitis as it may oped on the feet dorsa with exception of the portion of the sometimes be misdiagnosed as other skin conditions in- skin covered by the sandals. -

A Case of Squamous Cell Carcinoma of Skin Subsequent to Subcutaneous Foreign Body Mubashir S1, Anwar P2, Hassa I3, Arif T4
Vol. 12, No. 1, 2014 Case Report A Case of Squamous Cell Carcinoma of Skin Subsequent to Subcutaneous Foreign Body Mubashir S1, Anwar P2, Hassa I3, Arif T4 1Lecturer, 2Senior Resident, 3Professor and Head, Abstract 4Postgraduate scholar Squamous cell carcinoma (SCC) of the skin is one of the most Postgraduate Department of Dermatology, STD common non melanoma skin cancers (NMSC), along with basal cell & Leprosy, Govt. Medical College, Srinagar, J & carcinoma (BCC). Besides ultraviolet radiation, the role of exposure K , India. to industrial agents, ionizing radiation and areas of chronic inflammation is associated with the development of SCC. SCC may Address for correspondence also be associated with foreign bodies. We report a rare case of cutaneous SCC in an elderly Kashmiri female, developing subsequent Dr Parvaiz Anwar to subcutaneous non metallic foreign body, which was successfully excised with negative margins, and transposition flap closure. Senior Resident, Postgraduate Department of Dermatology, STD & Leprosy Key words: Squamous cell carcinoma, Foreign body, Transposition Govt. Medical College, Srinagar, J & K, India. flap closure E-mail: [email protected] Citation Mubashir S, Anwar P, Hassa I, Arif T. A case of squamous cell carcinoma of skin subsequent to subcutaneous foreign body. NJDVL 2014; 12(1): 53 - 55. Introduction lesion on left inner thigh. This was preceded, one Squamous cell and basal cell carcinoma are the month back, by a trivial trauma with penetration most important non melanoma skin cancers and of dry piece of broom. Like all Kashmiri exposure to ultraviolet radiation is the most population, she has been in the habit of using important risk factor for the development of these, Kangri for warmth for years together.