Heater-Associated Erythema Ab Igne: Case Report and Review of Thermal-Related Skin Conditions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Reticulate Hyperpigmentation of the Skin After Topical Application Of
Letters to the Editor 301 Reticulate Hyperpigmentation of the Skin After Topical Application of Benzoyl Peroxide Sir, Our two patients appeared to develop an irritant response on Benzoyl peroxide (BP) is an e¡ective and frequently used topical thetrunk afterapplication of 5% benzoyl peroxide. One medication for the treatment of acne vulgaris. It is a strong, patient applied BP to his face withnoirritation,consistentwith broad spectrum bactericidal agent that signi¢cantly decreases the ¢ndings of Hausteinetal.(3). Both patients then developed the number of Propionibacterium acnes in both the follicle and apattern of reticulate hyperpigmentation after their initial der- on surface skin (1). A common side e¡ect after usage is irritation matitis subsided. Biopsy in both cases was consistent with of the skin, usually manifested as a stinging or burning, and postin£ammatory hyperpigmentation. sometimes accompanied by erythema and scaling. Benzoyl per- Postin£ammatory hyperpigmentation develops after acute oxide is a strong irritant, but a weak allergen, rarely causing a or chronic in£ammation and trauma to the skin. The intensity contact dermatitis (2, 3). Tolerance can be achieved by gradually of the hypermelanosistendstobe more pronounced in darker- increasing the frequency of application over time. We describe skinnedindividuals. Other conditions that produce a pattern of two cases in which topical application of benzoyl peroxide reticulate hyperpigmentation include Riehl's melanosis, resulted in an unusual pattern of reticulate hyperpigmentation which is characterized by reticulate brown-black pigmenta- of the skin, most likely as a sequela of an irritant contact derma- tion of the face and neck. This is thought to be a result of a titis. -
Erythema Ab Igne and Use of Laptop Computers
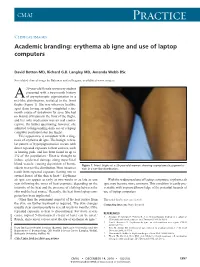
CMAJ Practice Clinical images Academic branding: erythema ab igne and use of laptop computers David Botten MD, Richard G.B. Langley MD, Amanda Webb BSc See related clinical image by Beleznay and colleagues, available at www.cmaj.ca 20-year-old female university student presented with a two-month history A of asymptomatic pigmentation in a net-like distribution, isolated to the front thighs (Figure 1). She was otherwise healthy, apart from having recently completed a six- month course of isotretinoin for acne. She had no history of trauma to the front of the thighs, and her only medication was an oral contra- ceptive. On further questioning, however, she admitted to longstanding daily use of a laptop computer positioned atop her thighs. This appearance is consistent with a diag- nosis of erythema ab igne. The benign, reticu- lar pattern of hyperpigmentation occurs with direct repeated exposure to heat sources, such as heating pads, and has been found in up to 3% of the population.1 Heat is thought to induce epidermal damage along superficial blood vessels, causing deposition of hemo- Figure 1: Front thighs of a 20-year-old woman showing asymptomatic pigmenta- siderin in a net-like distribution. Most instances tion in a net-like distribution. result from repeated exposure (lasting one to several hours) of the skin to heat.2,3 Erythema ab igne can appear as early as two weeks or as late as one With the widespread use of laptop computers, erythema ab year following the onset of heat exposure, depending on the igne may become more common. -

Erythema Ab Igne Erythema Ab Igne
gyöngyösi quark 10/18/13 8:48 Page 1 BÔRGYÓGYÁSZATI ÉS VENEROLÓGIAI SZEMLE • 2013 • 89. ÉVF. 5. 127–131. • DOI 10.7188/bvsz.2013.89.5.3 Erythema ab igne Erythema ab igne GYÖNGYÖSSY ORSOLYA DR., DARÓCZY JUDIT DR. Egyesített Szent István és Szent László Kórház – Rendelôintézet, Bôrgyógyászati Szakrendelô és Lymphoedema Rehabilitációs osztály, Budapest ÖSSZEFOGLALÁS SUMMARY Az erythema ab igne jelentése „bôrpír a tûztôl”. A bôr- Erythema ab igne means „redness from fire”. tünetek az ismétlôdô, 43-47 C fokos hôhatásra alakulnak Symptoms resulting from prolonged or repeated exposure ki. Régebben kályha, sugárzó hô okozta a tüneteket, újab- to moderate heat. The heat source used to be stove, and ban laptop, ágymelegítô hatása is bizonyított. A klinikai other infrared radiation, nowadays the role of laptop tüneteket retikuláris pigmentáció, petechiák, hólyagok, computer, hot blanket and many others are proved. The atypikus sebek jellemzik. Három észlelt esetben lehetôség clinical symptomes are reticular hyperpigmentation, volt az eltérô klinikai megjelenés bemutatására. A bôr petechia, blisters, aypical ulcers. Three different cases mikrocirkulációs zavara lézer-Doppler módszerrel igazol- show the variant clinical manifestation. Pathologic ható. A szerzôk elsôként vetik fel, hogy a bôrtünet kialaku- dermal microcirculation was verified with Laser Doppler lása a bôr kapillárisainak a hôhatásra adott kóros reak- examination. The authors first raised the relationship ciójával függhet össze. A ritkán diagnosztizált kórkép between abnormal capillary respond to heat and the onset felismerése azért fontos, mert az ismétlôdô vagy folyama- of skin symptoms. It is important to be familiar with this tos hám irritáció következtében elszarusodó laphámrák rarely diagnosed disease because the chronic epidermal keletkezhet és Merkel sejtes carcinomát is leírtak. -

What Is Acne? Acne Is a Disease of the Skin's Sebaceous Glands
What is Acne? Acne is a disease of the skin’s sebaceous glands. Sebaceous glands produce oils that carry dead skin cells to the surface of the skin through follicles. When a follicle becomes clogged, the gland becomes inflamed and infected, producing a pimple. Who Gets Acne? Acne is the most common skin disease. It is most prevalent in teenagers and young adults. However, some people in their forties and fifties still get acne. What Causes Acne? There are many factors that play a role in the development of acne. Some of these include hormones, heredity, oil based cosmetics, topical steroids, and oral medications (corticosteroids, lithium, iodides, some antiepileptics). Some endocrine disorders may also predispose patients to developing acne. Skin Care Tips: Clean skin gently using a mild cleanser at least twice a day and after exercising. Scrubbing the skin can aggravate acne, making it worse. Try not to touch your skin. Squeezing or picking pimples can cause scars. Males should shave gently and infrequently if possible. Soften your beard with soap and water before putting on shaving cream. Avoid the sun. Some acne treatments will cause skin to sunburn more easily. Choose oil free makeup that is “noncomedogenic” which means that it will not clog pores. Shampoo your hair daily especially if oily. Keep hair off your face. What Makes Acne Worse? The hormone changes in females that occur 2 to 7 days prior to period starting each month. Bike helmets, backpacks, or tight collars putting pressure on acne prone skin Pollution and high humidity Squeezing or picking at pimples Scrubs containing apricot seeds. -

Review Cutaneous Patterns Are Often the Only Clue to a a R T I C L E Complex Underlying Vascular Pathology
pp11 - 46 ABstract Review Cutaneous patterns are often the only clue to a A R T I C L E complex underlying vascular pathology. Reticulate pattern is probably one of the most important DERMATOLOGICAL dermatological signs of venous or arterial pathology involving the cutaneous microvasculature and its MANIFESTATIONS OF VENOUS presence may be the only sign of an important underlying pathology. Vascular malformations such DISEASE. PART II: Reticulate as cutis marmorata congenita telangiectasia, benign forms of livedo reticularis, and sinister conditions eruptions such as Sneddon’s syndrome can all present with a reticulate eruption. The literature dealing with this KUROSH PARSI MBBS, MSc (Med), FACP, FACD subject is confusing and full of inaccuracies. Terms Departments of Dermatology, St. Vincent’s Hospital & such as livedo reticularis, livedo racemosa, cutis Sydney Children’s Hospital, Sydney, Australia marmorata and retiform purpura have all been used to describe the same or entirely different conditions. To our knowledge, there are no published systematic reviews of reticulate eruptions in the medical Introduction literature. he reticulate pattern is probably one of the most This article is the second in a series of papers important dermatological signs that signifies the describing the dermatological manifestations of involvement of the underlying vascular networks venous disease. Given the wide scope of phlebology T and its overlap with many other specialties, this review and the cutaneous vasculature. It is seen in benign forms was divided into multiple instalments. We dedicated of livedo reticularis and in more sinister conditions such this instalment to demystifying the reticulate as Sneddon’s syndrome. There is considerable confusion pattern. -

What Is Acne and Why Do I Have Pimples?
What is acne and why do I have pimples? The medical term for “pimples” is acne. Most people develop at least some acne, especially during their teenage years. Although many believe that acne comes from being dirty, this is not true; rather, acne is the result of changes that occur during puberty. Your skin is made of layers. To keep the skin from getting dry, the skin makes oil in little wells called “sebaceous glands” that are found in the deeper layers of the skin. “Whiteheads” or “blackheads” are clogged sebaceous glands. “Blackheads” are not caused by dirt blocking the pores, but rather by oxidation (a chemical reaction that occurs when the oil reacts with oxygen in the air). People with acne have glands that make more oil and are more easily plugged, causing the glands to swell. Hormones, bacteria (called P. acnes) and your family’s likelihood to have acne (genetic susceptibility) also play a role. SKIN HYGIENE Good skin care habits are important and support the medications your doctor prescribes for your acne. » Wash your face twice a day, once in the morning and once in the evening (which includes any showers you take). » Avoid over-washing/over-scrubbing your face as this will not improve the acne and may lead to dryness and irritation, which can interfere with your medications. » In general, milder soaps and cleansers are better for acne-prone skin. The soaps labeled “for sensitive skin” are milder than those labeled “deodorant soap” or “antibacterial soap.” » Many “acne washes” may contain salicylic acid. Salicylic acid (SA) fights oil and bacteria mildly but can be drying and can add to irritation. -

Pattern of Skin Tumours in Kashmir Valley of North India: a Hospital Based Clinicopathological Study
International Journal of Information Research and Review, February 2015 International Journal of Information Research and Review Vol. 2, Issue, 02, pp. 376-381 February, 2015 Research Article PATTERN OF SKIN TUMOURS IN KASHMIR VALLEY OF NORTH INDIA: A HOSPITAL BASED CLINICOPATHOLOGICAL STUDY 1,*Peerzada Sajad, 2Iffat Hassan, 3Ruby Reshi, 4Atif Khan and 5Waseem Qureshi 1MBBS, MD Senior Resident, Postgraduate Department of Dermatology, GMC Srinagar, India 2Associate Professor and Head Postgraduate Department of Dermatology, STD and Leprosy GMC Srinagar, 3Associate professor and Head Postgraduate Department of Pathology GMC Srinagar, 4Scholar, PostgraduateIndia Department of Dermatology, STD and Leprosy GMC Srinagar, 5Chief physician and Registrar Academics, Government Medical College Srinagar, India India India ARTICLE INFO ABSTRACT Article History: Background: Earlier studies have shown that the incidence of all varieties of skin cancers is lower Received 27th November, 2014 among Indians due to the protective effects of melanin.However the pattern of skin cancers in kashmir Received in revised form valley is different from the rest of India due to the presence of Kangri cancer. 20th December, 2014 Objective: Our aim was to assess the distribution pattern of skin tumours among ethnickashmiri Accepted 30th January, 2015 population presenting to a tertiary care hospital in Kashmir and comparison of clinical diagnosis with st Published online 28 February, 2015 histopathological confirmation. Methods: This study was a prospective hospital based which was conducted over a one year period Keywords: on patients’ attending the outpatient department of Dermatology of our hospital and presenting with Non-Melanoma Skin Cancers, clinical features suspicious of benign or malignant skin tumours .All the relevant investigations Benign, including a skin biopsy were done in every individual patient to determine the type of tumour. -

Etiology, Classification, and Treatment of Urticaria
CONTINUING MEDICAL EDUCATION Etiology, Classification, and Treatment of Urticaria Kjetil Kristoffer Guldbakke, MD; Amor Khachemoune, MD, CWS GOAL To understand urticaria to better manage patients with the condition OBJECTIVES Upon completion of this activity, dermatologists and general practitioners should be able to: 1. Discuss the clinical classification of urticaria. 2. Recognize how to diagnose urticaria. 3. Identify treatment options. CME Test on page 50. This article has been peer reviewed and approved Einstein College of Medicine is accredited by by Michael Fisher, MD, Professor of Medicine, the ACCME to provide continuing medical edu- Albert Einstein College of Medicine. Review date: cation for physicians. December 2006. Albert Einstein College of Medicine designates This activity has been planned and imple- this educational activity for a maximum of 1 AMA mented in accordance with the Essential Areas PRA Category 1 CreditTM. Physicians should only and Policies of the Accreditation Council for claim credit commensurate with the extent of their Continuing Medical Education through the participation in the activity. joint sponsorship of Albert Einstein College of This activity has been planned and produced in Medicine and Quadrant HealthCom, Inc. Albert accordance with ACCME Essentials. Drs. Guldbakke and Khachemoune report no conflict of interest. The authors discuss off-label use of colchi- cine, cyclophosphamide, cyclosporine, dapsone, intravenous immunoglobulin, methotrexate, montelukast sodium, nifedipine, plasmapheresis, rofecoxib, sulfasalazine, tacrolimus, thyroxine, and zafirlukast. Dr. Fisher reports no conflict of interest. Urticaria is among the most common skin dis- autoimmune mechanisms are now recognized as a eases. It can be acute, chronic, mediated by a cause of chronic urticaria. A search of the PubMed physical stimulus, or related to contact with an database (US National Library of Medicine) for urticant. -

Local Heat Urticaria
Volume 23 Number 12 | December 2017 Dermatology Online Journal || Case Presentation DOJ 23 (12): 10 Local heat urticaria Forrest White MD, Gabriela Cobos MD, and Nicholas A Soter MD Affiliations: 1 New York University Langone Health, New York Abstract PHYSICAL EXAMINATION: A brisk, mechanical stroke elicited a linear wheal. Five minutes after exposure We present a 38-year-old woman with local heat to hot water, she developed well-demarcated, urticaria confirmed by heat provocation testing. Heat erythematous blanching wheals that covered the urticaria is a rare form of physical urticaria that is distal forearm and entire hand. triggered by exposure to a heat source, such as hot water or sunlight. Although it is commonly localized Conclusion and immediate, generalized and delayed onset forms Physical or inducible urticarias are a group of exist. Treatment options include antihistamines urticarias that are triggered by various external and heat desensitization. A brisk, mechanical stroke physical stimuli, such as mechanical stimuli, pressure, elicited a linear wheal. Five minutes after exposure cold, light, or temperature change. Urticarias due to hot water, she developed well-demarcated, to temperature change include heat urticaria (HU), erythematous blanching wheals that covered the cholinergic urticaria, and cold urticaria. distal forearm and entire hand. HU is a rare form of chronic inducible urticaria, with Keywords: urticaria, local heat urticaria, physical approximately 60 reported cases [1]. In HU, contact urticaria with a heat source such as hot water, sunlight, hot air, radiant heat, or hot objects results in wheal formation Introduction HISTORY: A 38-year-old woman presented to the Skin and Cancer Unit for the evaluation of recurrent, intensely pruritic eruptions that were precipitated by exposure to heat, which included hot water and sunlight. -

Edderm101 CORE DISEASES V2.09
ed.derm.101: core diseases almost everything you need to know to survive dermatology* “Two thirds of what we see is behind our eyes” “Explain, explain,” grumbled Étienne. “If you people can’t name something you’re incapable of seeing it.”— Cortázar, 1966, Hopscotch “Learning results from what the student does and thinks and only from what the student does and thinks. The teacher can advance learning only by influencing what the student does to learn.” Herbert Simon, Nobel Laureate. ! " *the first of many outright lies exaggerations. You need to know skincancer909 too, and ed.derm.101: core concepts, but these are also free. Professor Jonathan Rees FMedSci Grant Chair of Dermatology University of Edinburgh email me reestheskin.me: about me reestheskinblog.me: unreasonable views from the edge of education and medicine skincancer909: an online textbook of skin cancer for medical students V2.09, 25 September 2019 at 13:18 Distributed under a Creative Commons Attribution-Non Commercial ShareAlike 4.0 License !1 Preface The purpose of ed.derm.101: core diseases is to cover all the clinical material that we expect students to know, that is not covered in either ed.derm.101: core concepts or skincancer909. I assume you have already worked your way through ed.derm.101: core concepts (because what follows is heavily dependent on this foundational reading). A few words of advice about studying this aspect of dermatology and ed.derm.101: - It is hard to learn about a disease without some sort of mental image of what it looks like. In skincancer909 I was able to make use of a bespoke library of images that were developed as part of a research project funded by the Wellcome Trust. -

A Synopsis of Cancer
A SYNOPSIS OF CANCER GENESIS AND BIOLOGY BY WILFRED KARK M.B., B.Ch., F.R.C.S. Assistant Surgeon, Johannesburg Hospital; Lecturer in Clinical Surgery and Surgical Pathology, University of Witwatersr and; Lieut.-Col. R. A.M.C. ; Vice-President of the College of Physicians, Surgeons, and Gynaecologists of South Africa, and Chairman of its Examinations and Credentials Committee WITH A FOREWORD BY Sir ARTHUR PORRITT, Bt. K.C.M.G., K.C.V.O. .C.B.E., F.R.C.S. BRISTOL: JOHN WRIGHT & SONS LTD 1966 (§) JOHN WRIGHT & SONS LTD., 1966 Distribution by Sole Agents: United States of America: The Williams ώ Wilkins Company, Baltimore Canada: The Macmillan Company of Canada Ltd., Toronto PRINTED IN GREAT BRITAIN BY JOHN WRIGHT & SONS LTD., AT THE STONEBRIDGE PRESS, BRISTOL PREFACE THE disciplines involved in research into the genesis and biology of cancer are growing ever wider, and the detail of study is becoming increasingly deep. It is not surprising that the practitioner of medicine finds it difficult to maintain an appreciation of advances, and to co ordinate and apply the results of basic research to his own sphere of work. Not only does this imply the possibility of deficiencies in therapy, but it results in a serious and fundamental loss to the sum total of possible avenues of exploration of cancer. The lack of application and correlation of the results of investigation and experiment to the observa tion and management of patients suffering from cancer detracts from the practitioner's understanding of the disease and reduces his potential contribution to knowledge of the subject. -
Environmental Terminology in the Language Of
“Raindrops” describe the pattern of hypopigmented areas ENVIRONMENTAL TERMINOLOGY IN THE LANGUAGE OF DERMATOLOGY within larger areas of hyperpigmentation associated with Patricia Ting, BSc& Benjamin Barankin, MD arsenic -induced pigmentation Division of Dermatology and Cutaneous Sciences, University of Alberta, Edmonton, Alberta, Canada Background: Arsenic exposure often results in pigmentary changes (hyper- and/or hypopigmentation) and multiple punctate keratoses on the palms and soles. The latter may ABSTRACT develop into skin cancers (i.e. Bowen's, squamous cell, basal cell carcinoma). The source of inorganic arsenicals comes Communication in dermatology is based upon the accurate morphological description of cutaneous lesions. To facilitate this goal, dermatologists have adopted Multicentric reticulohistiocytosis (MRH) is a multi-system from agricultural, environmental (well water), industrial (glass interesting and descriptive terminology to portray dermatoses that are difficult to depict and visualize, including frequently e ncountered objects in nature disorder with distinct cutaneous lesions of 2 to 10 cm non- workers, miners), and medicinal (herbal) remedies. and natural phenomena. Many of these descriptions are able to effectively create rich visual imagery, and they are useful aids f or learning and recall. Many tender papules or nodules on the upper trunk and extremities, have stood the test of time. For example, varicella has been described as “dewdrops on a rose petal” and linear palmoplantar lesions of pachydermoperiotosis Pathophysiology : Arsenicals may increase susceptibility to hands and nail base that range in color from shades of yellow have been depicted as a “wind blown desert” of rippling sand. The “Christmas tree” pattern has been classically used to describe pityriasis rosea while the to red.