Dermatologic Conditions in Young Athletes Disclosures Objectives
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Reticulate Hyperpigmentation of the Skin After Topical Application Of
Letters to the Editor 301 Reticulate Hyperpigmentation of the Skin After Topical Application of Benzoyl Peroxide Sir, Our two patients appeared to develop an irritant response on Benzoyl peroxide (BP) is an e¡ective and frequently used topical thetrunk afterapplication of 5% benzoyl peroxide. One medication for the treatment of acne vulgaris. It is a strong, patient applied BP to his face withnoirritation,consistentwith broad spectrum bactericidal agent that signi¢cantly decreases the ¢ndings of Hausteinetal.(3). Both patients then developed the number of Propionibacterium acnes in both the follicle and apattern of reticulate hyperpigmentation after their initial der- on surface skin (1). A common side e¡ect after usage is irritation matitis subsided. Biopsy in both cases was consistent with of the skin, usually manifested as a stinging or burning, and postin£ammatory hyperpigmentation. sometimes accompanied by erythema and scaling. Benzoyl per- Postin£ammatory hyperpigmentation develops after acute oxide is a strong irritant, but a weak allergen, rarely causing a or chronic in£ammation and trauma to the skin. The intensity contact dermatitis (2, 3). Tolerance can be achieved by gradually of the hypermelanosistendstobe more pronounced in darker- increasing the frequency of application over time. We describe skinnedindividuals. Other conditions that produce a pattern of two cases in which topical application of benzoyl peroxide reticulate hyperpigmentation include Riehl's melanosis, resulted in an unusual pattern of reticulate hyperpigmentation which is characterized by reticulate brown-black pigmenta- of the skin, most likely as a sequela of an irritant contact derma- tion of the face and neck. This is thought to be a result of a titis. -
Erythema Ab Igne and Use of Laptop Computers
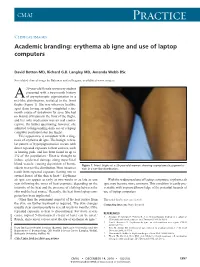
CMAJ Practice Clinical images Academic branding: erythema ab igne and use of laptop computers David Botten MD, Richard G.B. Langley MD, Amanda Webb BSc See related clinical image by Beleznay and colleagues, available at www.cmaj.ca 20-year-old female university student presented with a two-month history A of asymptomatic pigmentation in a net-like distribution, isolated to the front thighs (Figure 1). She was otherwise healthy, apart from having recently completed a six- month course of isotretinoin for acne. She had no history of trauma to the front of the thighs, and her only medication was an oral contra- ceptive. On further questioning, however, she admitted to longstanding daily use of a laptop computer positioned atop her thighs. This appearance is consistent with a diag- nosis of erythema ab igne. The benign, reticu- lar pattern of hyperpigmentation occurs with direct repeated exposure to heat sources, such as heating pads, and has been found in up to 3% of the population.1 Heat is thought to induce epidermal damage along superficial blood vessels, causing deposition of hemo- Figure 1: Front thighs of a 20-year-old woman showing asymptomatic pigmenta- siderin in a net-like distribution. Most instances tion in a net-like distribution. result from repeated exposure (lasting one to several hours) of the skin to heat.2,3 Erythema ab igne can appear as early as two weeks or as late as one With the widespread use of laptop computers, erythema ab year following the onset of heat exposure, depending on the igne may become more common. -

Review Cutaneous Patterns Are Often the Only Clue to a a R T I C L E Complex Underlying Vascular Pathology
pp11 - 46 ABstract Review Cutaneous patterns are often the only clue to a A R T I C L E complex underlying vascular pathology. Reticulate pattern is probably one of the most important DERMATOLOGICAL dermatological signs of venous or arterial pathology involving the cutaneous microvasculature and its MANIFESTATIONS OF VENOUS presence may be the only sign of an important underlying pathology. Vascular malformations such DISEASE. PART II: Reticulate as cutis marmorata congenita telangiectasia, benign forms of livedo reticularis, and sinister conditions eruptions such as Sneddon’s syndrome can all present with a reticulate eruption. The literature dealing with this KUROSH PARSI MBBS, MSc (Med), FACP, FACD subject is confusing and full of inaccuracies. Terms Departments of Dermatology, St. Vincent’s Hospital & such as livedo reticularis, livedo racemosa, cutis Sydney Children’s Hospital, Sydney, Australia marmorata and retiform purpura have all been used to describe the same or entirely different conditions. To our knowledge, there are no published systematic reviews of reticulate eruptions in the medical Introduction literature. he reticulate pattern is probably one of the most This article is the second in a series of papers important dermatological signs that signifies the describing the dermatological manifestations of involvement of the underlying vascular networks venous disease. Given the wide scope of phlebology T and its overlap with many other specialties, this review and the cutaneous vasculature. It is seen in benign forms was divided into multiple instalments. We dedicated of livedo reticularis and in more sinister conditions such this instalment to demystifying the reticulate as Sneddon’s syndrome. There is considerable confusion pattern. -

General Dermatology an Atlas of Diagnosis and Management 2007
An Atlas of Diagnosis and Management GENERAL DERMATOLOGY John SC English, FRCP Department of Dermatology Queen's Medical Centre Nottingham University Hospitals NHS Trust Nottingham, UK CLINICAL PUBLISHING OXFORD Clinical Publishing An imprint of Atlas Medical Publishing Ltd Oxford Centre for Innovation Mill Street, Oxford OX2 0JX, UK tel: +44 1865 811116 fax: +44 1865 251550 email: [email protected] web: www.clinicalpublishing.co.uk Distributed in USA and Canada by: Clinical Publishing 30 Amberwood Parkway Ashland OH 44805 USA tel: 800-247-6553 (toll free within US and Canada) fax: 419-281-6883 email: [email protected] Distributed in UK and Rest of World by: Marston Book Services Ltd PO Box 269 Abingdon Oxon OX14 4YN UK tel: +44 1235 465500 fax: +44 1235 465555 email: [email protected] © Atlas Medical Publishing Ltd 2007 First published 2007 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, without the prior permission in writing of Clinical Publishing or Atlas Medical Publishing Ltd. Although every effort has been made to ensure that all owners of copyright material have been acknowledged in this publication, we would be glad to acknowledge in subsequent reprints or editions any omissions brought to our attention. A catalogue record of this book is available from the British Library ISBN-13 978 1 904392 76 7 Electronic ISBN 978 1 84692 568 9 The publisher makes no representation, express or implied, that the dosages in this book are correct. Readers must therefore always check the product information and clinical procedures with the most up-to-date published product information and data sheets provided by the manufacturers and the most recent codes of conduct and safety regulations. -

Aswathy. P Aravind S, Ayurvedic Concept of Wellness
P a g e | 91 Editorial . International Research Journal of Ayurveda & Yoga An International Peer Reviewed Journal for Ayurveda & Yoga Management of Skin Allergy Due to Cosmetic Products -A Conceptual Study Dr. Monika Sharma 1 Dr. Rajveer Sason2, Dr. Sandeep Charak3 ICV-70.44- ISRA-1.318 VOLUME 4 ISSUE 4 1. Ph.D Scholar, P.G Department of Agad tantra Nia Jaipur Rajasthan. 2. Ph.D Scholar, P.G Department of Agad tantra Nia Jaipur Rajasthan. 3. Assistance Professor, Dept. of Agad Tantra, GAMC, Jammu & Kashmir. Corresponding Author :- Dr. Monika Sharma Ph.D Scholar, P.G Department of Agad tantra Nia Jaipur Rajasthan, Email: [email protected] Article received on 2nd April 2021 Article Accepted 20th April 2021 Article published 30th April 2021 ABSTRACT: - Beauty is a subject of social medical importance. Every person wants to stand at height and they require distinct personality which differ them from a crowd. People are using cosmetic products use for curing their skin problems and to maintain the skin appearance and beauty. Allergic reactions due to cosmetics may be delayed type reactions such as photo allergic contact dermatitis and immediate type reactions, that is contact dermatitis. Prick test is gold standard for diagnosis of allergy produce by cosmetic products. According to Ayurveda, if the body balance is maintained no allergic reactions are possible. All Skin disease have been described under Kustha (Psoriasis). Present paper highlights skin allergy produces by cosmetic products and its management through Ayurveda. Keywords-Skin allergy, Cosmetic product, Management This work is licensed under a creative attribution -Non-commercial-No derivatives 4.0 International License commons How to cite this article: - Dr. -

CSI Dermatology
Meagen M. McCusker, MD [email protected] Integrated Dermatology, Enfield, CT AbbVie - Speaker Case-based scenarios, using look-alike photos, comparing the dermatologic manifestations of systemic disease to dermatologic disease. Select the clinical photo that best matches the clinical vignette. Review the skin findings that help differentiate the two cases. Review etiology/pathogenesis when understood and discuss treatments. Case 1: Scaly Serpiginous Eruption This patient was evaluated for a progressively worsening pruritic rash associated with dyspnea on exertion and 5-kg weight loss. Despite its dramatic appearance, the patient reported no itch. KOH examination is negative (But, who’s good at those anyway?) A. B. Case 1: Scaly Serpiginous Eruption This patient was evaluated for a progressively worsening pruritic rash associated with dyspnea on exertion and 5-kg weight loss. Despite its dramatic appearance, the patient reported no itch. KOH examination is negative (But, who’s good at those anyway?) A. Correct. B. Tinea Corporis Erythema Gyratum Repens Erythema Gyratum Repens Tinea corporis Rare paraneoplastic T. rubrum > T. mentagrophytes phenomenon typically > M. canis associated with lung Risk factors cancer>esophageal and breast Close contact, previous cancers. infection, Less commonly associated with occupational/recreational connective tissue disorders such exposure, contaminated as Lupus or Rheumatoid furniture or clothing, Arthritis gymnasium, locker rooms “Figurate erythema” migrates up 1-3 week incubation → to 1 cm a day centrifugal spread from point of Resolves with treatment of the invasion with central clearing malignancy This patient was diagnosed with squamous cell carcinoma of the lung. Case 2: Purpuric Eruption on the Legs & Buttocks A 12-year old boy presents with a recent history of upper respiratory tract infection, fever and malaise. -

Canine Recurrent Flank Alopecia: a Synthesis of Theory and Practice
Vlaams Diergeneeskundig Tijdschrift, 2014, 83 Review 275 Canine recurrent flank alopecia: a synthesis of theory and practice Caniene recurrente flankalopecia: synthese van theorie en praktijk 1S. Vandenabeele, 1J. Declercq, 2H. De Cock, 1S. Daminet 1Department of Medicine and Clinical Biology of Small Animals, Ghent University, Belgium 2Veterinary Pathology Services/Medvet, Antwerpen, Belgium [email protected] A BSTRACT Canine recurrent flank alopecia is a non-inflammatory, non-scarring alopecia of unknown etiology and has a visually striking clinical presentation. Although this disease entity is relatively common in the northern hemisphere, there is only scant information in the literature regarding case descriptions. The aim of this article was to review the literature and to describe clinical presentations recognized in practice, which are not always extensively documented in the literature. SAMENVATTING Caniene recurrente flankalopecia wordt klassiek gekenmerkt door een niet-inflammatoire alopecia met onbekende etiologie. Deze dermatose wordt getypeerd door unieke huidsymptomen. Alhoewel de aandoening relatief frequent voorkomt in het noordelijk halfrond en dus ook in België, is er slechts beperkte informatie over te vinden in de literatuur. Het doel van dit overzichtsartikel is om enerzijds een samenvatting te geven van de literatuur en anderzijds de verschillende klinische presentaties die herkend worden in de dagelijkse praktijk maar niet vaak beschreven worden in de literatuur, te documenteren. INTRODUCTION and the different clinical presentations that are recog- nized in practice, but which are not extensively men- Canine recurrent flank alopecia (CRFA) is a visu- tioned in the literature. ally striking disease characterized by cyclic episodes of non-inflammatory hair loss (or coat changes) that can recur annually (Miller et al., 2013a). -

Canadian Clinical Practice Guideline on the Management of Acne (Full Guideline)
Appendix 4 (as supplied by the authors): Canadian Clinical Practice Guideline on the Management of Acne (full guideline) Asai, Y 1, Baibergenova A 2, Dutil M 3, Humphrey S 4, Hull P 5, Lynde C 6, Poulin Y 7, Shear N 8, Tan J 9, Toole J 10, Zip C 11 1. Assistant Professor, Queens University, Kingston, Ontario 2. Private practice, Markham, Ontario 3. Assistant Professor, University of Toronto, Toronto, Ontario 4. Clinical Assistant Professor, University of British Columbia, Vancouver, British Columbia 5. Professor, Dalhousie University, Halifax, Nova Scotia 6. Associate Professor, University of Toronto, Toronto, Ontario 7. Associate Clinical Professor, Laval University, Laval, Quebec 8. Professor, University of Toronto, Toronto, Ontario 9. Adjunct Professor, University of Western Ontario, Windsor, Ontario 10. Professor, University of Manitoba, Winnipeg, Manitoba 11. Clinical Associate Professor, University of Calgary, Calgary, Alberta Appendix to: Asai Y, Baibergenova A, Dutil M, et al. Management of acne: Canadian clinical practice guideline. CMAJ 2015. DOI:10.1503/cmaj.140665. Copyright © 2016 The Author(s) or their employer(s). To receive this resource in an accessible format, please contact us at [email protected]. Contents List of Tables and Figures ............................................................................................................. v I. Introduction ................................................................................................................................ 1 I.1 Is a Clinical Practice Guideline -

Skin of Color
Dermatology Patient Education Skin of Color There are a variety of skin, hair and nail conditions that are common in people with skin of color such as African Americans, Asians, Latinos and Native Americans. Your dermatologist can help diagnose and treat these skin conditions. SKIN CONDITIONS Postinflammatory hyperpigmentation (PIH) This condition results in patches of darker skin as your skin heals after a cut or scrape, or when acne, eczema or other rashes clear. PIH often fades, but the darker the PIH, the longer fading can take. Your dermatologist can help restore your skin’s color more quickly. Prescription medicines containing retinoids or hydroquinone (a bleaching ingredient), and procedures such as chemical peels and microdermabrasion may help. Your dermatologist will also encourage you to wear sunscreen to avoid further darkening of the skin due to ultraviolet (UV) light exposure and prevent further PIH from developing. Treatment products available over-the-counter rarely help and can make PIH more noticeable. Melasma This common condition causes brown to gray-brown patches, usually on the face. It occurs most often in women who have Latina, African, or Asian ancestry. Men can get melasma, too. Melasma can also appear on other parts of the body that get lots of sun exposure, such as the forearms and neck. Melasma may be associated with pregnancy, birth control pills or estrogen replacement therapy. It may also be hereditary. Melasma can fade on its own, but it often recurs. Your dermatologist can provide prescription topical treatment to help the condition fade. Procedures including chemical peels and microdermabrasion can also help. -
Copyrighted Material
1 Index Note: Page numbers in italics refer to figures, those in bold refer to tables and boxes. References are to pages within chapters, thus 58.10 is page 10 of Chapter 58. A definition 87.2 congenital ichthyoses 65.38–9 differential diagnosis 90.62 A fibres 85.1, 85.2 dermatomyositis association 88.21 discoid lupus erythematosus occupational 90.56–9 α-adrenoceptor agonists 106.8 differential diagnosis 87.5 treatment 89.41 chemical origin 130.10–12 abacavir disease course 87.5 hand eczema treatment 39.18 clinical features 90.58 drug eruptions 31.18 drug-induced 87.4 hidradenitis suppurativa management definition 90.56 HLA allele association 12.5 endocrine disorder skin signs 149.10, 92.10 differential diagnosis 90.57 hypersensitivity 119.6 149.11 keratitis–ichthyosis–deafness syndrome epidemiology 90.58 pharmacological hypersensitivity 31.10– epidemiology 87.3 treatment 65.32 investigations 90.58–9 11 familial 87.4 keratoacanthoma treatment 142.36 management 90.59 ABCA12 gene mutations 65.7 familial partial lipodystrophy neutral lipid storage disease with papular elastorrhexis differential ABCC6 gene mutations 72.27, 72.30 association 74.2 ichthyosis treatment 65.33 diagnosis 96.30 ABCC11 gene mutations 94.16 generalized 87.4 pityriasis rubra pilaris treatment 36.5, penile 111.19 abdominal wall, lymphoedema 105.20–1 genital 111.27 36.6 photodynamic therapy 22.7 ABHD5 gene mutations 65.32 HIV infection 31.12 psoriasis pomade 90.17 abrasions, sports injuries 123.16 investigations 87.5 generalized pustular 35.37 prepubertal 90.59–64 Abrikossoff -

International Journal of Scientific Research
ORIGINAL RESEARCH PAPER Volume-9 | Issue-1 | January-2020 | PRINT ISSN No. 2277 - 8179 | DOI : 10.36106/ijsr INTERNATIONAL JOURNAL OF SCIENTIFIC RESEARCH TYPES AND VARIANTS OF ACNE Dermatology Shailee Patel ABSTRACT Acne occur when pores of skin are blocked with oil, dead skin, or bacteria. It can occur when excessive oil is produced by follicles, bacteria build up in pores, and dead skin cells accumulate in pores. All these problem contribute in development of pimple. Acne are majorly seen among teenagers but they can also occur in adults. There are varying from of acne, and their varying treatment. KEYWORDS 1.INTRODUCTION ulcerative colitis and Crohn's disease and syndromes, such as Acne is linked to the change in hormone level during puberty. Acne is a synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) and disorder that is seen worldwide. Acne is a disease of the teenagers but pyogenic arthritis, pyoderma gangrenosum, and acne (PAPA) can be seen even in newborn children and also adults. Age and gender syndromes. also play a very important role in onset of acne. Acne most commonly occur between the ages of 10-13 years. Girls have an earlier onset 3.4 Occupational Acne which easily contribute to the onset of puberty in girls than in boys. The Occupational acne is defined as development of acne-like lesions after disease severity in more in boys during the late adolescence. Acne exposure to occupational agents in persons not prone to develop acne mostly develops on areas of skin that have abundant oil glands, like the and who have not had acne before engaging in the said occupation. -

Importance of a Thorough Physical Examination! Muhammad Imran, M.D., Julian Magadan III, M.D., Mehrdad Maz, M.D
Kansas Journal of Medicine 2015 Physical Examination Importance of a Thorough Physical Examination! Muhammad Imran, M.D., Julian Magadan III, M.D., Mehrdad Maz, M.D. University of Kansas Medical Center Department of Internal Medicine Division of Allergy, Clinical Immunology, & Rheumatology Kansas City, KS A 73-year-old white female presented for management of her tophaceous gout, pyoderma gangrenosum, and chronic back pain. On exam, there was an incidental finding of reticular, reddish-brown, non-tender, macular, non-blanching discoloration on her entire back, with a few superficial erosions (see Figure). The patient did not know the duration of her rash. It was neither pruritic nor painful. She denied arthralgia, fever, chills, or other constitutional symptoms. She did not have a history of insect bites, recent foreign travel, falls, or trauma. She frequently used a heating pad to alleviate her chronic back pain. Complete blood count, comprehensive metabolic panel, urine analysis, and inflammatory markers were within normal limits. What is most likely diagnosis? A. Vasculitis B. Livedo Reticularis C. Erythema Ab Igne D. Cutaneous Lupus E. Actinic Keratosis 48 Kansas Journal of Medicine 2015 Physical Examination Correct Answer: C. Erythema Ab Igne Erythema ab igne (EAI), also known as ephelis ignealis or toasted skin syndrome, is an unintentional, unperceived, and self-induced condition, which occurs in individuals who persistently use topical or conventional heat to relieve localized pain or cold.1 It is characterized by chronic, localized, erythematous or hyper-pigmented, reticulated, and net-like skin patches in the affected area. It is usually asymptomatic, but burning and pruritus are reported by some patients.