Diagnostic Criteria for Neuromuscular Disorders 2Nd Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, the General Infirmary, Leeds
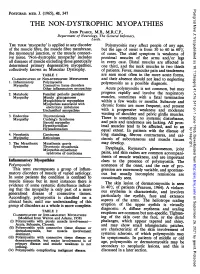
Postgrad Med J: first published as 10.1136/pgmj.41.476.347 on 1 June 1965. Downloaded from POSTGRAD. MED. J. (1965), 41, 347 THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, The General Infirmary, Leeds. THE TERM 'myopathy' is applied to any disorder Polymyositis may affect people of any age, of the muscle fibre, the muscle fibre membrane, but the age of onset is from 30 to 60 in 60% the myoneural junction, or the muscle connect- of cases. The chief symptom is weakness of ive tissue. 'Non-dystrophic myopathy' includes proximal muscles of the arms and/or legs all diseases of muscle excluding those genetically in every case. Distal muscles are affected in determined primary degenerative myopathies, one third, and the neck muscles in two thirds collectively known as Muscular Dystrophy. of patients. Fever, muscular pain and tenderness TABLE 1 are seen most often in the more acute forms, CLASSIFICATION OF NON-DYSTROPHIC MYOPATHIES and their absence should not lead to neglecting 1. Inflammatory Polymyositis as a Myopathy Connective tissue disorders polymyositis possible diagnosis. Other inflammatory mvopathies Acute polymyositis is not common, but may 2. Metabolic Familial periodic paralysis progress rapidly and involve the respiratory Myopathy Muscle glycogenoses muscles, sometimes with a fatal termination Myoglobinuric myopathies within a few weeks or months. Myopathies associated with Subacute and electrolyte imbalance chronic forms are more frequent, and present Unclassified myopathies with a progressive weakness and moderate of shoulder 3. Endocrine Thyrotoxicosis wasting and pelvic girdle muscles. Myopathy Cushing's Syndrome There is sometimes no systemic disturbance, Steroid myopathy and pain and tenderness are lacking. -

Disease Mutations in the Ryanodine Receptor N-Terminal Region Couple to a Mobile Intersubunit Interface
ARTICLE Received 1 Oct 2012 | Accepted 15 Jan 2013 | Published 19 Feb 2013 DOI: 10.1038/ncomms2501 OPEN Disease mutations in the ryanodine receptor N-terminal region couple to a mobile intersubunit interface Lynn Kimlicka1, Kelvin Lau1, Ching-Chieh Tung1 & Filip Van Petegem1 Ryanodine receptors are large channels that release Ca2 þ from the endoplasmic and sar- coplasmic reticulum. Hundreds of RyR mutations can cause cardiac and skeletal muscle disorders, yet detailed mechanisms explaining their effects have been lacking. Here we compare pseudo-atomic models and propose that channel opening coincides with widen- ing of a cytoplasmic vestibule formed by the N-terminal region, thus altering an interface targeted by 20 disease mutations. We solve crystal structures of several disease mutants that affect intrasubunit domain–domain interfaces. Mutations affecting intrasubunit ionic pairs alter relative domain orientations, and thus couple to surrounding interfaces. Buried disease mutations cause structural changes that also connect to the intersubunit contact area. These results suggest that the intersubunit contact region between N-terminal domains is a prime target for disease mutations, direct or indirect, and we present a model whereby ryanodine receptors and inositol-1,4,5-trisphosphate receptors are activated by altering domain arrangements in the N-terminal region. 1 Department of Biochemistry and Molecular Biology, Life Sciences Institute, University of British Columbia, Vancouver, British Columbia, Canada V6T 1Z3. Correspondence and requests for materials should be addressed to F.V.P. (email: fi[email protected]). NATURE COMMUNICATIONS | 4:1506 | DOI: 10.1038/ncomms2501 | www.nature.com/naturecommunications 1 & 2013 Macmillan Publishers Limited. All rights reserved. -

Central Core Disease - a Case Report
The Korean Journal of Pathology 2004; 38: 68-71 Central Core Disease - A Case Report - Ji Hoon Kim∙Young S. Park Central core disease is a rare autosomal dominantly inherited non-progressive congenital myopa- Sung-Hye Park∙Je G. Chi thy, which is pathologically characterized by the formation of a ‘‘core’’. We report a 28-year-old female with non-progressive muscle weakness, who had a hypotonic posture at birth. The devel- Department of Pathology, Seoul National opmental milestones were delayed with her first walking at 18 months of age. She could not University College of Medicine, Seoul, run or walk a long distance and weight-bearing tasks were almost impossible. None of her Korea family members showed motor symptoms. An investigation of the electromyography and nerve conduction velocity showed non-specific results. A gastrocnemius muscle biopsy revealed Received : November 14, 2003 central cores in approximately 70% of myofibers with a type 1 myofiber predominance and Accepted : January 7, 2004 deranged sarcolemmal structures. To the best of our knowledge, this is the fifth report of cen- tral core disease in the Korean literature. Corresponding Author Sung-Hye Park, M.D. Department of Pathology, Seoul National University College of Medicine, 28 Yongon-dong, Chongno-gu, Seoul 110-799, Korea Tel: 02-740-8278 Fax: 02-765-5600 E-mail: [email protected] Key Words : Myopathy, Central Core-Muscle, Skeletal-Ultrastructure Central core disease is a form of congenital non-progressive right upper extremity. The symptoms were relieved with the help myopathy, which was first described by Shy and Magee in 1956. -

Central Core Disease in Focus
Central Core Disease In Focus Fast Facts Central core disease (CCD) is a genetic muscle disease characterized by the appearance of corelike struc- tures running through the centers of muscle fibers. The cores are areas of metabolic inactivity. Symptoms vary widely in sever- ity and can begin anywhere from infancy to adulthood. They include weakness, muscle cramps, orthope- dic abnormalities (spinal curvature, foot deformities, hip dislocations) caused by the weakness, and a dan- gerous susceptibility to malignant hyperthermia, an adverse reaction to anesthesia. The disease is usually dominantly In Focus inherited, meaning only one gene mutation, inherited from one parent, CCD: A Disease with Many Faces is necessary to cause symptoms. by Margaret Wahl The underlying molecular cause of the disease is an abnormality of orty-one-year-old Sandy Doak remem- since Doak is 5 feet tall and weighs 128 calcium release from deep inside Fbers that she was never athletic, pounds, the test result said her body was the muscle fibers. Normally, a signal couldn’t do sit-ups, and always had trou- 38 percent fat. There was only one way from a nerve fiber tells a muscle fiber ble finishing physical tasks. But, she says, that could be the case, the fitness expert to contract and, after a cascade of “I never really thought I had anything and she agreed: She had very little mus- events, calcium is released in a burst wrong. I just thought I was awkward. I cle. For Doak, it was a clue that something from internal storage areas. Calcium knew I was weaker than others. -

Neurological Diseases Caused by Ion-Channel Mutations Frank Weinreich and Thomas J Jentsch*
409 Neurological diseases caused by ion-channel mutations Frank Weinreich and Thomas J Jentsch* During the past decade, mutations in several ion-channel humans. This is probably the case for important Na+-chan- genes have been shown to cause inherited neurological nel isoforms, such as those dominating excitation in diseases. This is not surprising given the large number of skeletal muscle or heart, and may also be the case for the different ion channels and their prominent role in signal two channel subunits that assemble to form M-type processing. Biophysical studies of mutant ion channels in vitro K+-channels, which are key regulators of neuronal allow detailed investigations of the basic mechanism excitability [8••,9•]. This concept is supported by the underlying these ‘channelopathies’. A full understanding of observation that many channelopathies are paroxysmal these diseases, however, requires knowing the roles these (i.e. cause transient convulsions): mutations leading to a channels play in their cellular and systemic context. Differences constant disability might be incompatible with life, or may in this context often cause different phenotypes in humans and significantly decrease the frequency of the mutation with- mice. The situation is further complicated by the developmental in the human population. In contrast to the severe effects and other secondary effects that might result from ion- symptoms associated with the loss of function of certain channel mutations. Recent studies have described the different key ion channels, the large number of ion-channel isoforms thresholds to which ion-channel function must be decreased in may lead to a functional redundancy under most circum- order to cause disease. -

Supplementary Information
Supplementary Information Structural Capacitance in Protein Evolution and Human Diseases Chen Li, Liah V T Clark, Rory Zhang, Benjamin T Porebski, Julia M. McCoey, Natalie A. Borg, Geoffrey I. Webb, Itamar Kass, Malcolm Buckle, Jiangning Song, Adrian Woolfson, and Ashley M. Buckle Supplementary tables Table S1. Disorder prediction using the human disease and polymorphisms dataseta OR DR OO OD DD DO mutations mutations 24,758 650 2,741 513 Disease 25,408 3,254 97.44% 2.56% 84.23% 15.77% 26,559 809 11,135 1,218 Non-disease 27,368 12,353 97.04% 2.96% 90.14% 9.86% ahttp://www.uniprot.org/docs/humsavar [1] (see Materials and Methdos). The numbers listed are the ones of unique mutations. ‘Unclassifiied’ mutations, according to the UniProt, were not counted. O = predicted as ordered; OR = Ordered regions D = predicted as disordered; DR = Disordered regions 1 Table S2. Mutations in long disordered regions (LDRs) of human proteins predicted to produce a DO transitiona Average # disorder # disorder # disorder # order UniProt/dbSNP Protein Mutation Disease length of predictors predictors predictorsb predictorsc LDRd in D2P2e for LDRf UHRF1-binding protein 1- A0JNW5/rs7296162 like S1147L - 4 2^ 101 6 3 A4D1E1/rs801841 Zinc finger protein 804B V1195I - 3* 2^ 37 6 1 A6NJV1/rs2272466 UPF0573 protein C2orf70 Q177L - 2* 4 34 3 1 Golgin subfamily A member A7E2F4/rs347880 8A K480N - 2* 2^ 91 N/A 2 Axonemal dynein light O14645/rs11749 intermediate polypeptide 1 A65V - 3* 3 43 N/A 2 Centrosomal protein of 290 O15078/rs374852145 kDa R2210C - 2 3 123 5 1 Fanconi -

Chapter 23 PATHOPHYSIOLOGY of MUSCLE DISORDERS LINKED TO
Chapter 23 PATHOPHYSIOLOGY OF MUSCLE DISORDERS LINKED TO MUTATIONS IN THE SKELETAL MUSCLE RYANODINE RECEPTOR Robert T. Dirksen1 and Guillermo Avila2 1 Dept. of Pharmacology and Physiology, University of Rochester Medical Center, Rochester, USA; 2 Dept. of Biochemistry, Cinvestav-IPN, Mexico City, Mexico INTRODUCTION Skeletal muscle excitation contraction (EC) coupling involves a unique, bi-directional mechanical interaction between two different types of calcium channels: a sarcolemmal voltage-gated L-type calcium channel (dihydropyridine receptor, DHPR) and the ryanodine receptor (RyR1), a ligand-gated intracellular release channel located in the sarcoplasmic reticulum (SR) (see Dirksen852 for review). In response to sarcolemma depolarization, the DHPR undergoes a conformational change that results in activation of nearby RyR1 release channels and subsequent massive release of SR into the myoplasm (see Melzer et al.169 for review). Thus, the DHPR and RyR1 proteins are essential components of the EC coupling machinery in skeletal muscle, and thus, play a central role in muscle homeostasis. Not surprisingly, mutations and/or deletions in the genes that encode the skeletal muscle DHPR and RyR1 proteins are linked to at least five different human diseases: Malignant hyperthermia (MH), hypokalemic periodic paralysis, central core disease (CCD), multiminicore disease (MmD) and nemaline rod myopathy (NM). Mutations in RyR1 result in MH, CCD, MmD and NM, whereas DHPR mutations are linked only to MH and hypokalemic periodic paralysis. The genetic bases of these diseases, as well as the cellular mechanisms involved, have been thoroughly reviewed elsewhere.853,854 This chapter will focus on the clinical manifestations and functional defects associated with human RyR1 disease mutations and how 230 Chapter 23 these defects might contribute to the pathophysiology of the skeletal muscle ryanodinopathies. -

General Disease Finder
General Disease Finder This overview will help to fi nd neuromuscular disease patterns in the different sections Cushing’s disease, steroid myopathy; Addison’s disease, general muscle weakness Adrenal dysfunction Periodic paralysis Aldosteronism Tetanic muscles CN: VII AIDS Polyneuropathies: infl ammatory, immune mediated, treatment related Myopathies: infl ammatory, treatment related Neoplastic: lymphoma (direct invasion) Opportunistic infections: CMV, toxoplasmosis, Cryptococcus , HSV Candida, Varicella, Histoplasma, TBC, Aspergillus CMV polyradiculomyelopathy Herpes zoster radiculitis Syphilitic radiculopathy Treatment related: polyneuropathy/myopathy Ddl, ddC, foscarnet, isoniazid Zidovudine Polyneuropathy (distal, rarely proximal) Alcohol Mononeuropathy – radial nerve (compression) Myopathy Acute necrotizing myopathy and myoglobinuria Chronic proximal weakness Hypokalemic paralysis Myoglobinuria Compartment syndromes (prolonged compression) Familial amyloid polyneuropathies Amyloid Transthyretin Neuropathy Sensorimotor neuropathy Autonomic (continued) E.L. Feldman et al., Atlas of Neuromuscular Diseases, 299 DOI 10.1007/978-3-7091-1605-0, © Springer-Verlag Wien 2014 300 General Disease Finder Autonomic involvement Primary/secondary Apolipoprotein A-1 Polyneuropathy, painful, hearing loss Gelsolin type V, VII, and other CN Mild polyneuropathy Primary amyloidosis (AL) Deposition of immunoglobulin light chains in tissue Adrenal dysfunction Aldosteronism AIDS Alcoholism Amyloid Painful neuropathy Autonomic involvement Carpal tunnel syndrome -

Rg Dg15 Rg16
CALENDAR YEAR(s): 2016,2017,2018,2019 AUSTRALIA Clayton - Monash University Peter David Currie PhD RG Using zebrafish congenital muscular dystrophy models to find novel therapies. $100,000.00 8/1/2015 7/31/2016 Year 1 $100,000.00 8/1/2016 7/31/2017 Year 2 $100,000.00 8/1/2017 7/31/2018 Year 3 Summary Numerous studies have suggested that zebrafish genetic models of human diseases can recapitulate many aspects of the human pathology. This is particularly well documented for muscle wasting diseases where a number of genetic models of human muscular dystrophies have been identified by our laboratory. Specific to the aims of this project was the identification of a zebrafish mutation in the Laminin alpha 2 gene which is mutated in the most common form of congenital muscular dystrophy (CMD). We have used this zebrafish model to make observations on the mechanisms by why muscle cells die when they lack Laminin alpha2 protein. We now wish to understand this process better and will use the specific advantages of the zebrafish system to make observations that will lead to the identification of novel therapeutic approaches for the treatment of CMD. We have also developed methods to screen the zebrafish model of CMD to identify novel drug compounds and we will use these methods to find drugs that prevent the onset and progression of muscle waiting in this model. We hope these compounds will form the basis for the development of drugs to treat congenital muscular dystrophy. Tamar Esther Sztal Ph.D DG15 Evaluating therapies to improve muscle function in nemaline myopathy $60,000.00 2/1/2016 1/31/2017 Year 1 $60,000.00 2/1/2017 1/31/2018 Year 2 $60,000.00 2/1/2018 1/31/2019 Year 3 Summary Nemaline myopathies are congenital muscle diseases causing severe muscle weakness and low muscle tone. -

Structure and Function of the Human Ryanodine Receptors and Their Association with Myopathies—Present State, Challenges, and Perspectives
molecules Review Structure and Function of the Human Ryanodine Receptors and Their Association with Myopathies—Present State, Challenges, and Perspectives Vladena Bauerová-Hlinková * , Dominika Hajdúchová † and Jacob A. Bauer Institute of Molecular Biology, Slovak Academy of Sciences, Dúbravská Cesta 21, 845 51 Bratislava, Slovakia; [email protected] (D.H.); [email protected] (J.A.B.) * Correspondence: [email protected]; Tel.: +421-2-5930-7439 † Current address: Department of Pathological Physiology, Jessenius Faculty of Medicine in Martin, Comenius University in Bratislava, Malá Hora 4C, 036 01 Martin, Slovakia. Academic Editor: Jacopo Sgrignani and Giovanni Grazioso Received: 31 July 2020; Accepted: 30 August 2020; Published: 4 September 2020 Abstract: Cardiac arrhythmias are serious, life-threatening diseases associated with the dysregulation of Ca2+ influx into the cytoplasm of cardiomyocytes. This dysregulation often arises from dysfunction of ryanodine receptor 2 (RyR2), the principal Ca2+ release channel. Dysfunction of RyR1, the skeletal muscle isoform, also results in less severe, but also potentially life-threatening syndromes. The RYR2 and RYR1 genes have been found to harbor three main mutation “hot spots”, where mutations change the channel structure, its interdomain interface properties, its interactions with its binding partners, or its dynamics. In all cases, the result is a defective release of Ca2+ ions from the sarcoplasmic reticulum into the myocyte cytoplasm. Here, we provide an overview of the most frequent diseases resulting from mutations to RyR1 and RyR2, briefly review some of the recent experimental structural work on these two molecules, detail some of the computational work describing their dynamics, and summarize the known changes to the structure and function of these receptors with particular emphasis on their N-terminal, central, and channel domains. -

Myotubular/Centronuclear Myopathy and Central Core Disease
Review Article Myotubular/centronuclear myopathy and central core disease Chieko Fujimura-Kiyono, Gabor Z. Racz, Ichizo Nishino Department of Neuromuscular Research, National Institute of Neuroscience, National Center of Neurology and Psychiatry, 4-1-1 Ogawahigashi-Cho Kodaira, Tokyo 187-8502, Japan The term congenital myopathy is applied to muscle disorders Despite their genetic heterogeneity, the clinical presenting with generalized muscle weakness and hypotonia features have some characteristics in common. Main from early infancy with delayed developmental milestones. symptoms are generalized muscle weakness and The congenital myopathies have been classiÞ ed into various hypotonia, typically presenting at birth or in infancy. The categories based on morphological Þ ndings on muscle biopsy. clinical severity is highly variable from a mild, almost Although the clinical symptoms may seem homogenous, the asymptomatic form, to a severe form characterized by genetic basis is remarkably variable. This review will focus marked hypotonia at birth. Muscle weakness can be on myotubular myopathy, centronuclear myopathy, central very subtle in childhood and thus can only present core disease, and congenital neuromuscular disease with during adult years. Dysmorphic facies is very common uniform Type 1 Þ ber, myopathies that are subjects of our due to facial muscle involvement, and when this does ongoing examinations. occur, the onset is thought to be in utero. High arched palate is often documented in almost all patients with Key words: Central core disease, centronuclear myopathy, this disease. Scoliosis and contracture of joints are congenital myopathy, congenital neuromuscular disease with seen early in childhood, especially in infantile or child uniform Type 1 Þ bers, myotubular myopathy onset form. -

The Channelopathies: Novel Insights Into Molecular and Genetic Mechanisms of Human Disease
The channelopathies: novel insights into molecular and genetic mechanisms of human disease Robert S. Kass J Clin Invest. 2005;115(8):1986-1989. https://doi.org/10.1172/JCI26011. Review Series Introduction Ion channels are pore-forming proteins that provide pathways for the controlled movement of ions into or out of cells. Ionic movement across cell membranes is critical for essential and physiological processes ranging from control of the strength and duration of the heartbeat to the regulation of insulin secretion in pancreatic β cells. Diseases caused by mutations in genes that encode ion channel subunits or regulatory proteins are referred to as channelopathies. As might be expected based on the diverse roles of ion channels, channelopathies range from inherited cardiac arrhythmias, to muscle disorders, to forms of diabetes. This series of reviews examines the roles of ion channels in health and disease. Find the latest version: https://jci.me/26011/pdf Review series introduction The channelopathies: novel insights into molecular and genetic mechanisms of human disease Robert S. Kass Department of Pharmacology, Columbia University Medical Center, New York, New York, USA. Ion channels are pore-forming proteins that provide pathways for the controlled movement of ions into or out of cells. Ionic movement across cell membranes is critical for essential and physiological processes ranging from control of the strength and duration of the heartbeat to the regulation of insulin secretion in pancreatic β cells. Diseases caused by mutations in genes that encode ion channel subunits or regulatory proteins are referred to as channelopathies. As might be expected based on the diverse roles of ion channels, channelopathies range from inherited cardiac arrhythmias, to muscle disorders, to forms of diabetes.